Introduction
Acne is one of the most common skin diseases seen in clinical practice and is caused by multiple factors which originates in the pilosebaceous follicle.1, 2 Although a number of clinical studies have been carried out on acne, large-scale population studies which can really help to explicate the epidemiology and pathogenesis of acne have been limited and almost exclusively conducted in Western countries. 3, 4, 5, 6 For epidemiological study, population‑based data is important in quantifying social burden, distribution of the disease and its social and psychological impact in the community. Despite these facts, such data based studies on acne patients are lacking from India. Recently, few clinical studies have tried to address these aspects of acne in Indian population. 7, 8, 9, 10 But many of these studies have been comparatively small in scale and conducted at single institutions. The primary objective of the this study is to observe the prevalence, clinical features, contributing etiological and aggravating factors of acne in adults, with a view to establishing possible etiological factors and management of acne at different age group.
Materials and Methods
This study was conducted over a period of 6 months from April 2019 to September 2019 which was specifically designed to evaluate the epidemiology of acne in India and all questions were related to this objective. Ethical clearance was not obtained as it was an observational study. The adopted methodology followed the direct approach by questionnaire based document. A poll of 1500 Dermatologists across India was used for a random allocation of an acne questionnaire to 15000 acne patients. Patients presenting with acne vulgaris in any age group in the outpatient department of respective Dermatologist were included in the study. Patients presenting with other dermatological diseases with acne were excluded. The two-page questionnaire was designed and validated by authors. The questionnaire aimed to obtain different kinds of information such as age of patient, smoking history, history of diet, comorbidities, factors influencing acne (hormonal, drug intake, seasonal variations, pregnancy), manifestations and complications of acne and whether and in what form the treatment had been used (medical and cosmetic). Clinical assessment of each patient was done by Dermatologist including type of acne lesions, distribution, and severity and grading of acne. Acne vulgaris was graded into four grades.
Results
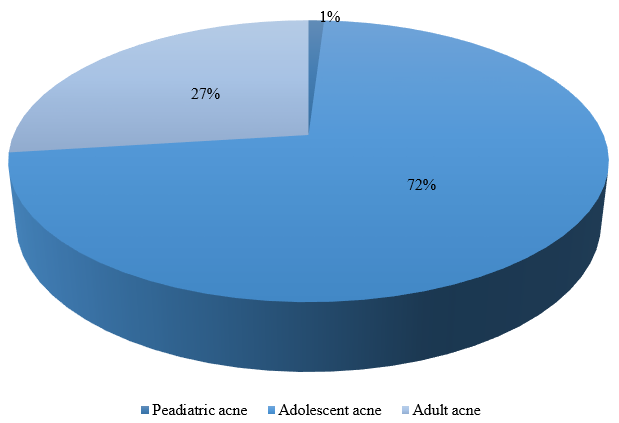
Out of 1500 Dermatologist, 1133 responded with a data of 6409 patients. Out of 6409 patients, 2884 (45%) were male and 3525 (55%) were females. The mean age of the patients was 24.64 years with a range of 10‑55 years. The proportion of population of different age groups is detailed in Figure 1 . Almost 72% of the patients are in the adolescent group followed by 27% in the adult group. Only 1% patients were reported in pediatric age group.
The different risk factors investigated were: smoking habit, diet history, cosmetic habit and causes of acne. 14% of the patients presented with smoking habits while high glycemic diet (HGD) was seen in half of the cases. Amongst HGD, junk foods topped the list (Table 1). Polycystic Ovarian Disease (PCOD) was seen in 727 females (21% of female patients).
Table 1
Percentage of patients with High Glycemic Diet and Co-morbidities in acne patients
| Characteristic | N | % |
| High glycemic diet | 3158 | 49 |
| Chocolates | 2020 | 32 |
| Soft drinks | 1912 | 30 |
| Junk foods | 2177 | 34 |
| Milk products | 1340 | 21 |
| No high glycemic diet | 1789 | 28 |
| Co morbidities | ||
| CAH | 370 | 6 |
| PCOD | 727 | 11 |
Knowledge of etiology of acne
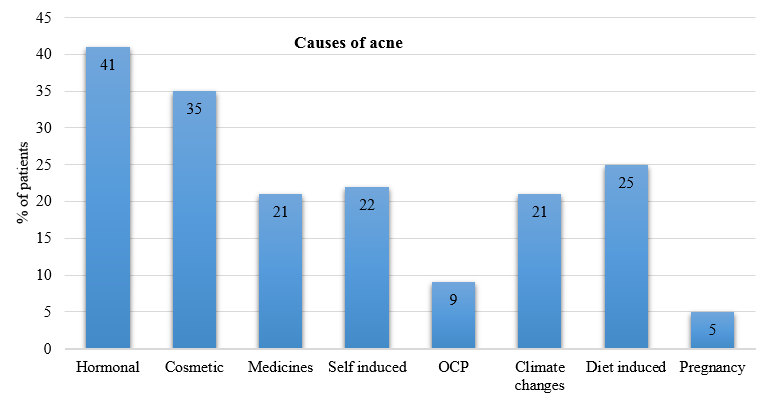
Of respondents, 41% knew that acne was associated with increased sebum production and blockade of pilosebaceous units whereas 35% associated acne with excessive cosmetic use. There was no significant gender difference in the aspect of knowledge. The detail causes of acne are listed below (Figure 2)
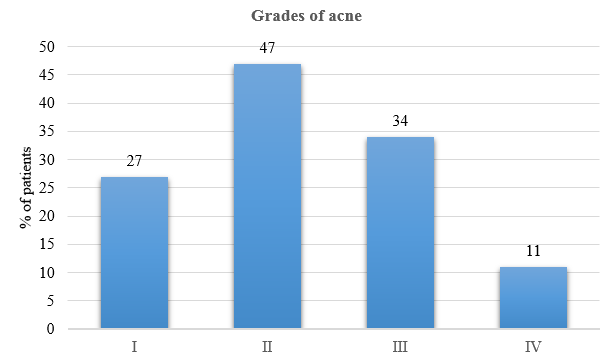
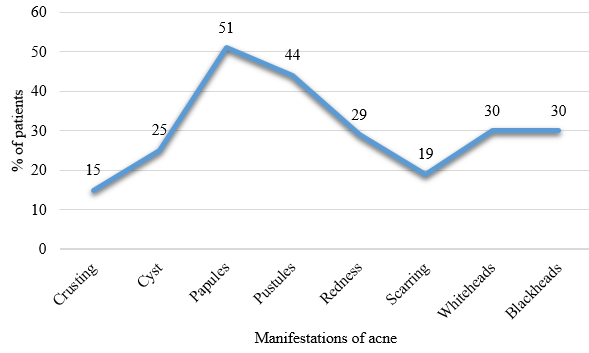
Grade II acne was seen in most of the patients (47%), followed by Grade III and I (Figure 3). Almost all the lesions were in the form of papules (51%), followed by pustules (44%). Blackheads and whiteheads were also noted with all types of acne lesions.
Complication of acne
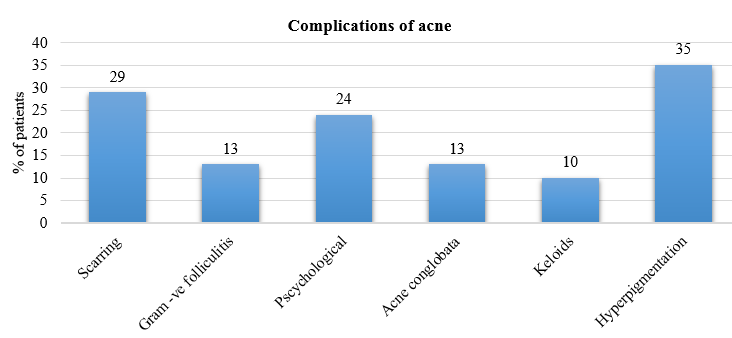
The presence of hyperpigmentation and scarring was considered to be a reflection of the severity of the acne. Hyperpigmentation and acne scarring were reported in 35% and 29% of the patients respectively (Figure 5).
Management of acne
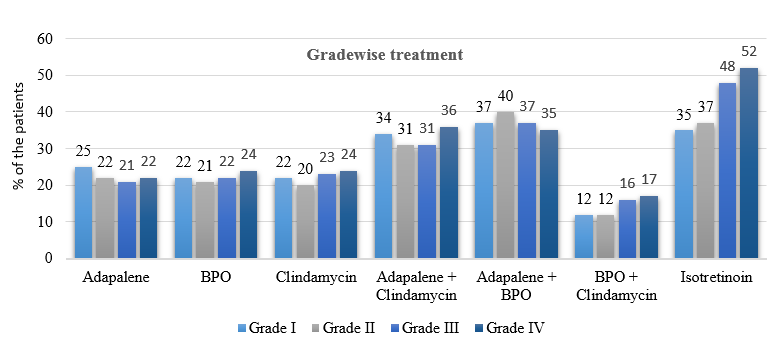
Moisturizers and cleansers are one of the most common supportive measure of acne management. Cleansers were prescribed for 53% of the patients whereas 43% of the patients were prescribed moisturizers. Amongst topical treatment, adapalene and BPO combination (34%) was the most commonly prescribed combination followed by adapalene & clindamycin combination (29%). Monotherapy was not commonly prescribed. Most of the patients were managed with combination therapy. Isotretinoin was most commonly prescribed medication in all grades of acne comprising of 40% of the patients. Systemic antibiotics and OCP were not commonly prescribed. Acne grade-wise different treatment options are depicted in Figure 6.
Table 2
Percentage of patients with different treatment modalities
Discussion
To our knowledge, this study is the first epidemiological study investigating multiple factors associated with acne in the general population in India. A self-administered questionnaire is an adequate tool for such epidemiological studies in the general population. However, as self-recording of acne and its associated factors might be difficult for lay-persons, a detailed description of this information was given in the questionnaire and correspondence, and validated with a clinical dermatological examination by dermatologists. This kind of reporting is also more adequate as seen in other clinical studies.
Acne vulgaris is a chronic disease affecting the pilo-sebaceous glands. Though a disease predominating in adolescence data indicates that the age distribution of acne is widening and this is happening in both sexes but more prominently in woman over the age of forty years. 11 A previous study in South Indian population showed a male preponderance, 7 whereas Raghavan JS et al 8 reported a female preponderance. The mean age was 24.64 years which is different with some other studies. 7, 12
In this study, about 27% of the acne cases were of adult acne which is in line with Raghavan JS et al 8 study but against the previous study from South India which reported only 9.3% adult acne (age >25 years).7 Again, the most common age group involved in this study was 18-25 years (55.7%) while it was 16-20 years (59.8%) in the same study. 7
This indicated that adult acne can either persist from adolescence or be late onset beginning in adulthood. In the study done by Khunger and Kumar,9 acne was persistent from adolescence in a majority of patients (73.2%) whereas Goulden et al13 noted that 82% of the study population had persistent acne. Similarly, in our study, 55.7% had persistent acne which in concordance with another study by George et al. 10 Thus in a majority, acne develops in adolescence and persists into adulthood.
Historically, there was much debate on the subject of diet in the management of acne. Cordain et al. postulated that high glycemic diets may be a significant contributor to the high prevalence of acne in Western countries. 14 It was hypothesized that milk and dairy products carried hormones and bioactive molecules that had the potential to aggravate acne. Almost half of the patients in our study gave the history of high glycemic diet. About 25% could attribute their exacerbation of the lesions due to the intake of diet.
In female subpopulation, cosmetic induced acne has been discussed as an important cause acne. 15 Many cosmetics including some sunscreens are comedogenic. 10 Some well‑known cosmetic ingredients are comedogenic e.g. isopropyl myristate, lanolin, butyl stearate, etc. 16 In one study done in India, facials were observed to have caused acneiform eruptions in 33.1% of participants. 17 Oils form an occlusive film over the applied area and may cause comedogenesis and aggravation of acne. Most of the sunscreens are too oily for acne patients and tend to aggravate it. Khunger and Kumar observed aggravation of acne due to cosmetic in 22% of the patients.9 In our study, 35% patients reported aggravation of lesion after using some form of cosmetics.
An Indian study by Sardana et al. showed that majority of patients with acne vulgaris worsened during climate change especially summer.18 In our study, 21% patients reported aggravation due to seasonal changes. Khunger and Kumar in their study reported summer season as an aggravating factor in 36.7% of patients.9
Surprisingly, in our study 21% patients claimed medicines as causative factor of acne. The well-known causative drugs are corticosteroids, anti-epileptics, antidepressants, antipsychotics, anti-tubercular drugs, etc.19 Khunger and Kumar observed that there was no significant relation with drug usage in their patients, except the use of topical steroids which caused aggravation in all the patients applying it (11.8%). 9 Self-manipulation of acne lesions are a mainstay of acne (22%) which in contrast with another study in France. 20
In our study, pregnancy was associated with worsening of acne in 5% which is in corcordance with Khunger et al. 9 This is in contrast to the study by Goulden et al., where pregnancy resulted in a flare in 18%. 13
We graded the lesions using a simple 4 graded system 21 and got predominantly grade 2 (47%) and grade 3 (34%) lesions in these subjects as seen in recent study. 8 Raghavan JS et al reported Grade 1 and grade 4 in 8% and 18% respectively as compared to our study where we got 27% and 11% in Grade I and grade IV respectively. 8 This finding is a diversion from the previous studies pointing to the possibility of a greater inflammatory nature of acne vulgaris. 7, 22, 23
Scarring and hyperpigmentation are very common complications of acne which is seen in 29% and 35% of the patients in our study. This is probably because acne in adolescents and adults is predominantly inflammatory and may be resistant to treatment. Treatment is often delayed in such patients, which leads to greater chances of these complications. One Indian study for acne of all groups documented scarring and hyperpigmentation in 39.5% and 24.6% of the patients respectively.7 Goulden et al., observed scarring in 77.2% men and 58.5% women. 13 In our study, supportive therapy in terms of cleansers and moisturizers are well prescribed. Role of cleansers is well defined in many articles. In a study by Veraldi et al., 69% of the patients reported using cleansers as adjunctive therapy to acne. 24 Skin cleansers lower the surface tension on the skin and thus help to remove dirt, sebum, oil from cosmetic products, microorganisms, and exfoliated corneum cells in an emulsified form. 25 Many anti acne therapies are associated with dryness of the skin and hence moisturizers are commonly prescribed. Thiboutot and Del Rosso, 26 Del Rosso and Brandt 27 highlighted the role of anti-acne therapy in epidermal barrier damage. The moisturizer component assists in mitigating epidermal barrier impairment and its related skin sensitivity and irritation. 28, 29, 30 Role of moisturizer in acne in India has been well studied by Bhat et al. 31
Adapalene and BPO was most commonly prescribed combination medication in our study. Recent guidelines on acne also mentions to use this combination as first line of therapy. 32 Combination therapies are preferred to avoid skin sensitization, antibiotic resistance as well as to enhance the treatment outcomes. 33, 34, 35, 36, 37, 38, 39, 40, 41 In combination therapy, multimodal therapy targets different pathological processes, simultaneously, leading to a better outcome due to synergistic effects. 42 Studies also report that combination therapy plays a role in improving patient adherence due to incorporation of simplified and personalized daily regimen. 42, 43
Adapalene and clindamycin was second most commonly prescribed combination. This could be due to assistance of adapalene for the penetration of clindamycin into the pilosebaceous unit (colonization site for P. acnes), hence achieving better efficacy. 34
Currently, only available retinoid in India is isotretinoin for the treatment of acne. It targets all four major factors involved in the mechanism of acne, viz., stabilizing the follicular desquamation, suppressing the sebum production, preventing the P. acnes growth, and allowing anti-inflammatory action.44, 45, 46 Although isotretinoin is recommended for severe acne, in real-life practice, it is used earlier in the treatment of acne, commonly in all grades of acne. The same is reflected in our study.
This large‑scale analysis presents the demographic features, etiology, pattern, complications and management of acne among Indian patients. Epidemiological studies on acne have been conducted primarily in the West, and few studies have been performed in Asian patients. Herein, we report the findings of a collaborative study involving 6409 Indian patients. A limitation of this study is that the large number of variables included in the statistical analyses may make it difficult to evaluate the relative contribution of each factor to acne. Furthermore, as the patients were recruited from large number of clinics, the data collection process may have been subject to either selection or recall bias. In the future, larger, community-based, epidemiological studies are warranted to better delineate the characteristics of acne patients in India. However, to the best of our knowledge, no large-scale study of this type from India has been reported previously. We believe that the study outcomes will be useful in future studies comparing Indian and other populations and during patient consultation and treatment.