Introduction
Kaposi sarcoma (KS) is a low-grade vascular neoplasm caused by proliferation of lymphatic endothelium associated with infection of endothelial cells by human herpes-8 (HHV-8). However, since 1979, KS was found to be increasingly common in immunosuppressed individuals such as organ transplant recipients or patients infected with the human immunodeficiency virus (HIV).1 Four clinical variants have been described for the disease, differing in natural history, site of predilection, and prognosis. Classic Kaposi sarcoma (CKS) is a rare and slow growing variant commonly seen in elderly Eastern European and Mediterranean population which presents with reddish-brown papules and nodules particularly on the lower limbs. 2 We report a case of CKS in an 81-year-old HIV-negative male with predominant involvement of lower extremities and profound lymphedema.
Case Report
An 81-year-old male presented with asymptomatic violaceous papules, plaques and nodules with swelling of the lower legs for 1 year. He had no history of intravenous drug use, homosexuality or other high risk sexual behaviour, or use of immunosuppressive drugs. He had completed a course of anti-tubercular medicines 7 months back for pulmonary tuberculosis.
Cutaneous examination revealed bluish-black discrete papules and small nodules on feet and lower legs as well as indurated, hyperkeratotic large plaques with ulceration on the left foot (Figure 1, Figure 2). Significant non-pitting edema with peau d’ orange appearance was seen on both legs (Figure 1). Mucous membranes including oral, nasal and genital mucosa were normal. Lymphadenopathy was absent and systemic examination findings were normal.
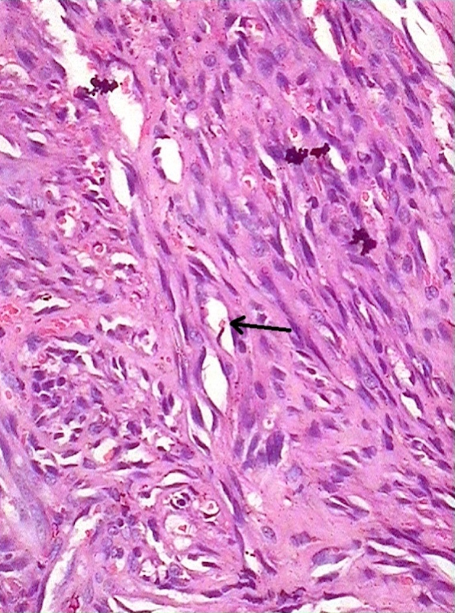
Histopathological examination of the papular lesions on the left foot showed densely collagenized dermis with numerous foci displaying plump spindle cells and numerous slit-like spaces containing red blood cells lined by spindle cells (Figure 3). Routine blood investigations revealed anemia. HIV serology was negative. However, the total lymphocyte count and absolute CD4+ T lymphocytes count were 650/µL (<1,000/µL) and 94/µL (<500/µL) respectively. Other tests including hepatitis B and C serology were negative. Ultrasonography of whole abdomen, magnetic resonance imaging of the soft tissue of legs and Doppler study of lower limbs were normal. Chest X-ray showed features of old pulmonary tuberculosis.
A diagnosis of CKS was made based on the clinical and histological findings. Combination of chemotherapy and radiotherapy was started. Injection liposomal doxorubicin 40 mg/m2 and etoposide 150 mg/m2 were given 3 weekly. The skin lesions improved significantly on subsequent follow-ups. However, the patient expired after receiving 4 cycles of this regime.
Discussion
The aetiology of KS remains unclear. Age, socio-economic status, consumption of traditionally brewed alcoholic beverages, high anti-HHV-8 titers and pulmonary tuberculosis have been reported to be various co-factors in the development of KS. 3, 4 Histology of the lesions is characterised by spindle cell proliferation in a directional streaming pattern, admixed with fibroblasts, endothelial and inflammatory cells. 1
The four clinical variants of Kaposi’s sarcoma are classical, endemic, immunosuppression-associated (transplantation-associated) and epidemic or AIDS-associated. Classical non-HIV KS is considered a rare disease. 2 It is mostly seen among elderly men (50-80 years) and characterized by vascular-appearing plaques and nodules mostly over the lower extremities. Pedal edema can precede or follow the onset of the lesions. It follows an indolent course and disseminations and visceral lesions occur later. 2 The only HIV-negative KS reported from India involved a 45-year-old female presenting with multiple painful reddish brown plaques, papules and nodules on both lower limbs and left index finger. 5 CKS risk has been found to be positively associated with reduced hemoglobin, CD4 and CD8 positive lymphocytes and increased monocytes. 6 HIV-associated KS, however, follows an aggressive course and has poor response to therapy as compared to the other forms. 2
Treatment modalities of KS include surgery, radiotherapy, chemotherapy and immune therapy depending on the stage of the disease. For patients with single lesions, excisional biopsy often provides adequate treatment. Extensive or recurrent cases can be treated with a combination of surgery, chemotherapy, and radiation or with chemotherapy alone. 7
Conclusion
This is the first case report of HIV-negative CKS from Northeast India, thus, showing wide ethnic and geographic area of prevalence of this condition. Careful clinical and histological examinations are necessary in suspected cases without HIV infection as KS is not always associated with HIV. Since KS in HIV-negative patients respond adequately to available treatment protocols, early diagnosis and treatment is warranted to improve survival from this uncommon disease.