- Visibility 181 Views
- Downloads 17 Downloads
- DOI 10.18231/j.ijced.2020.012
-
CrossMark
- Citation
A clinical and dermatoscopic study of melasma
- Author Details:
-
Akbar Ali Shanavaz
-
Meghana Bathina
-
Vishal B Amin *
-
Malcolm Pinto
-
Manjunath Shenoy M
Introduction
Melasma is an acquired hypermelanosis of uncertain etiology that occurs exclusively in sun-exposed area mostly on face and rarely on the neck and forearms.[1] It is more common in women and in Asians. Exact pathogenesis remains elusive, however, genetic predisposition and ultraviolet light exposure seem to play an important role.[2] Diagnosis of melasma remains clinical and aided by Wood’s lamp examination; the latter has also been questioned in the recent past.[3] Melasma needs to be differentiated from other causes of facial hypermelanoses, such as pigmented contact dermatitis, lichen planus pigmentosus, and erythema dyschromicum perstans. Histopathology is not performed routinely for diagnosis of facial hypermelanoses because of reluctance on part of the patient and physician alike as there is a risk of development of unsightly scar/postinflammatory dyschromia. Dermatoscopy is increasingly being used for diagnosis of pigmentary disorders other than malignancy.[4] There are only a few studies till date on dermatoscopic patterns in melasma in Indian patients. The aim of the study is to characterize the clinical and dermatoscopic pattern of melasma, so as to allow early diagnosis of melasma and differentiate it from other facial hypermelanoses. These findings also provide new avenues for research into better understanding and treating this challenging condition.
Hydroquinone (HQ) and Triple combination creams (TCCs) remain the gold standard of treatment. Various botanical extracts that have been tried in melasma are grape seed extract, pycnogenol, aloesin, green tea extracts, coffee berry, soy, and licorice extract.[5]
Materials and methods
Source of data collection
The study will be conducted in the Dermatology department of Yenepoya Medical College and Hospital on 110 patients during the period of December 2016 to June 2018. Clinical examination includes standard dermatological examination along with Wood’s lamp and dermatoscopic examination (Detailed format attached).
We used Heine Delta 20 plus Dermatoscope for evaluation of Melasma.
Method of data collection
All male and female patients with melasma attending the out-patient clinic of the department of Dermatology, Venereology and Leprosy at Yenepoya Medical College, Mangalore were included in the study after obtaining written, informed consent.
Details of clinical examination
The study involved clinical evaluation of melasma which was documented photographically. Dermatoscopic examination was done to assess the area of involvement and to grade melasma according to the MASI (Melasma Area and Severity Index). Wood’s lamp examination was performed to analyze the degree of extent of melasma based on depth of involvement.
Inclusion criteria
All consenting male and female patients with clinical diagnosis of melasma attending the outpatient clinic.
Exclusion criteria
Patients who have taken any treatment for melasma within a period of past 3 months.
Sample size calculation
Sample size is calculated using G* lower software n=110 minimum sample, with level of significance alpha = 5%, power = 80 % Effective size= 0.27.
Results
Age Distribution: Out of 110 cases, the maximum incidence was noted in the age group 31-40 years and minimum in the age group above 50 years of age. There were 39(35.5%) patients in age group 31-40 and only 13(11.8%) above the age of 50 years([Table 1]).
Sex distribution
Out of 110 patients 76(69.1%) were female and 34(30.9%) were male showing the involvement of females were more than double that in males ([Table 2]).
Distribution based on Fitzpatrick skin type
Out of 110 patients 99(90%) had Fitzpatrick skin type IV, followed by Fitzpatrick skin type V in 6(5.5%) patients and Fitzpatrick skin type III in 5(4.5%) patients ([Table 3]).
Distribution based on occupation
Out of 110 patients it was found out that housewives constituted the majority 66(60%) patients followed by farmers/labourers making for 28(25.5%)patients, employees 10(9.1%) patients, business men 4(3.6%) and others making 2(1.8%) of the total ([Table 4]).
Distribution based on the clinical type of melasma
Out of 110 cases it was found out that 65(59.1%) of the patients had a centrofacial pattern ([Figure 1]), 44(40%) patients had a malar pattern followed by only 1(0.9%)patient with a mandibular pattern ([Table 5]).
Distribution based on Family history
Out of 110 cases, only 4(3.6%) of patients gave a positive family history of melasma where as the remaining 106(96.4%) of patients were negative for the same ([Table 6]).
Distribution based on Drug history
Out of 110 cases 2(1.80%) gave a positive history of OCP intake whereas the remaining 108(98.20%) were negative for the same ([Table 7]).
Distribution based on menstrual history
Out of 110 cases, 48(43.63%) patients had regular cycles. Six (5.45%) had irregular cycles, 23 (20.9%) of the cases had attained menopause and the rest 33(30%) of the patients were males ([Table 8]).
Distribution based on Melasma Area Severity Index(MASI)
Out of 110 cases, patients with Moderate MASI 73(66.4%) comprised of the majority, followed by 34(30.9%) patients with a mild MASI score. Only 3(2.7%) patients had a severe MASI score ([Table 9]).
Distribution based on Wood's Lamp Examination
Out of 110 cases Patchy enhancement ([Figure 2]) was seen in 62(56.4%) patients is suggestive of a mixed type of melasma. This was followed by enhancement seen in 40(36.4%) of the patients. Only 8(7.3%) of patients showed no enhancement indicating Dermal type of melasma ([Table 10]).
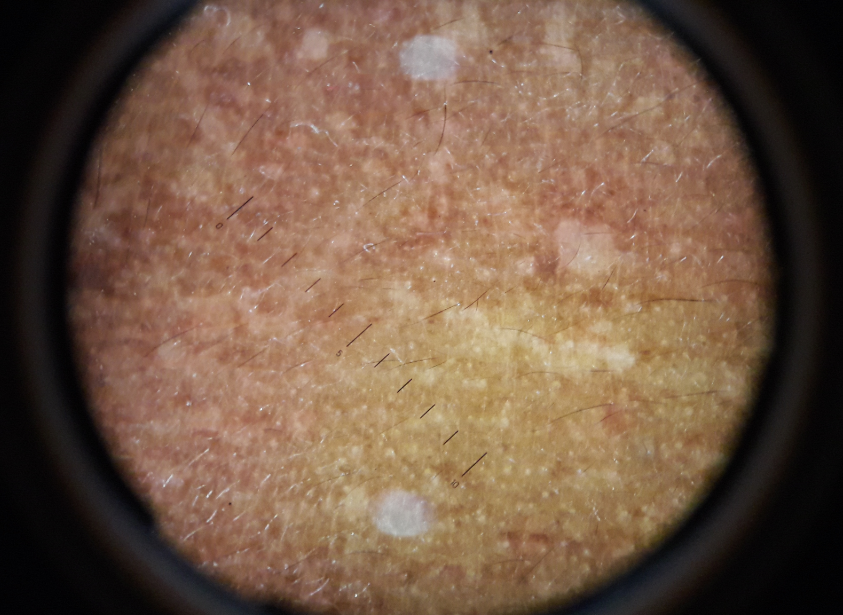
Distribution based on Dermatoscopic patterns
In 110 cases it was found out that 94(85.45%) of the cases had a reticuloglobular pattern ([Figure 3]) under dermatoscopy. In 110 cases it was found out that only 30(27.3%) of patients had granules/dots under dermatoscopy.
In 110 cases it was found out that 50(45.54%) patients had a perifollicular brown black globules under dermatoscopy
Out of 110 cases 21(19.1%) patients had an unpatterned pigmentation distribution under dermatoscopy ([Table 11]).
Additional findings under Dermatoscopy
Out of 110 cases, only 40(36%) of the patients had telangiectasia ([Figure 4]) on Dermatoscopy.
Out of 110 cases, 27(24.5%) patients showed depigmentation suggestive of topical treatment taken for Melasma.([Table 12]).
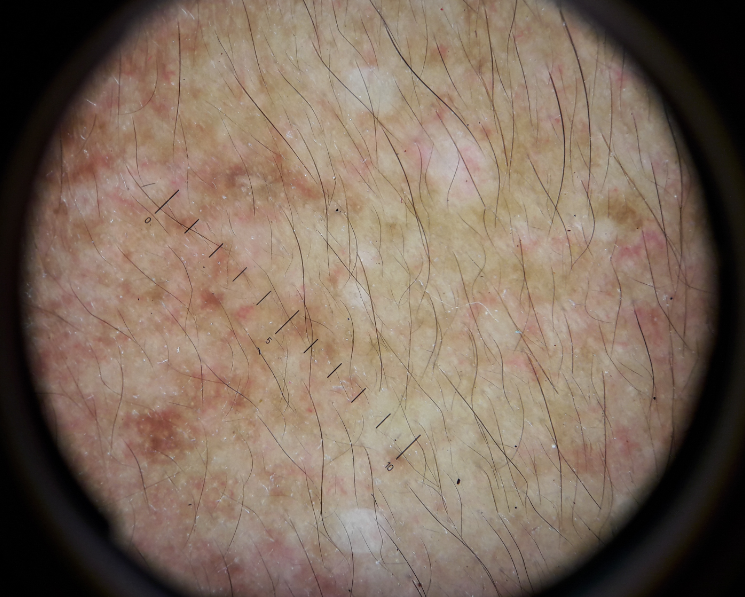
Type of melasma under Dermatoscopy
Out of 110 cases, 71(64.5%) patients had Epidermal type Melasma ([Figure 5]) followed by a mixed type in 33(30%) of the patients. However only 6(5.5%) patients had a Dermal type of melasma ([Table 13]).



| Frequency | Percent | |
| 20 - 30 | 24 | 21.8 |
| 31 - 40 | 39 | 35.5 |
| 41 - 50 | 34 | 30.9 |
| Above 50 | 13 | 11.8 |
| Total | 110 | 100.0 |
| Count | Column N % | ||
| Sex | F | 76 | 69.1% |
| M | 34 | 30.9% | |
| Total | 110 | 100.0% |
| Fitzpatrick skin type | III | 5 | 4.5% |
| IV | 99 | 90.0% | |
| V | 6 | 5.5% | |
| Total | 110 | 100.0% |
| Occupation | business | 4 | 3.6% |
| Employees | 10 | 9.1% | |
| farmer/Labourer | 28 | 25.5% | |
| housewife | 66 | 60.0% | |
| Other | 2 | 1.8% | |
| Total | 110 | 100.0% |
| CF | Present | 65 | 59.1% |
| Absent | 45 | 40.9% | |
| Total | 110 | 100.0% | |
| Malar | Present | 44 | 40.0% |
| Absent | 66 | 60.0% | |
| Total | 110 | 100.0% | |
| M | Present | 1 | 0.90% |
| Absent | 109 | 99.09% | |
| Total | 110 | 100.0% |
| Family history | Present | 4 | 3.6% |
| Absent | 106 | 96.4% | |
| Total | 110 | 100.0% |
| Drug history | Present | 2 | 1.8% |
| Absent | 108 | 98.2% | |
| Total | 110 | 100.0% |
| Menstrual history | Regular | 48 | 43.63% |
| Irregular | 6 | 5.45% | |
| Menopause | 23 | 20.9% | |
| NA | 33 | 30.0% |
| MASI | Mild | 34 | 30.9% |
| Moderate | 73 | 66.4% | |
| Severe | 3 | 2.7% | |
| Total | 110 | 100.0% |
| Woods lamp | No enhancement seen | 8 | 7.3% |
| Enhancement seen | 40 | 36.4% | |
| Patchy enhancement seen | 62 | 56.4% | |
| Total | 110 | 100.0% |
| Reticuloglobular pattern | Present | 94 | 85.45% |
| Absent | 16 | 14.54% | |
| Total | 110 | 100.0% | |
| Granules/dots | Present | 30 | 27.3% |
| Absent | 80 | 72.7% | |
| Total | 110 | 100.0% | |
| Perifollicular brown black globules | Present | 50 | 45.45% |
| Absent | 60 | 54.54% | |
| Total | 110 | 100.0% | |
| Unpatterned patchy Pigmentation | Present | 21 | 19.1% |
| Absent | 89 | 80.9% | |
| Total | 110 | 100.0% |
| Telangiectasia | Present | 40 | 36.4% |
| Absent | 70 | 63.6% | |
| Total | 110 | 100.0% | |
| Depigmentation | Present | 27 | 24.5% |
| Absent | 83 | 75.5% | |
| Total | 110 | 100.0% | |
| Ochronosis | Present | 0 | .0% |
| Absent | 110 | 100.0% | |
| Total | 110 | 100.0% |
| Types of melasma based on dermatoscopy | 0 | 6 | 5.5% |
| 1 | 71 | 64.5% | |
| 2 | 33 | 30.0% | |
| Total | 110 | 100.0% |
Discussion
A total of 110 patients with clinical diagnosis of psoriasis attending the Department of Dermatology in Yenepoya Medical College were enrolled during a period of 18 months.
Age distribution
In the present study among 110 patients it was found that, the maximum incidence was noted in the age group 31-40 years and minimum in the age group above 50 years of age. There were 39(35.5%) patients in age group 31-40 and only 13(11.8%) above the age of 50 years. The mean age of patients with melasma was 39 years.
Sex distribution
In our study out of 110 patients 76(69.1%) were female and 34(30.9%) were male showing the involvement of females were more than twice that in males.
Fitzpatrick skin type
In our study out of 110 patients, 99(90%) had Fitzpatrick skin type IV, followed by Fitzpatrick skin type V in 6(5.5%) patients and Fitzpatrick skin type III in 5(4.5%) patients.
In a sample of 302 Brazilian patients, 34.4% had skin type III, 38.4% had skin type IV and 15.6% had skin type V.[6]
In Tunisia, a survey of 188 women showed that: 14% had skin type III, 45% had skin type IV and 40% had skin type V.[7]
This is in accordance with our study as Fitzpatrick skin type IV is the predominant type.
Distribution based on occupation
In our study out of 110 patients it was found out that housewives 66(60%)constituted the majority of patients followed by farmers/labourers making for 28(25.5%) patients, employees 10(9.1%) patients, business men 4(3.6%) and others making 2(1.8%) of the total. They were exposed to sunlight for a prolonged period of time.
In a study conducted by Shenoi SD et al the prevalence of Melasms among paddy field workers in India reached 41.8%. However in our study farmers/labourers made for only 25.5% of the patients. Both these studies suggest that the intensity of sun exposure plays an important role in the development of the disease.[8]
Clinical classification
In our study among 110 cases it was found out that 65(59.1%) of the patients had a centrofacial pattern, 44(40%) patients had a malar pattern followed by only 1(0.9%)patient with a mandibular pattern. Hence clearly the Centrofacial pattern was dominant.
The observed predilection sites of melasma in our patients were areas receiving greatest UV exposure, e.g. fore- head, upper lip, infra- and supraorbital margins, and zygomatic process.
Family history
According to our study only 4(3.6%) of patients gave a positive family history of melasma.
Drug history
History of oral contraceptive pills use was present in only 2(1.8%) of 110 cases. Interestingly our study found similar results with a study conducted by Ortonne et al. who carried out a large survey in 12 centers of nine countries involving 324 patients to study the impact of UV radiation and hormonal influences in the development of melasma suggested there was a weak impact of OCPs in the evolution of melasma, especially in patients with a family history of melasma, supporting the view that hormonal contraceptives need not be changed in such patients.[9]
Menstrual history
In our study 48(43.63%) patients had regular cycles, only 6(5.4%) patients had irregular cycles. Menopause was seen in 23(20.9%) of women suggesting that it was women of reproductive age who have a higher chance of developing melasma. A study by Miot et al showed a significant reduction in prevalence after 50 years of age, which may be due to menopause and the reduction in the number and activity of melanocytes that occurs with aging.[10]
Melasma Area Severity Index
In our study out of 110 cases, patients with moderate MASI 73(66.4%)comprised of the majority, followed by 34(30.9%) patients with a mild MASI score. Only 3(2.7%)patients had a severe MASI score.
However in a study conducted by Yalamanchili et al[11] on 140 cases MASI score was 0-5 in 34(24.2%) of the patients, 6-10 in 70(50%) of the patients and more than 10 in 36(25.7%) patients.
However this is not in accordance with our study as the above study had almost three times more mild cases of MASI than in our study.
Wood’s lamp examination
Out of 110 cases patchy enhancement was seen in 62(56.4%) patients is suggestive of a mixed type of melasma. This was followed by enhancement seen in 40(36.4%) of the patients. Only 8(7.3%) of patients showed no enhancement indicating Dermal type of melasma.
This is in accordance with a study conducted by Carla TM[12] in which it was found out that mixed melasma is more followed by epidermal and mixed pattern.
Dermatoscopic pattern
In our study out of 110 cases 94(85.45%) of patients had a reticuloglobular pattern, 50(45.45%) of patients had perifollicular brown black globules, granules/dots was seen in 30(27.3%) patients and unpatterned pigmentation in 21(19.1%).
In another study conducted by Neema et al[13] it was found out that reticuloglobular pattern was seen in 83(83%) of patients followed by perifollicular brown black globules in 60(60%) of the patients. Granules/dots formed 28(28%) of patients and unpatterned pigmentation in 17(17%) of the patients. These findings are in accordance with our study.
Additional findings under dermatoscopy
In our study out of 110 cases telangiectasia was seen in 40(36.4%) of the patients followed by depigmentation in 27(24.5%) of the patients. None of them had ochronosis.
In a similar study conducted by Neema et al[13] telangiectasia was observed in 33(33%) of patients. This is in accordance with our study as our study showed similar results.
In another study by Chan et al[14] on 5 Chinese patients it was seen that there was no significant improvement in melasma and all five patients developed laser-induced depigmentation.
In our study none of the patients had Ochronosis. However in a study conducted by Kulandaisamy et al[15] it was found out that out of 104 patients only 5(4.8%) of the patients had Ochronosis. This shows that there is a minimal probability of developing Ochronosis.
Types of melasma under dermatoscopy
In our study out of 110 cases, 71(64.5%) patients had epidermal type of melasma followed by a mixed type in 33(30%) of the patients. However only 6(5.5%) patients had a dermal type of melasma.
Similarly in a study conducted by Carla TM[12] there was a predominance of epidermal type in 16 patients followed by Mixed type in 15 patients and only 9 patients with Dermal melasma. This is in accordance with our study.
Conclusion
A total of 110 patients with clinical diagnosis of melasma attending the Department of Dermatology in Yenepoya medical college were studied during a period of December 2016 to June 2018. In our study most of the patients were between the age group of 20 and 50 years. There is a clear female preponderance. Those with Fitzpatrick skin type IV constituted a major portion of our study. Those who engage in outdoor activities having sunexposure over an extended period of time namely the housewives and farmers/labourers dominated our study. Clinically Centrofacial pattern was the most common. Family history was not very significant. Most of the women had regular cycles. According to the MASI category moderate range was seen in most of the patients. Wood’s lamp examination revealed mixed type of melasma in contrast to the epidermal type seen under dermatoscopy. Among the patterns observed on dermatoscopy, the reticuloglobular pattern was seen in majority of patients which is favourable in its diagnosis as per various studies where this is considered to be a characteristic feature. In our study additional features such as telangiectasia and depigmentation were observed that helps in arriving at a conclusion that some form of treatment was taken for melasma. Hence all these findings help in analyzing the severity of the condition and planning treatment accordingly.
Source of funding
None.
Conflict of interest
None.
References
- D Bandyopadhyay. Topical treatment of melasma. Indian J Dermatol 2009. [Google Scholar]
- Ana Carolina Handel, Luciane Donida Bartoli Miot, Hélio Amante Miot. Melasma: a clinical and epidemiological review. An Bras de Dermatol 2014. [Google Scholar]
- Pearl E Grimes, Nanaka Yamada, Jag Bhawan. Light Microscopic, Immunohistochemical, and Ultrastructural Alterations in Patients with Melasma. Am J Dermatopathol 2005. [Google Scholar]
- A. Lallas, J. Giacomel, G. Argenziano, B. García-García, D. González-Fernández, I. Zalaudek. Dermoscopy in general dermatology: practical tips for the clinician. Br J Dermatol 2014. [Google Scholar]
- Pooja Arora, VijayKumar Garg, Sidharth Sonthalia, Narendra Gokhale, Rashmi Sarkar. Melasma update. Indian Dermatol Online J 2014. [Google Scholar]
- A.de.A. Tamega, L.D.B. Miot, C. Bonfietti, T.C. Gige, M.E.A. Marques, H.A. Miot. Clinical patterns and epidemiological characteristics of facial melasma in Brazilian women. J Eur Acad Dermatol Venereol 2013. [Google Scholar]
- C Guinot, S Cheffai, J Latreille, MA Dhaoui, S Youssef, K Jaber. Aggravating factors for melasma: a prospective study in 197 Tunisian patients. J Eur Academy Dermatol Venereol 2010. [Google Scholar]
- Danielle Cristina Zimmermann Franco, Gustavo Senra Gonçalves de Carvalho, Paula Rafaela Rocha, Raquel da Silva Teixeira, Adilson David da Silva, Nádia Rezende Barbosa Raposo. Inhibitory Effects of Resveratrol Analogs on Mushroom Tyrosinase Activity. Molecules 2012. [Google Scholar]
- JP Ortonne, I Arellano, M Berneburg, T Cestari, H Chan, P Grimes. A global survey of the role of ultraviolet radiation and hormonal influences in the development of melasma. J Eur Acad Dermatol Venereol 2009. [Google Scholar]
- Luciane Donida Bartoli Miot, Hélio Amante Miot, Márcia Guimarães da Silva, Mariângela Esther Alencar Marques. Fisiopatologia do melasma. An Brasileiros de Dermatol 2009. [Google Scholar]
- Ravali Yalamanchili, Veeranna Shastry, Jayadev Betkerur. Clinico-epidemiological study and quality of life assessment in melasma. Indian J Dermatol 2015. [Google Scholar]
- C Tamler, R M Fonseca, F B Pereira, C B Barcauí. Classificação do melasma pela dermatoscopia: estudo comparativo com lâmpada de Wood. Surg Cosmet Dermatoly 2009. [Google Scholar]
- Manas Chatterjee, Shekhar Neema. Dermoscopic Characteristics of Melasma in Indians: A Cross-sectional Study. Int J Dermoscopy 2017. [Google Scholar]
- N P Chan, G.Y. Ho, Shek Y.N., Henry H. Chan. A case series of facial depigmentation associated with low fluence q-switched 1,064 nm Nd:YAG laser for skin rejuvenation and melasma. Lasers Surg Med 2010. [Google Scholar]
- DevinderMohan Thappa, Divya Gupta, Sivashankari Kulandaisamy. Exogenous ochronosis in melasma: A study from South India. Pigment Int 2014. [Google Scholar]
- Introduction
- Materials and methods
- Source of data collection
- Method of data collection
- Details of clinical examination
- Inclusion criteria
- Exclusion criteria
- Sample size calculation
- Results
- Distribution based on occupation
- Distribution based on the clinical type of melasma
- Distribution based on Family history
- Distribution based on Drug history
- Distribution based on menstrual history
- Distribution based on Melasma Area Severity Index(MASI)
- Distribution based on Wood's Lamp Examination
- Distribution based on Dermatoscopic patterns
- Additional findings under Dermatoscopy
- Type of melasma under Dermatoscopy
- Discussion
- Clinical classification
- Family history
- Drug history
- Menstrual history
- Melasma Area Severity Index
- Wood’s lamp examination
- Dermatoscopic pattern
- Additional findings under dermatoscopy
- Types of melasma under dermatoscopy
- Conclusion
- Source of funding
- Conflict of interest
