Author Details :
Volume : 5, Issue : 1, Year : 2019
Article Page : 54-60
https://doi.org/10.18231/2581-4729.2019.0013
Abstract
Introduction: Tinea Pedis (T. Pedis) and toe nail Onychomycosis is a chronic relapsing superficial fungal infection, often associated with that of other cutaneous areas. Dermatophytes are the commonest organisms in T. Pedis and Onychomycosis, Trichophyton Rubrum (T. Rubrum) being the commonest isolate. The causative species may be different from place to place, so it is important to have a knowledge about the dermatophytes causing T. Pedis and Onychomycosis in a particular area, so that specific agents are used for effective treatment, and prevent drug resistance.
Aims: Study morphological patterns of T. Pedis and toe nail Onychomycosis and find causative fungal species.
Material and Methods: Prospective hospital based study over 1 year period, on clinically diagnosed cases of T. Pedis and toe nail Onychomycosis, confirmed by positive results on microscopic examination of KOH preparation. Culture was done to isolate the specific pathogen involved.
Results: Out of 150 patients, 60 (40%) had T. Pedis alone, 34 (22.7%) Toe nail Onychomycosis alone and 56 (37.3%) both T. Pedis and Onychomycosis in the same patient. On culture, 56 patients out of 150 (37.3%) showed a positive fungal growth. 30 out of 56 patients (53.3%) of mixed T. Pedis and Onychomycosis were positive. 16 out of 60 patients (26.7%) of T. Pedis and 10 out of 34 (29.4%) Onychomycosis patients respectively were culture positive.
Conclusion: Among all the clinically diagnosed and KOH positive patients, culture positivity was established in 56 (37.3%) patients only, T. Rubrum being the most common fungal strain, followed by T. Mentagrophyte.
Keywords: Tinea pedis, Onychomycosis, Fungal culture, Trichophyton rubrum, Trichophyton mentagrophyte.
Tinea Pedis is a common relapsing superficial fungal infection of the feet, affecting 10-15% of population worldwide, with four main clinical variants which include chronic intertriginous type (also known as ‘Athlete’s foot’); chronic papulosquamous type; vesicular/ vesicobullous type and acute ulcerative type.[1] Most common causative species of T. Pedis have been found to be anthropophilic dermatophytes especially Trichophyton rubrum, Trichophyton mentagrophtes and Epidermophyton floccosum.[2] Trichophyton tansurans has also been implicated in children.
Onychomycosis denotes fungal infection of nail plate of toes caused by different species of dermatophytes, yeasts and non–dermatophyte fungi and is one of the commonest nail disorders, accounting for about 30% of superficial fungal infections of skin. Main clinical patterns of dermatophytic Onychomycosis are Distal or lateral subungual Onychomycosis (DLSO); Total dystrophic subungual Onychomycosis (TDO); Proximal Subungual Onychomycosis (PSO); Superficial white Onychomycosis (SWO).[3],[4][5],[6],DLSO is the most common pattern. PSO is the least common pattern seen predominantly in immune compromised patients such as those with HIV and AIDS.[4],[7]
Trichophytons and Epidermophytons are the common species of dermatophytes affecting toe nails. In addition, a number of various opportunistic non-dermatophyte moulds colonise the feet and nails primarily damaged by trauma or some other dermatoses.[8],[9]
The prevalence of Tinea Pedis and Onychomycosis of toes are determined by various predisposing factors, such as age, socio-economic status; occupation; climate; living condition; sharing of bathing facilities at sports clubs and swimming pools; wearing of occlusive shoes and clothing; frequent travels and population shifts, along with immunosuppression, local trauma and impaired circulation.
The clinical diagnosis of Tinea Pedis and Onychomycosis can be confirmed by direct microscopy of potassium hydroxide (KOH) preparation. Fungal culture is necessary to identify the specific genus and species of pathogen, as clinical appearance caused by one species of fungus is indistinguishable from that caused by any other species.[10] Sabouraud's dextrose agar being one of the most commonly used mediums.
The etiological role of a particular dermatophyte in Tinea Pedis and Onychomycosis depends upon its ecological distribution and infection by the same pathogen at any other body site. If a particular dermatophyte is prevalent in a given area it is likely to be the most common cause of fungal infection in that area. The causative species may be different from place to place. So it is important to have a knowledge about the dermatophytes causing Tinea Pedis and Onychomycosis in a particular area, so that specific agents are used for effective treatment and prevent drug resistance.
We undertook this study at two centres simultaneously, a tertiary centre and a secondary referral centre, to evaluate the patterns of Tinea Pedis and toe nail Onychomycosis, and find out the causative organisms in this part of the World.
It was a prospective hospital based clinical study carried out over a period of 1 year at 2 centres simultaneously, one a tertiary centre and other a secondary referral centre. Clinically suspected patients of Tinea Pedis and toe nail Onychomycosis, microscopically proven to be positive for fungal elements were taken up for study after proper informed consent. Patients with history of any oral medication for any skin diseases for last 3 months and topical application for last 1 month were excluded.
Besides collection of demographic data, a detailed history of every patient was recorded in a format particularly with reference to duration of illness, occupation, hobbies and recreational activities, type of foot wear, contact with pets and cattle, fungal infection elsewhere on the body, presence of fungal infection in other family members, significant drug intake and co-morbid condition.
In addition to general physical and systemic examination, a detailed mucocutaneous examination of feet, toe nails and rest of the body was conducted by the same dermatologists and recorded in the format.
Specimen collection for microscopic examination of KOH preparation as well as for fungal culture was done as per the standard procedure.
Only KOH positive sample were inoculated into two to three sets of culture media, such as Sabourand`s dextrose agar (SDA) with chloramphenicol; SDA with chloramphenicol and cycloheximide; Dermatophyte test medium (DTM). Each set of media was incubated at room temperature and 370c and examined for any growth of fungi for 4 weeks. Minimal culture time to call it negative was 21 days.
Statistical analysis of the data was done with the help of computer software M S Excel of windows. Descriptive characteristics have been presented with the help of summary measures like mean; standard deviation and qualitative variable have been presented as percentages.
The study was conducted on 150 prospective patients of T.Pedis and toe nail Onychomycosis, who visited the outpatient department of our respective hospitals.
In this study, Patients ranged from 2-71 years of age with mean age at presentation 35.4 years. Most of the patients were in the age group 21-40 years followed by 41-60 years, and males outnumbered females. Various demographic and other variables are presented in summarized form in table 1.
Table 1: various demographic and other variables of the.
|
Variable |
|
|
|
|
Age group (years) |
Males |
Females |
Number & (%) |
|
?20 |
12 |
4 |
16 (10.9) |
|
21-40 |
74 |
22 |
96 (64.3) |
|
41-60 |
24 |
10 |
34 (22) |
|
? 61 |
4 |
0 |
4 (2.8) |
|
Total |
114 (76) |
36 (24) |
150 |
|
Residential status |
|
|
|
|
|
Rural |
|
87 (58) |
|
|
Urban |
|
63 (42) |
|
|
Total |
|
150 |
|
Type of disease |
|
|
|
|
|
T. Pedis |
|
60 (40) |
|
|
Both T. Pedis & toe nail Onychomycosis |
|
56 (37.3) |
|
|
Onychomycosis |
|
34 (22.7) |
|
Coexisting fungal infection |
|
|
|
|
|
T. Cruris |
|
20 (62.5) |
|
|
T. Corporis |
|
6 (18.8) |
|
|
T. Manum |
|
2 (6.2) |
|
|
T. Cruris & T. Manum |
|
4 (12.5) |
|
|
Total |
|
32 |
Associated comorbid systemic diseases were found in 10 patients, 5 with diabetes mellitus and hypertension in 5, already on treatment and under control.
Various morphological patterns of T.Pedis and toe nail Onychomycosis are shown in table 2.
Table 2: Morphological patterns of T. Pedis and toe nail Onychomycosis.
|
T. Pedis |
No Of patients |
Onychomycosis |
No Of patients |
|
Intertriginous type |
54 (46.5) |
DLSO |
45 (50) |
|
Squamous hyperkerototic type |
51 (44) |
TDO |
22 (24.4) |
|
Intertriginous & Squamous hyperkerototic type |
9 (7.8) |
DLSO & TDO |
18 (20) |
|
Vesico or vesicobullous types |
2 (1.7) |
SWO |
3 (3.3) |
|
|
|
DLSO & SWO |
2 (2.2) |
|
|
|
PSO |
0 |
|
Total |
116 |
|
90 |
Out of all the 150 KOH positive patients, 56 patients (37.3%) showed a positive fungal growth on culture. Among 56 patients of mixed Tinea Pedis and Onychomycosis, 30 (53.6%) were positive. Likewise among
60 patients of isolated T. Pedis and 34 with Onychomycosis, 16 (26.7%) and 10 (29.4%) respectively showed positive culture results. The results are summarized in table 3.
Table 3: Isolation of fungal strains on culture of the patient samples
|
Type of infection |
No. of patients (n=150) |
No. of patients positive on SDA |
Percentage |
|
Tinea Pedis and Onychomycosis |
56 |
24+6*=30 |
53.6% |
|
Tinea Pedis |
60 |
14+2*=16 |
26.7% |
|
Onychomycosis |
34 |
8+2*=10 |
29.4% |
|
Total |
150 |
56 |
37.3% |
|
*non dermatophyte isolates on culture media |
|||
T. Rubrum alone was isolated in 28 positive culture results and associated with A. Niger in 2 isolates. Out of these, 14 culture isolates had mixed T.Pedis and Onychomycosis, 10 had T.Pedis only and 4 had Onychomycosis only.
T. Mentagrophytes was isolated alone in 18 culture results and in association with A. Niger in 2. Out of these, 10 culture isolates had mixed T.Pedis and Onychomycosis, and 4 each had T.Pedis and Onychomycosis alone.
Growth of A. Niger and Candida albicans in isolation was found in 2 cases each. This is summarized in table 4.
Table 4: Distribution of fungal species in culture positive patients.
|
Isolate |
TP & O* |
TP* |
O* |
Total |
Percentage |
|
T. Rubrum |
14 |
10 |
4 |
28 |
50% |
|
T. Mentagrophyte |
10 |
4 |
4 |
18 |
32.1% |
|
T. Rubrum & A. Niger |
- |
2 |
- |
2 |
3.5% |
|
T. Mentagrophyte & A.niger |
2 |
- |
- |
2 |
3.5% |
|
A.niger |
- |
- |
2 |
2 |
3.5% |
|
Candida albicans |
2 |
- |
- |
2 |
3.6% |
|
Pencillinum spp. |
1 |
- |
- |
1 |
1.8% |
|
Fusarium |
1 |
- |
- |
1 |
1.8% |
|
Total |
30 |
16 |
10 |
56 |
100% |
|
*TP & O= Tinea Pedis & Onychomycosis; TP= Tinea Pedis; O= Onychomycosis |
|||||
In squamous hyperkeratotic and intertriginous types of Tinea Pedis, T. Rubrum was the most common isolate
(57.5%), followed by T. Mentagrophyte (35%), as summarized in table 5.
Table 5: Fungal species in relation to morphological patterns of T. Pedis
|
Causative fungus |
Sq. Keratotic |
Intertriginous |
Intertriginous & sq. Keratotic |
Total |
|
T. Rubrum |
14 |
7 |
2 |
23 |
|
T. Mentagrophyte |
10 |
4 |
0 |
14 |
|
T. Rubrum & A. Niger |
0 |
1 |
1 |
2 |
|
T. Mentagrophyte & A. Niger |
1 |
0 |
0 |
1 |
T. Rubrum was most commonly isolated (27%) from DLSO Onychomycosis pattern. T. Mentagrophyte was equally isolated from cases of DLSO, TDO and mixed DLSO/ TDO (11% each). Both cases of C. albicans had DLSO morphological type. A.niger was isolated from 2 cases each with DLSO and TDO, as shown in table 6.
Table 6: Fungal species in relation to morphological types of onychomycosis.
|
Causative fungus |
DLSO |
TDO |
DLSO & TDO |
SWO |
DLSO & SWO |
PSO |
|
T. Rubrum |
10 |
3 |
2 |
0 |
0 |
0 |
|
T. Mentagrophyte |
4 |
4 |
4 |
1 |
1 |
0 |
|
A. Niger |
2 |
2 |
0 |
0 |
0 |
0 |
|
C. Albicans |
2 |
0 |
0 |
0 |
0 |
0 |
|
Fusarium |
1 |
0 |
0 |
0 |
0 |
0 |
|
Pencillinium |
1 |
0 |
0 |
0 |
0 |
0 |
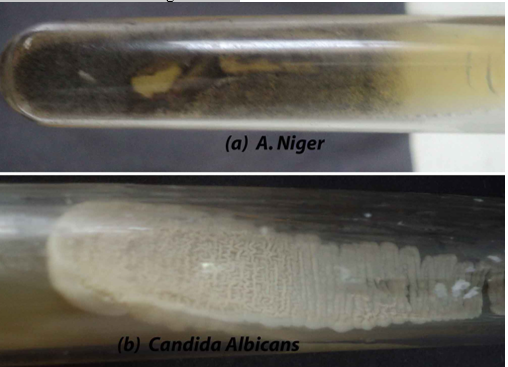
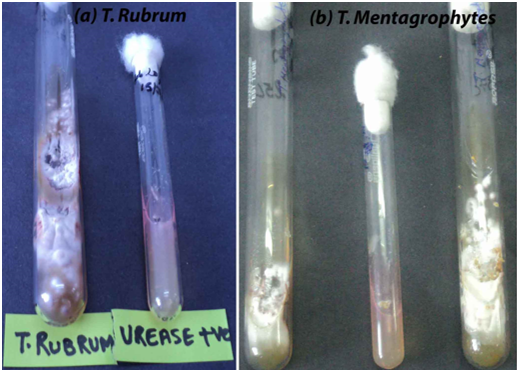
ome of the culture positive results are shown in fig. 1 and 2.
 |
Click here to view |
Fig. 1: Growth of A. Niger (a) and Candida (b) on culture.
 |
Click here to view |
Fig. 2: Growth of T. Rubrum (a) and T. Mentagrophytes (b) on culture.
Discussion
In this study, most of the patients were in the age group 21-40 years followed by 41-60 years. Lesser prevalence was found in ?20 year age group and least prevalence in ?61 year age group. These findings are consistent with the previous studies from around the world, justifying the statement that Tinea Pedis and Onychomycosis is generally a disease of adults and uncommon in children and elderly.[4],[11],[12],[13],[14],[15],[16],[17],[18],[19][20]
A high prevalence of Tinea Pedis and Onychomycosis in patients above 55 years was found in some previous studies in contrast to ours.[14],[21],[22],[23] The actual incidence of Tinea Pedis and Onychomycosis may, in fact, be higher in elderly group in our country, because it is very difficult for elderly to seek medical consultation at hospital, as they are dependent upon others to visit the hospital. The low prevalence of Tinea Pedis and Onychomycosis in children is attributed to difference in nail plate structure, a lack of cumulative trauma, lack of occlusive foot wear and increased growth rate of nail plate with subsequent elimination of fungus.[24]
In our study, Tinea Pedis and Onychomycosis were found to be more common in males than females, similar to the observations in various previous studies.[2],[3],[13],[17],[18],[23],[25],[26],[27],[28],[29]In contrast, high incidence in
females has been reported in some studies.[7],[20],[24],[30],[31] Candidial Onychomycosis has been reported to be more common in females in most of the previous studies.[2],[3],[9],[20],[24]In our study also, both of the 2 cases of candidal toe nail Onychomycosis were females. Lesser incidence of Tinea Pedis and Onychomycosis in females reported in literature may not be true in real sense, as the disease being often asymptomatic is not reported as frequently as in males.[18][23]
More number of patients from rural areas than the urban is in proportion to the overall more rural population. Again rural population having farming as main occupation and also chances of more contact with cattle are more liable to get fungal infections.
Occupations which predispose the patient to micro trauma and injuries lead to overall more chances of Tinea Pedis and Onychomycosis.[3],[8],[9],[13],[32]These include farmers, labourers and defence personnel, which comprised respectively 4%, 6% and 13.3% of all the patients. However, history of obvious trauma preceding the Tinea Pedis and Onychomycosis may not be always given, for example, only 3 patients in our study. In our study, service class being the most common patient group, 35 patients out of 150, may be attributed to more awareness among these, along with easy accessibility to hospital, hence reported more.
Tinea Pedis and Onychomycosis has asymptomatic and indolent course as observed by other workers.[11] ,[20],[24],[26],[33]In our study also, disease duration of more than 6 months at the time of presentation was found in 88 (75.7%) cases of Tinea Pedis and 86 (95.6%) cases of Onychomycosis.
Animals may be a source of fungal infections in rural areas,[34] and in our study also history of contact with cattle and pets was present in 29 (19.3%) patients, although there was no history suggestive of infection in these animals.
Warm and moist environment provided by occlusive footwear promotes growth of fungus and predisposes to Tinea Pedis and Onychomycosis, as observed in previous studies.[6],[8],[21],[23],[35]Similarly, majority of patients in our study had the habit of wearing occlusive shoes and socks.
Distal and lateral subungual Onychomycosis (DLSO) was the commonest type (50%) encountered in our study, consistent with observations in previous studies.[20],[29]The reason behind this is that the initial site of invasion is usually the free edges, followed by involvement of hyponychium and later nail bed and nail plate at distal and lateral end.
In this study 24.5% of the cases had total dystrophic Onychomycosis (TDO) and 20% had both DLSO and TDO in the same patient. Number of cases of TDO was more as compared to some of the previous studies.[17][19],[29],[35]
Proximal subungual Onychomycosis (PSO), which may be a sign of immunodeficiency, has been very rare variety in previous studies.[3][9],[10],[7],[22],[36] It was not present in any of our patients as well.
In our study, 56 out of 150 patients had both Tinea Pedis and toe nail Onychomycosis in the same patient. Tinea Pedis infection preceded the nail involvement in 28 (50%) patients and followed it in 16 (28.5%) patients, whereas in 12 (21.5%) patients there was simultaneous involvement of skin and nails. From this we can infer that though transmission of infection between skin and nail is a two way process, yet Tinea Pedis mostly precedes Onychomycosis, because hard difficult-to-dissolve keratinous structure and low nutrient supply of nails do not provide favourable environment for establishment of fungus than the skin, but once established it acts as reservoir for constant source of infection for other parts of the body.[8][11],[32]
In our study, dermatophytes were isolated in 46 out of 56 culture positive results (82.14%) and most of these were positive within first two weeks of inoculation. These observations show that dermatophytes are the main etiological agents causing Tinea Pedis and Onychomycosis, a fact established by previous studies as well.[9],[12],[27],[35]
Generally, there is always a difficulty in isolating the fungi on culture from the nail material. One of the reasons may be the non-viability of fungal hyphae in the distal portion of the nail plate from where the samples are usually taken.[3],[4],[8],[9],[18],[20]
The most common isolate obtained in our study was T. Rubrum (50%), which has been reported as most prevalent pathogen in Tinea Pedis and Onychomycosis in previous studies also.[2] [7],[9],[12],[13],[17],[18],[22],[23],[26],[27][35] T. Rubrum can colonize easily on stratum corneum and hard keratin, so it has greater capacity to infect the skin and nails of the feet than any other dermatophyte.[8],[22]
T. Mentagrophyte was the second most common isolate in our study (32.3%). Similar observations were made in previous studies also.[2] [9],[13],[17],[18],[29]T. Mentagrophyte has been reported as the most common isolate in some other studies.[2],[37]
In our study, there were 2 (3.5%) culture positive candida albicans species and these patients had chronic paronychia and nail involvement. The isolation rates of yeasts from the nails have been highly variable. Among all the yeasts, candida species are the most frequently reported ones.[3],[20],[24],[35]
Non-dermatophytes were isolated in 8 cases (14.2%) and 6 of them were Aspergillus species, of which 2 cases of Tinea Pedis had mixed culture of A. niger and T. Rubrum. It may be presumed that T. Rubrum was the primary pathogen and moulds secondarily infected the damaged nail. Aspergillus species has also been reported in earlier studies.[9],[17],[19],[22],Other isolates in our study were Penicillinum and Fusarium. Onychomycosis caused by non-dermatophytes are often associated with that caused by dermatophytes. Non-dermatophyte Onychomycosis is usually confined to toe nails and often asymptomatic, which may be the reason for its low incidence due to under reporting.[32]
In our study T. Rubrum was the most common isolate in squamous hyperkeratotic and intertriginous types of Tinea Pedis, followed by T. Mentagrophyte in both groups, similar to previous reported studies.[2],[28]
T. Rubrum was found to be the commonest cause of DLSO and TDO in our study. DLSO is the commonest type of nail dystrophy and is usually caused by T. Rubrum.[9],[17]
Conflict of Interest: None.
Financial Support: None.
Although all the 150 clinically diagnosed cases with Tinea Pedis and Toe nail Onychomycosis alone or in combination pattern, were selected for the study after establishing KOH positivity for fungal elements in all the cases, yet the culture results for fungal growth correlated in 56 (37.3%) patients only. Among these 53.3% (30 out of 56) patients with both Tinea Pedis and Onychomycosis, 26.7% (16 out of 60) with Tinea Pedis only and 29.4% (10 out of 34) with Onychomycosis only were culture positive. The most frequent growth obtained was that of T. Rubrum which was isolated in 28 out of 56 (50%) patients, followed by T. Mentagrophyte, isolated in 18 (32.1%) cases. Nail plate biopsy followed by periodic acid-Schiff staining should be the most accurate method for diagnosing fungal elements in Onychomycosis, but this facility was not available in our laboratory.
How to cite : Bhatti R, Rather P A, Dogra D, Gupta V, Mahajan B, Clinico-Mycological study of tinea pedis and toe nail onychomycosis: A multi-center study from Jammu. IP Indian J Clin Exp Dermatol 2019;5(1):54-60
This is an Open Access (OA) journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
Viewed: 1852
PDF Downloaded: 589