- Visibility 75 Views
- Downloads 13 Downloads
- DOI 10.18231/j.ijced.2020.046
-
CrossMark
- Citation
Childhood Vitiligo: A hospital based retrospective study in Coastal South India
- Author Details:
-
Bansari Davda *
-
V Sivasubramanian
Introduction
Vitiligo is a chronic, acquired, multifactorial disorder of depigmentation of skin, characterized by well-defined white macules or large macules due to loss of functional melanocytes and melanin from the epidermis. Childhood-onset vitiligo has distinguishable epidemiological and clinical features as compared to adult-onset vitiligo. It starts before 20 years of age (before 10 years in 25% cases). A female prevalence, segmental presentation is common and association with other endocrine or autoimmune disorders is rare.
Vitiligo is a psychologically distressing disorder for the children as well as the care givers. Social stigmas, preconceptions, unawareness, prohibitions, and confusion about vitiligo are widespread in India. Hence, this study was undertaken to record various patterns of childhood vitiligo in Coastal South India.
Materials and Methods
Study type
Retrospective study
Study period
January 2015 to January 2020
Study sample
Children attending Dermatology outpatient department
Study place
Dermatology outpatient department at the Vinayaka Missions Hospital, Karaikal, Puducherry
Ethical considerations
Approval from Institutional Ethical Committee of Vinayaka Missions Research foundation, Karaikal was obtained, before starting the clinical study. Written informed consent was obtained in local vernacular language from every patient before enrollment.
Inclusion criteria
Children with diagnosis of vitiligo.
Participants less than 12 years old.
Participants who had given written informed consent.
Methodology
Demographic details of all patients like the age of onset, initial site involved, duration of disease, associated mucosal involvement and diseases and family history were obtained from the clinical notes.
Results
There were 19 (38%) boys and 31 (62%) girls out of the total 50 children with vitiligo. So, a female predominance is observed.
The mean age of onset of vitiligo was 5.8 years and the mean duration of disease was 1.4 years with majority of patients (44%) having more than 1-year duration.
| Age (in Years) | Number of patients(n=50) | Prevalence % |
| 0-1 | 06 | 12% |
| 2-5 | 16 | 32% |
| 6-12 | 28 | 56% |
| Duration (in months) | Number of patients (n=50) | Prevalence % |
| <6 | 16 | 32% |
| 6-12 | 12 | 24% |
| >12 | 22 | 44% |
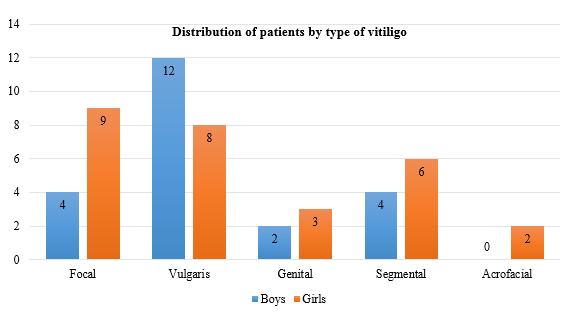
The most prevalent type of vitiligo seen in our patients was vitiligo vulgaris (40%), followed by focal (26%), segmental (20%), genital (10%) and acrofacial (4%). Vulgaris was more common in boys (63.1%) and focal type in girls (29.03%).
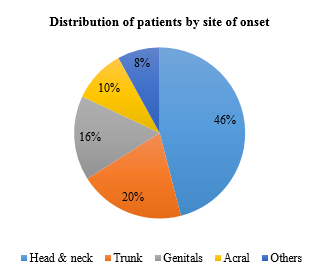
The most common site of onset was the head and the neck area (46%), followed by trunk (20%), genitalia (16%) and acral (10%).
Vitiligo family history was present in 5 (10%) patients. Thyroid disorder family history was present in 2 patients (4%) and Alopecia areata family history in 1 patient (2%).
| Family History | Frequency % |
| Vitiligo in 1o relative | 4% |
| Vitiligo in 2o relative | 6% |
| Thyroid in 1o relative | 2% |
| Thyroid in 2o relative | 2% |
| Alopecia Areata | 2% |
Bilateral involvement is seen in 72% patients and unilateral involvement in 28% of patients.
Involvement of mucosa, leukotrichia and koebnerization were seen in 12%, 11% and 10% patients, respectively.
Distribution of patients by clinical examination findings.
| Laterality | Prevalence % |
| Unilateral | 28% |
| Bilateral | 72% |
| Mucosal Involvement | 12% |
| Leukotrichia | 11% |
| Koebnerization | 10% |
Majority of the patients (49%) were having multiple lesions (more than 5).
Most (96%) had only less than 5% body surface area involved.
Distribution of patients by clinical examination findings.
| Number of Lesions | Prevalence % |
| Single | 23% |
| 1-5 | 28% |
| >5 | 49% |
| Body Surface Area (BSA)% | % |
| <5 | 96% |
| 5-20 | 3.5% |
| >20 | 0.5% |
Discussion
Vitiligo is an acquired, chronic, multifactorial disorder of depigmentation of skin characterized by well-defined white macules and large macules due to loss of functional melanocytes and melanin from the epidermis.
Female predominance is seen in the present study (62% vs. 38%), similar to the results in studies done by Jaisankar et al and Al-Jabari et al.[1], [2] Studies with male predominance were not found among children in contrast to that among adults (Shankar et al. [51.25%], Alzolibani et al. [52.63%], Singh et al. [56%] and Kar [51.6%]). [3], [4], [5], [6] So, there is more concern amongst parents in India when a girl is developing depigmented lesion than a boy as cosmetic appearance and related social and marital problems are more among girls in Indian structure.
Most of our patients (56%) were in 6-12 years of age group like in the study by Sheth et al. and Mu et al. [7], [8] and the mean age was (5.8 years) as compared to other studies by Al-Jabari et al. (7.9 years), Agarwal et al. (6.9 years), and Sheth et al (8.92 years). [2], [9], [7] In this study, head-and-neck region was the most common site of onset with 23 patients (46%), much higher than the finding (25.71%) by Jain et al. [10] Despite that, trauma prone sites like the lower limbs, hands and face may develop vitiligo lesions more easily in genetically susceptible individuals.The most prevalent type of vitiligo in boys in our study was vulgaris (63.1%) and in girls was focal (29.03%). The reason behind this finding could be a bigger worry in parents seeing even a single white patch in girls than in boys, making them consult the doctors early.
Family history findings of vitiligo in our study (first-degree relatives-affected in 4% patients, second degree in 6%) were similar to the Indian studies by Handa and Dogra (12%) and Jain et al. (17.5%) but much lesser than in the study by Nicolaidou et al. (35%). [11], [12], [10]
In this study, 28% patients had unilateral vitiligo and the rest had bilateral involvement. Involvement of mucosa was seen in 12% of patients, like in the study by Sheth et al. (18%) and genitalia were more affected (11%) than lips (6%). [7]
In a North Indian study, 8 out of 625 children (1.3%) had an associated autoimmune disease like alopecia areata, thyroid disease, diabetes mellitus, pemphigus vulgaris or Addison’s disease. [12] In our study, 1 out of 50 children (2%) had associated autoimmune disease like alopecia areata similar to study findings in Halder et al. study (2.4%).
Conclusion
As observed in our study, vitiligo can start at 2 months of age in children and is more prevalent in the age group of 6–12 years (56%). Thus, any depigmented patch in babies and children should be investigated carefully and followed-up regularly. Regional studies will help the clinicians practicing in these areas to be acquainted with its clinical and epidemiological patterns and be prepared for the management.
Limitations
The design of this study does not establish causal relationship. Sample size is small. Prospective studies with a larger sample size are required for this.
Source of Funding
None.
Conflict of Interest
None.
References
- T J Jaisankar, M C Baruah, B R Garg. Vitiligo in children. Int J Dermatol 1992. [Google Scholar]
- M M Al-Jabri, A Al-Raddadi. Childhood vitiligo: A retrospective hospital based study, Jeddah, Saudi Arabia. J Saudi Soc Dermatol Dermatol Surg 2011. [Google Scholar]
- D S K Shankar, R Madala, K Shashikala. Clinical patterns of vitiligo and its associated co morbidities: A prospective controlled cross-sectional study in South India. Indian Dermatol Online J 2012. [Google Scholar]
- A A Alzolibani, A A Robaee, H Al-Shobaili, F Al-Saif, E Al-Mekhadab, A A Settin. Association ofCYP2C9Genetic Variants with Vitiligo. Ann Dermatol 2014. [Google Scholar]
- S Singh, Usha, S S Pandey. Role of autoimmunity in vitiligo. Indian J Allergy Asthma Immunol 2009. [Google Scholar]
- P K Kar. Vitiligo: A study of 120 cases. Indian J Dermatol Venereol Leprol 2001. [Google Scholar]
- P K Sheth, S Sacchidanand, G S Asha. Clinico-epidemiological profile of childhood vitiligo. Indian J Paediatr Dermatol 2015. [Google Scholar]
- E W Mu, B E Cohen, S J Orlow. Early-onset childhood vitiligo is associated with a more extensive and progressive course. J Am Acad Dermatol 2015. [Google Scholar]
- S Agarwal, S Gupta, A Ojha, R Sinha. Childhood Vitiligo: Clinicoepidemiologic Profile of 268 Children from the Kumaun Region of Uttarakhand, India. Pediatr Dermatol 2013. [Google Scholar]
- S K Jain, S Kalwaniya, R Kumar, P Mehta, N Banjara, M Jain. Clinical profile of childhood vitiligo patients in Hadoti region in Rajasthan. Indian J Paediatr Dermatol 2014. [Google Scholar]
- E Nicolaidou, C Antoniou, A Miniati, E Lagogianni, A Matekovits, A Stratigos. Childhood- and later-onset vitiligo have diverse epidemiologic and clinical characteristics. J Am Acad Dermatol 2012. [Google Scholar]
- S Handa, S Dogra. Epidemiology of Childhood Vitiligo: A Study of 625 Patients from North India. Pediatr Dermatol 2003. [Google Scholar]
How to Cite This Article
Vancouver
Davda B, Sivasubramanian V. Childhood Vitiligo: A hospital based retrospective study in Coastal South India [Internet]. IP Indian J Clin Exp Dermatol. 2025 [cited 2025 Sep 08];6(3):227-230. Available from: https://doi.org/10.18231/j.ijced.2020.046
APA
Davda, B., Sivasubramanian, V. (2025). Childhood Vitiligo: A hospital based retrospective study in Coastal South India. IP Indian J Clin Exp Dermatol, 6(3), 227-230. https://doi.org/10.18231/j.ijced.2020.046
MLA
Davda, Bansari, Sivasubramanian, V. "Childhood Vitiligo: A hospital based retrospective study in Coastal South India." IP Indian J Clin Exp Dermatol, vol. 6, no. 3, 2025, pp. 227-230. https://doi.org/10.18231/j.ijced.2020.046
Chicago
Davda, B., Sivasubramanian, V.. "Childhood Vitiligo: A hospital based retrospective study in Coastal South India." IP Indian J Clin Exp Dermatol 6, no. 3 (2025): 227-230. https://doi.org/10.18231/j.ijced.2020.046
