Introduction
Psoriasis is a chronic inflammatory skin disease characterized by T-cell-mediated hyper proliferation of keratinocytes in the skin affecting about 2-3% of the world's population with equal sex incidence.1, 2 Approximately, 10-78% of patients with psoriasis have concurrent nail psoriasis, while isolated nail involvement is seen in 5-10% of patients.3 The typical cutaneous features of psoriasis include sharply demarcated, silvery white scaled erythematous plaques with a predilection for appearing on the scalp, lumbosacral region and extensor surfaces of the elbows and knees. Over time, the inflammation spreads to the nail matrix which leads to appearance of specific nail patterns which can act as diagnostic markers for psoriasis in cases of diagnostic dilemma with other papulosquamous disorders. Psoriasis of nails may affect the nail bed or the nail matrix.4 The various nail patterns in psoriasis are the presence of coarse irregular pits, subungual hyperkeratosis, oil drop sign, onycholysis, splinter haemorrhages etc. These patterns can be observed on gross examination of nails also but by then considerable damage to the nail unit has usually occurred and the management is delayed. Dermatoscopy is a highly practical diagnostic technique and an effective non invasive tool to facilitate the clinical assessment of nail diseases. In this study, we used dermatoscope as a tool to detect specific nail patterns in psoriasis which can aide in diagnosis and to detect utility of a dermatoscope in detecting these nail patterns.
Material and Methods
The present descriptive and observational study was conducted on 37 patients with skin biopsy proven psoriasis selected by stobe randomization, during the period of January 2018 to September 2019. An approval from the Institutional Ethics Committee was taken before hand. An informed consent was taken from each patient. All skin biopsy proven cases of psoriasis with clinically appreciable nail changes between the age group of 18-70 years were enrolled in the study. The nail biopsy was done wherever deemed necessary. A detailed history of all the patients was taken in terms of demographic details. Local skin and nail clinical examination was done to see morphology of nail patterns. It was followed by dermatoscopic examination of all the nails to see morphological changes in nail patterns and capillary examination to examine all twenty nails. The patients with history of trauma to nails were excluded from the study. The patients who showed clinical signs of superadded onychomycosis underwent KOH examination of nail clippings and were excluded from the study if found positive for fungal hyphae. Dermlite DL4 Dermatoscope with polarized mode and magnification of 10X was used. The non-polarized mode was used for nail plate examination to see for the nail plate surface changes. In few cases, Giemsa stain was used to stain the edges of the pits. The polarized mode was used for nail bed examination and color changes. Both wet and dry dermatoscopic examination were done. The dermatoscope was kept below the nail plate to visualize the subungual changes. The linkage fluid used was gel based hand sanitizer. All the nails were examined in a sequence of dermatoscopic examination of proximal nail folds, lateral nail folds, lunula, nail plate surface changes, nail bed changes, then vascular examination. The photographs of the findings were taken and recorded. The results were analysed statistically using SPSS Software 19.0 version. Chi-Square Test, Wilcoxon-Signed Rank Test, One-Way ANOVA stats were used for comparing different variables and making correlations.
Results
The mean age of presentation came out to be 41.5 years with SD of 13.2 amongst 16 females and 21 males patients. The patients were suffering from cutaneous lesions for a mean duration of 5.49 years. The duration of psoriasis in patients ranged from 1 to 9 years in our study with majority of patients falling in the category of beyond 5 years (56%). In our study we found that finger nails were affected in 97% patients and toe nails were affected in 78% patients. Nail plate and nail fold lesions showed highly significant nail patterns (Table 1).
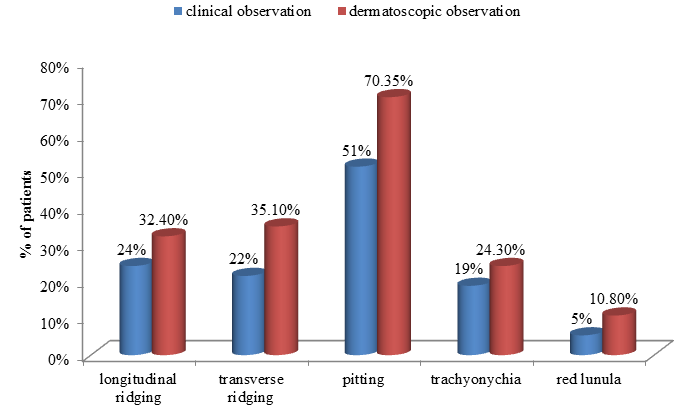
Nail matrix changes namely longitudinal ridges, Transverse ridges, nail pitting, trachyonychia and red lunula were observed clinically and dermatoscopoicaly and the observations were compared (Figure 1).
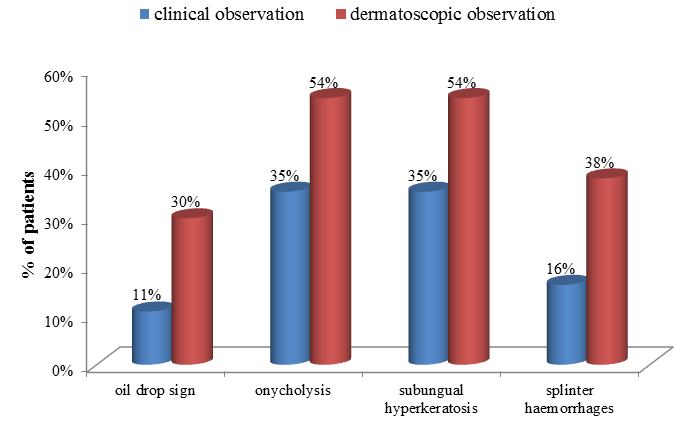
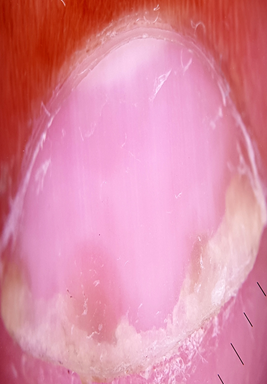
Nail bed dermatoscopy was done with linkage fluid and observations were compared with clinical observations (Figure 2). The difference in observations of all variables was statistically significant (p value- 0.020).
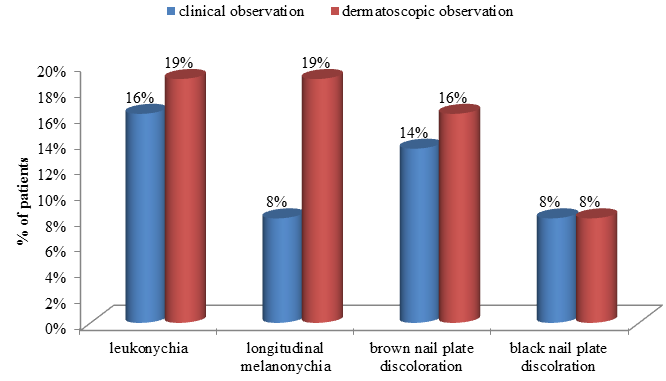
On examining the nails for chromonychia, leukonychia and longitudinal melanonychia and nail plate pigmentation was observed. (Figure 3)
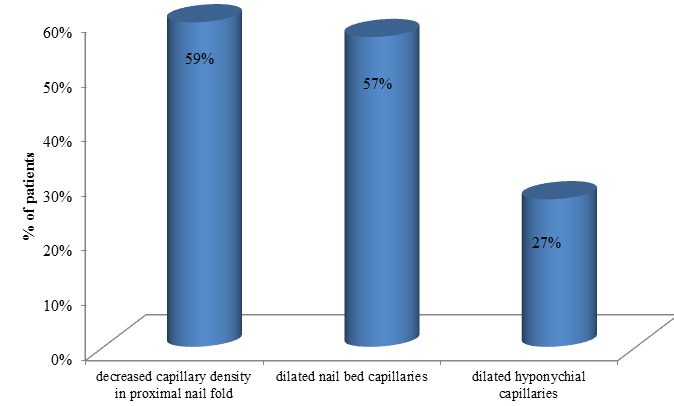
On examining proximal nail fold capillaries, decreased capillary density was seen in 22 patients. Dilated nail bed capillaries were visible in 21 patients and dilated hyponychial vessels were seen in 10 patients(Figure 4)
Table 1
howing nail fold and nail plate patterns in psoriasis
Discussion
In our study the most common finding was nail pitting seen clinically in 51.4% patients and with dermatoscopy in 70.3% patients. The second most common finding seen was onycholysis and subungual hyperkeratosis. Observed both clinically and dermatoscopically as 35.1% and 54.1% each respectively. This difference in observation was statistically significant as dermatoscope turning out to be a better modality to observe finer details. In a study involving 68 patients, Yadav TA et al. reported nail pitting to be the most common finding, followed by onycholysis which is consistent with our study.5 On the other hand, a recent study by Yorulmaz A of 67 patients reported splinter haemorrhages to be the most common finding followed by pitting and onycholysis.6 Parakeratosis is among the main histopathological features responsible for these manifestations. Within the matrix, parakeratotic cells interfere with the process of normal keratinization; as the nail grows, these cells slough off, leaving coarse psoriatic pits that usually manifest as large, deep and irregularly distributed cupuliform depressions.
We have divided nail unit changes into nail matrix and nail bed changes. In the nail matrix changes, longitudinal ridging was seen in 24.3% patients clinically and 32.4% patients with dermatoscope. Transverse ridging was seen in 21.6 % and 35.1% patients respectively. The clinical findings are comparable to study conducted by Puri N et al on clinical finding of nail dermatosis, where they found longitudinal ridging and transverse ridging in 12% and 14% patients respectively.7 In another study conducted by Bhatt YJ et al on dermoscopy of nail findings they found longitudinal and transverse ridging in 85% and 54% cases respectively which is higher than our study.8 So from our study, we infer that there is not much difference in clinical and dermatoscopic finding in these nail surface changes.
Another interesting feature of psoriatic nail matrix is erythematous lunula which has been considered as one of the prominent feature in some studies. We found erythematous lunula in only 5.4% patients clinically and 10.8% dermatoscopicaly. These findings were comparable to a dermatoscopic study conducted by Yorulmaz A et al where they found erythematous lunula in 1.5% patients as well as Klassen KM et al observed erythematous lunula in only 6.5% patients clinically. 9 In their study on nail psoriasis D daulatabad et al found erythematous lunula in only 7.3% patients clinically.10 In our study we found that in case psoriatic nail a perilunular erythematous halo was seen in majority of patients but not lunular erythema , this finding has not been described in any of the other studies.
Coming on to nail bed changes, the most characteristic feature of nail bed psoriasis is oil drop sign (salmon patches), onycholysis, subungual hyperkeratosis, splinter haemorrhages.. Parakeratotic lesions within the nail bed lead to salmon patches, parakeratotic cell shedding at the level of the hyponychium leads to onycholysis. These pits, which are filled with gel and surrounded by a peripheral whitish halo, are generally easily recognized via dermoscopy. Salmon patches, also known as the oil drop sign, refer to the yellowish-red discolorations that appear as irregular translucent areas visible on the nail plate. As per our observations, psoriatic onycholysis has a distinctive dermoscopic appearance comprising a typical erythematous border encircling a white onycholytic area. Dermoscopy improves the visualization of splinter haemorrhages, which are more vivid when newer and darker when older. Remarkably, the dermoscopic evaluation of our cases revealed not only typical longitudinal fusiform streaks but also minute pinpoint or elongated serpentine-like haemorrhages, which in our opinion result from nail matrix involvement because the delicate grooves underneath the nail plate deteriorate as the nail plate thickens. The difference in findings of nail bed patterns when compared clinically and dermatoscoicaly was found to be highly significant, hence proving that dermatoscopy has a dramatic advantage over clinical examination when it comes to detecting subtle, subsurface nail bed patterns.
The most prominent advantage of dermatoscopy in nail psoriasis lies in nail capilloroscopy. Iorizzo et al. conducted a videodermoscopic evaluation of the hyponychium in patients with psoriasis to introduce a method for visualizing the capillary network of the nails.11 In our study we found reduced capillary density in proximal nail fold in 59.4% patients, visible dilated nail bed vessels in 56.7% patients and dilated hyponychial vessels in only 27.3% patients. In a study conducted by Bhushan M et al they observed similar findings of decreased capillary density in proximal nail folds of psoriatic patients but none of the figures were mentioned. 11 In a study conducted by Yadav TA et al he found 54% patients had nail bed blood vessels as well as Yorulmaz A et al found 30% patients had dilated hyponychial blood vessels.5, 6 Our findings were in contrast to study by Bhat YJ et al who found 90% patients with dilated nail bed and hyponychial blood vessels.8 In 2012, Piraccini et al., described dilatation and tortuosity of the nail bed vessels in most of the psoriatic patients which were appreciated by examining the hyponychium.12 However, it was not appreciated in a lot of our patients, due to the pigmentation of the skin in the Indian population as a barrier for visibility of blood vessels in dark skin population. We suggest that these findings reflect the role of dermal microvascular expansion in psoriasis pathogenesis. In fact, psoriasis pathogenesis has been closely associated with increased angiogenesis. Several studies have focused on the pathogenic roles of angiogenic factors and microvascular changes in psoriasis. Increased dermal vascularity has been considered among histopathological hallmarks of psoriasis. Enhanced cutaneous blood flow, elongation and increased tortuosity and dilation of the dermal papillae capillary loops and high endothelial venule formation have been observed in psoriatic lesions.
Summary
The diagnostic features of nail patterns in psoriasis include nail pitting (70.3%), erythematoys lunula (10.8%), oil drop sign(29.7%), typical onycholytic pattern(54%), compact subungual hyperkeratosis (54%), decreased proximal nail fold capillary density(27%), visible nail fold dilated capillaries (56.7%). The difference in observation by clinical and dermatoscopic examination was statistically significant in nail bed changes but not in nail matrix and plate changes.
Conclusion
Psoriasis comes under papulosquamous group of disorders with overlapping clinical features affecting skin, hair and nail. The cutaneous features mimic each other in morphological as well as histopathological examinations. Establishing the diagnosis in such scenarios becomes difficult and thus hampers the treatment. In such situations, the nails can open the diagnostic window in the patients helping the clinician to arrive at a specific diagnosis. The knowledge of specific nail patterns in psoriaisis gives a diagnostic clue. But as per our observations mere naked eye examination of the nails can miss the subtle changes in nail patterns and more pathognomic nail bed signs and capillary examination can only be done with the help of a dermatoscope and can lead to early diagnosis of the condition for timely managment. Histopathology is a gold standard technique to confirm a diagnosis, but is an invasive procedure. Dermatoscope is a non-invasive tool that helps in visualization of surface and sub-surface changes.. Though it’s not a confirmatory tool, it definitely aids in making a diagnosis thus avoiding the invasive procedures.