Introduction
Acne vulgaris can be categorised as one of the single disease that results in psychic trauma, a feeling of insecurity and emotional impact in many adolescents, which can last a lifetime. Data from western countries suggest Acne vulgaris can occur in 80% of people between 10-30 years of age.1 Scarring may occur in 95% of those with acne vulgaris, related both its severity and delay in treatment. Atrophic acne scars are the most common type. The atrophic acne scars can be – ice pick scars, boxcar scars and rolling atrophic scars.2 Treatment of the acne scars provides a therapeutic challenge for dermatologists. Options available for the treatment of acne scars, include chemical peeling, dermabrasion, laser treatment, punch techniques, fat transplantation, fractional microneedling, subcision, and combined therapy.3 Dermatologist should individualize the best treatment options for each patient.
Pain perception and its implication
Most of the patients have fear of the injections rather than the procedure itself. The patient may perceive mild to moderate or severe pain depending on the procedure and the technique of anaesthesia used. The procedural pain, fear of needles and associated stress and anxiety are of major concern for the dermatologist.4 Hence the dermatologist should have an in-depth knowledge about the anaesthetic techniques and the drugs used.
Fractional microneedling, also known as percutaneous collagen induction, is a recent addition to the treatment modalities for acne scars. With this technique, thousands of micropunctures (192 fine micro needles in eight rows, 0.5 – 1.5 mm in length and 0.1mm in diameter) are made in skin up to level of mid dermis. This initiates a complex cascade of growth factors that finally results in collagen and elastin production in dermis. Also, new capillaries develop, leading to reduction of scars.
Minimally invasive procedures require either topical or injectable local anaesthetics to ensure adequate analgesia during the procedure. However, injectable forms of local anaesthetics, although effective, are uncomfortable for the patient during administration. Regional nerve blocks will cause discomfort and anxiety for majority of the patients and may leave skip areas. Tumescent anaesthesia, on the other hand, need multiple needle pricks and may result in unsightly edema. 5 Thus, we are in need of a proper patient preferred anaesthetic modality for patient acceptance and the operator comfortness. Traditionally, topical application of eutectic mixture of topical 2.5% lignocaine and 2.5% prilocaine cream (EMLA) is being used for these procedures. But various studies have given a mixed result of its efficacy in pain relief. Newer anaesthetic drug with eutectic mixture of Lignocaine 7% with Tetracaine 7% (LT cream) have been introduced and found to have a quicker onset of action with a greater potency and a relatively fewer side effects.
Topical anaesthetic preparations6
Topical anaesthetics penetrate the stratum corneum through the epidermis to act on the dermal nerves. They act by reversibly blocking the pain conducting nerve fibres which can act for minutes to hours depending on the site, dose, drug metabolism and elimination. Eutectic mixtures are one which has lower melting point than any one of the individual components which permits higher concentration of anaesthetic drug to be used.7
The components of EMLA are, it is a 5% oil in water emulsion cream which contains 2.5% of Lignocaine and 2.5% of prilocaine. EMLA cream is applied as thick layer over the intact skin in a dose of 1-2g/10 cm2, up to a maximum dose of 20 g/200 cm2, and covered by occlusive dressing to promote the depth of penetration. Depth of anaesthesia achieved depends on the duration of contact time with the anaesthetic.
Various studies reported that after 60 minutes application of EMLA cream, dermal analgesia was obtained to a depth of about 3mm. The maximum depth of analgesia of 5 mm was achieved after 120 min. of application.8 Dermal analgesia continues even after removal of the topical anaesthesia, presumably because accumulation of the product in the stratum corneum. The duration of analgesia after 1-2 hour application is at least 2 hours.
LT cream is a self occlusive cream which when exposed to air forms a film that increases the dermal absorption. Tetracaine is an ester group of anaesthetic. Lignocaine 7%/ tetracaine 7% cream is the first FDA approved cream which contains the highest concentration of the drug which is proved to be safe and effective. Lignocaine being more aqueous soluble produces a faster, more intense, long lasting anaesthesia. On the other hand tetracaine, being more lipophilic gets accumulated in the epidermis and slowly diffuses and gives a prolonged anaesthesia. Thus it has a longer duration of action and a reduced systemic toxicity. As a result, LT combination produces a rapid and durable anaesthesia.9
Depth of analgesia obtained by this technique is 6.8 mm. 10 Tetracaine is more lipophilic than prilocaine or lidocaine, thus penetrates stratum corneum more easily.
When used according to recommendations, LT combination is reported to have mild side effects and a safe profile.9
Microneedling requires an analgesic depth of 0.5- 2mm, which is effectively achieved with topical anaesthesia.
Visual Analog Scale (VAS)
Pain is a subjective phenomenon and hence its objective measurement is difficult. Various pain scales are available for clinically assessing the pain during and after procedures and also to measure the effectiveness of anaesthetics used. Pain scores are now considered the fifth vital sign.11
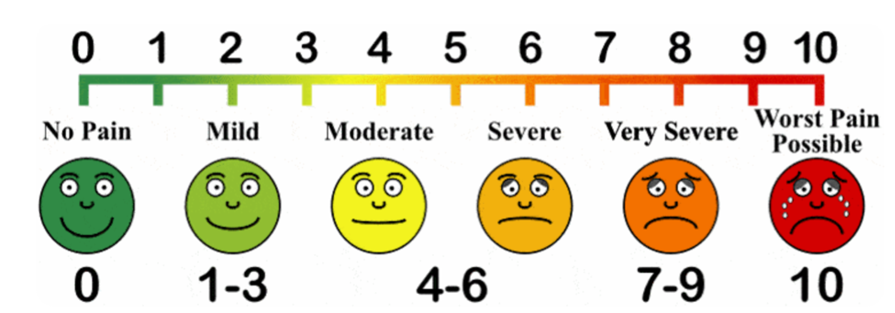
In our study, Visual Analog Scale (VAS) method was used to assess the pain that patients experienced. The Visual Analog Scale (VAS) was first used by Hayes and Patterson in 1921. The values can be used to track pain progression for a patient or to compare pain between patients with similar conditions.12 The simplicity, reliability, and validity, as well as its ratio scale properties, make the VAS the optimal tool for describing pain severity or intensity. 13 when using VAS to assess pain, subjects were asked to indicate intensity by marking a (usually) 10cm long horizontal line that is labelled “no pain” at one end and “worst pain possible” at the other end (Figure 1). The scales correlate with pain intensity measured by other methods.
Materials and Methods
This study was conducted in the department of Dermatology, Rajah Muthiah Medical College during November 2018 to October 2020. Ethical clearance was sought from Institutional Ethical committee. Patients in the age group 18 to 60 years were selected according to the inclusion criteria-Patients with acne scars scheduled for treatment who were able to give written informed consent. Exclusion Criteria followed were hypersensitivity to local anaesthesia, Pregnancy or Lactation, current treatment with systemic analgesics or medications that can influence pain sensation. Also patients with active acne, history of keloidal scars, bleeding disorders, active skin infection like warts, herpes and bacterial infection were excluded.
A total of twenty patients were selected based on the inclusion and exclusion criteria, after obtaining written informed consent, detailed history and thorough clinical examination and basic haematological parameters were checked. Any history of drug hypersensitivity was sought. Patients were allotted to either group A receiving 2.5% Lignocaine and 2.5% Prilocaine cream (EMLA) or group B receiving 7% Lignocaine and 7% Tetracaine cream (LT), based on computer derived randomisation. Patient’s baseline parameters were measured and they were administered either of the topical anaesthetic creams under occlusion. After a period of 30 minutes, pain sensation was assessed using a pin prick, and Visual Analog Score of pain perception was recorded. At the end of 60 minutes, the micro-needling procedure was carried out. If patients couldn’t tolerate the procedure, they were supplemented with additional infiltration anaesthesia. Patients were asked to validate their pain score, during the procedure. They were kept under observation for 2 hours to look for any complications and also asked to note the time of onset of pain, to be mentioned during their follow up.
Results
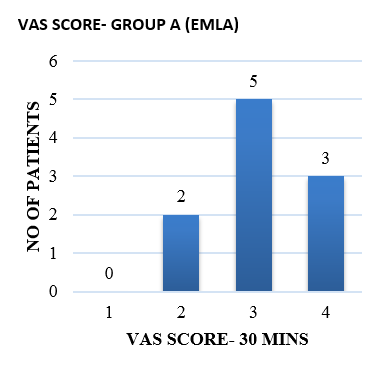
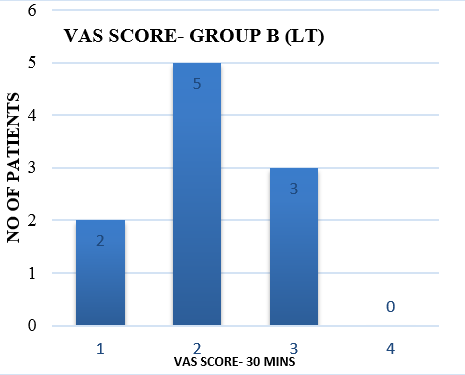
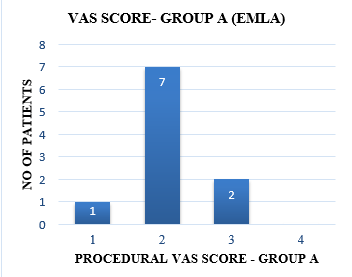
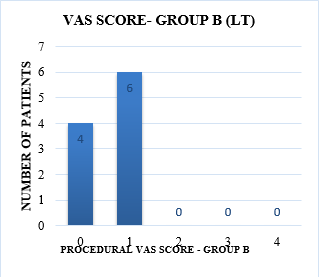
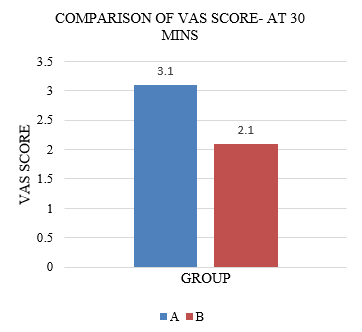
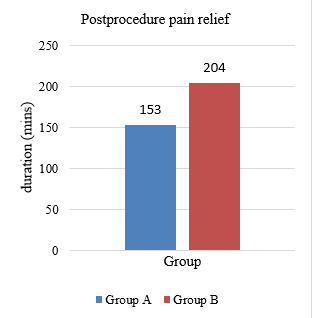
In our study, the mean age of patients was 23.8 years with the minimum age being 17 years and the maximum age being 35 years. Male Female ratio was 0.82:1. Acne scar duration was between 1 year to 6 years. Pre operative vitals were recorded. After applying the test drug, the mean pain score after 30 mins was 3.1 for group A and 2.1 for group B. The pain score during the procedure was 2.1 for group A and 0.6 for group B. The adverse effects noted were erythema (2- group A, 2- group B) itching (1-group A, 2-group B) edema (1-group A). All were transient and did not require any intervention. None of the patients needed additional anaesthetic requirements. The mean duration of post procedural pain relief was 153 minutes for group A (min- 60 mins, max- 240 mins) and 204 minutes for group B (min- 120 mins, max- 240mins).
Table 1
Showing demographic characters of the study population
|
Group |
Male |
Female |
Total |
|
A |
4 |
6 |
10 |
|
B |
5 |
5 |
10 |
Table 2
Mean VAS scores of the study groups at 30 mins and during procedure.
|
Group |
VAS at 30 min |
VAS During Procedure |
|
A |
3.1 |
2.1 |
|
B |
2.1 |
0.6 |
Discussion
Acne Scar is an unsightful picture imparting a severe psychological stress in the individual. The advances in the management of the acne scars has provided multiple treatment options of which micro-needling is one which has got good success rate of healing.
Traditionally infiltration anaesthesia was used, which is associated with undue anxiety and significant pain during administration. With the advent of novel anaesthetic drugs, different drug formulation and drug delivery systems, the modality of providing anaesthesia to office based anaesthetic procedures grew tremendously.
The preferred topical anaesthetic should have shorter onset time, providing adequate analgesia, and minimal systemic absorption with no or minimal side effects both local and systemic. Eutectic mixtures can bridge the niche between the invasive and non invasive mode of analgesia. In our study there was a significant difference in the VAS score between the two groups both at 30 minutes and during the procedure. LT cream had shorter onset time and demonstrated good analgesic efficacy. Alster et al reported similar findings in a study conducted on patients coming for full face laser resurfacing with CO2.14 Our study findings also concurred with Chen et al who used S-caine (tetracaine) peel for induction of local anaesthesia for laser assisted tattoo removal.15 The adverse effects noted were erythema, itching, and oedema which were transient and self-limiting in both the creams. Local anaesthetics drug related side effects were not noted may be it is due to the dosage used as per manufacturer recommendations. We noted that, LT cream produced a long lasting analgesic effect when compared with EMLA cream.
Limitations
Our study was conducted only on patients with acne scars, to demonstrate the superior efficacy of drugs more spectrum of procedures need to be included. Sample size, blinding the patients for the drugs are other limitations of the study.
Conclusion
In conclusion, we infer from our study, topical anaesthetic cream- lignocaine tetracaine is more effective than topical lignocaine prilocaine cream for microneedling procedures. They have a minimal side effect profile and also provide longer duration of post operative analgesia than EMLA cream.