Introduction
Psoriasis is a common, chronic, and recurrent inflammatory disorder of the skin characterized by well-defined erythematous papules and plaques surmounted by silvery- white scales over the extensor surfaces. The condition has different presentations depending on the activity of disease (stable, progressive, or resolving), anatomic site involved, and whether any treatment is being used.1 It is extremely variable even in its duration and course.
In the classical form of psoriasis, the disease is usually easy to diagnose on clinical features alone, which spares the use of skin biopsy for histopathological examination. Conversely, microscopic analysis of skin biopsy specimens is done to confirm the diagnosis in classic and clinically atypical variants and also to compare the clinical signs and symptoms with histopathological changes.2
Histopathological picture of psoriasis varies significantly with the stage of the lesion and has a diagnostic value only in early scaling papules or near the margin of advancing plaques.3 However in Indian population, the frequency with which an individual histopathological feature is seen in clinically diagnosed cases has not been extensively studied. For this reason, the study was done to note the correlation between clinical and histopathological features of psoriasis.
Materials and Methods
The study was conducted in the department of dermatology, tertiary care Centre from April 2015 to April 2016. 276 patients with psoriasis confirmed by biopsy were enrolled for the study. Psoriasiform dermatitis cases were excluded. Age, sex, duration, site of lesions, type of psoriasis, and individual histopathological features of psoriatic lesions were noted from the recorded data and analyzed.
Results
Psoriasis accounted for 1.3 % (276 patients) of total dermatology outpatients. Of 276 cases of psoriasis, 152(55.1%) were males, 124 (44.9%) were females with male to female ratio of 1.22:1. The mean age was 37.1 years. A maximum number of cases, 69 (25 %) were encountered in the 3rd and 4th decade of life with extremes of 8 and 76 years. Out of 276 patients, 13 of them were children (<12 years), and male to female ratio in children was 1:1.
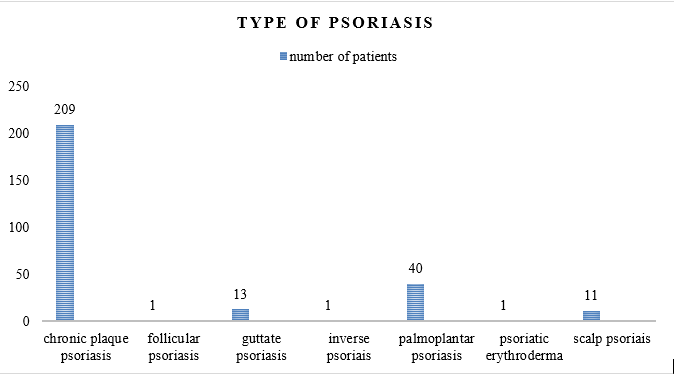
According to the Graph 1, the most common type of psoriasis was chronic plaque (75%), followed by palmoplantar (14%), guttate (4%), scalp (4%), follicular (0.4%), erythrodermic (0.4%) and inverse psoriasis (0.4%).
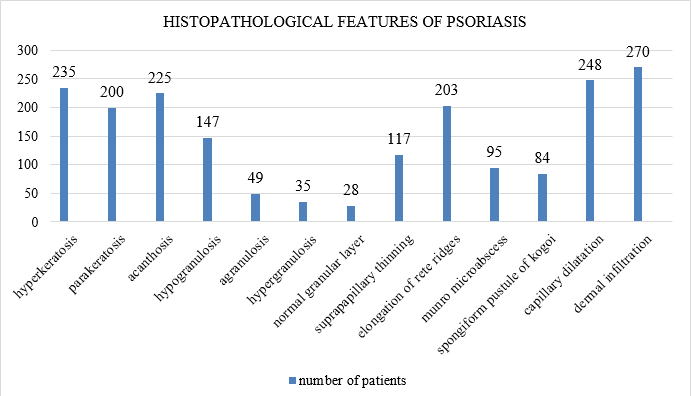
Histopathological findings of psoriasis are shown inFigure 1, Figure 2, Figure 3, Figure 4 and Figure 6. Following features were seen, hyperkeratosis (85%), parakeratosis (72%), acanthosis (81%), hypogranulosis (53%), agranulosis (17%), hypergranulosis (12.7%), normal granular layer (10%), suprapapillary thinning (42%), elongation of rete ridges (73%), Munro micro abscess (34%), spongiform pustule of Kogoj (30%), capillary dilatation (90%) and lymphocytic dermal infiltration (97.8%).
Table 1
1: Histopathology of various clinical types of psoriasis
Table 2
Comparison of histopathological features of psoriasis
Discussion
In various studies from India, psoriasis patients accounted for around 1% of the total dermatology outpatients. We noted 1.3% of cases of the total dermatology cases, which is in accordance with Okhandir et al. and Kaur et al. 9, 10
In our study, a preponderance of patients was between the age group of 30-40 years (25%), mean age was 37.1 years with extremes of 8 and 76 years. In the study by Kassi K et al., the average age of psoriasis was 39.6±3.3 years with extremes of 4 and 77 years.4 In the study by Alhumidi AA the age of onset of psoriatic disease ranged between 6 and 83 years with a mean of 31.5 years. 11
Children (<12 years) accounted for 4.7 % of total psoriasis patients. We noted the mean age of 10 years with extremes of 8 and 12 years, male to female ratio was 1:1 and chronic plaque psoriasis was the most common clinical presentation. In India, the largest series on childhood psoriasis was reported by Kumar et al.12 They presented data of 419 children with psoriasis. Children accounted for 12.5% of total psoriasis patients for 13 years. Age ranged from 4 days to 14 years, the male and female incidence was equal, and plaque type psoriasis was the most common clinical presentation.
Bedi et al. stated that psoriasis is twice more common in males compared to females.13 In our study, the incidence of psoriasis in both males and females were almost equal that is in accordance with Fry et al. 14 The increasing incidence among females shows that probably in this present time even females are more conscious about the appearance of the skin whether the skin lesions are exposed or unexposed.
In this study, chronic plaque psoriasis is the most common type. The second most common clinical type was palmoplantar psoriasis followed by guttate and scalp psoriasis. Inverse, pustular, follicular, and erythrodermic forms were very uncommon. There are only a few studies from India which have analyzed the clinical spectrum of the disease in psoriasis patients. Bedi at al.,15 analyzed data of 530 psoriasis patients seen for five years. Chronic plaque- type psoriasis was the most common (90%) clinical phenotype. The second most common clinical phenotype was palmoplantar psoriasis followed by flexural psoriasis. He found guttate psoriasis and psoriatic erythroderma to be uncommon. Okhandiar et al.,9 collected epidemiological data of 116 psoriasis patients from various medical colleges. They did not comment on the morphological types of psoriasis in their patients.
Extremities were the most common site of involvement followed by trunk and scalp. None of the patients had mucosal involvement in our study. Okhandiar et al.,9 found that the extensors (93%) were the most common site of involvement followed by the scalp (88%). None of their patients had mucosal involvement. In the Karumbaiah KP et al., study the most common sites of lesion were extremities followed by trunk and back. 16
In the present study as shown in Table 1, psoriasis had different clinical appearances and also had variations in their histopathologic findings.
The histopathological findings in the present study showed features consistent with psoriasis, but there were differences between the findings with other studies. A comparison of histopathological features of psoriasis with other studies is shown in Table 2.
In our study, it was seen that hyperkeratosis, parakeratosis, elongated rete ridges, and acanthosis were more prominent in most of the cases (85.1, 72.5, 73.6, and 81.5%). Alternatively, supra papillary thinning (42.4%) was less evident. The incidence of Munro micro abscess (34.4%) and pustules of Kogoj (30.4%) were more or less similar. Among the dermal changes dilated capillaries (90%) were more prominent in psoriasis even inflammatory infiltrate (97.8%) was prominent in most of the cases. These findings were similar to the study by Raghuveer C et al. 5
A study by Kassi K et al.,4 showed hyperkeratosis and agranulosis were exclusive epidermal features of psoriasis (100%), followed by supra papillary thinning (90.9%) and Munro microabscess (72.2%). In their study lymphocytic infiltrate (100%), dilated capillaries (63.6%), and tortuosity (36.6%) were the commonly observed dermal changes. Whereas in the current study, hyperkeratosis, parakeratosis, elongated rete ridges, and acanthosis were more prominent in most of the cases followed by Munro microabscess and spongiform pustule of Kogoj. But in the dermis, dilated capillaries were prominent.
Karumbaiah KP et al., the study showed Munro microabscess in 22.72%, spongiform pustule in 4.54%, hypogranulosis in 22.72%, and vascular changes in 86.36%.16 In the present study, similar findings of histopathology are seen.
The study by Mehta S et al., concluded that supra papillary thinning and absence of granular layer were the statistically significant features of psoriasis whereas, in the study by Bai S et al., hyperkeratosis, parakeratosis, exocytosis of inflammatory cells, spongiosis and dilated capillaries were the significant features of psoriasis along with hypogranulosis and agranulosis. 6, 7 In this study, hyperkeratosis, acanthosis, dilated capillaries and dermal infiltrate were significant features of psoriasis.
In the study, there were variations in the granular layer. Hypogrnaular layer and agranular layer were seen in 53% and 17% respectively indicates the features of psoriasis. About 12.7% showed hypergranulosis while 10% showed normal granular layer. Granular layer of epidermis in psoriasis in the Bai S et al., study was appreciated as a characteristic finding with prominent agranulosis or hypogranulosis. 7 Mehta et al., also stated that the absence of the granular cell layer could be added to the list of essential histopathological criteria for psoriasis, in addition to Munro microabscess and Kogoj’s abscess. 6 This finding of lack in the granular layer is consistent with the pathogenesis of psoriasis where the abnormal regulation of T cells interacting with keratinocytes causes defective keratinocyte proliferation. The variations in the granular layer in various studies can be explained that the plaques of psoriasis were either treated or resolving.
This study also shows capillary dilatation in most of the specimens similar to the study done by Pandit et al. 8 This can be considered as one of the histopathological clues to the diagnosis of psoriasis along with other findings.
Conclusion
Classic psoriasis is often straight forward to diagnose clinically. On the other hand, when the clinical presentation is varied, the definitive diagnosis may sometimes depend on the histologic examination. However, the histological changes of psoriasis are as varied as the clinical presentations. In such conditions agranular cell layer and capillary dilatation could be added to the list of essential histopathological criteria for psoriasis, in addition to Munro microabscess and Kogoj’s abscess. However, we would hasten to add that this is not the final word on this issue. Replication of results by other studies is the cornerstone of science. When similar studies are followed by systematic review and meta-analysis, we will arrive at a clear understanding of the essential histopathological criteria for psoriasis. Hence it is the combination of histopathological features of psoriasis with the clinical correlation that helps the physician to arrive at the diagnosis in doubtful cases.
Source of Funding
None.
Conflict of Interest
None.