- Visibility 308 Views
- Downloads 40 Downloads
- Permissions
- DOI 10.18231/j.ijced.2020.065
-
CrossMark
- Citation
A prospective study to evaluate the repigmentation in vitiligo after noncultured epidermal cell transplant followed by puva
- Author Details:
-
Mohammed Azharudeen
-
P K Kaviarasan *
-
Kannambal K
-
Poorana B
-
Abhirami C
Abstract
Aim of the study: To evaluate the repigmentation with non-cultured epidermal cell suspension followed by PUVA in patients with stable vitiligo.
Materials and Methods: A prospective study conducted at the department of Dermatology, Venerology, Leprosy of Rajah Muthiah Medical College and Hospital. 26 cases of stable vitiligo were treated with non-cultured epidermal cell suspension followed by PUVA and were reviewed for a period of 20 weeks.
Results: The results were assessed subjectively. 9 (34.6%) patients showed excellent response to our therapy, 7 (26.9%) patients had good response, 5 (19.3%) patients showed fair response and 3 (11.5%) showed very poor response. 17 (65%) patients showed a very good colour match when compared with the surrounding skin and 1 (3.8%) patients showed donor site scarring.
Conclusion: Epidermal non cultured cell suspension followed by PUVA is a relatively safe method with superior quality of repigmentation.
Introduction
Vitiligo is the most common acquired depigmentation disorder worldwide equally affecting people of both sexes.[1] The overall prevalence of Vitiligo worldwide ranges between 0.5% to 1 %. [2]
The currently employed conventional management modalities include steroids, Interlukin-2 inhibitors and phototherapy. Eventhough medical management is the primary mainstay treatment modality, it is only effective in about 60 % to 70% of the cases. [3] In view of these shortcomings, surgical management was introduced in 1964 and from there we have come a long way in grafting techniques ranging from tissue grafts to grafting at the cellular level. The most important advantage of cellular grafting over tissue grafting is that it can be used to treat affected areas which are much larger than the donor site. [4]
Non-cultured Cell Epidermal Suspension (NCES) is a newer modality of surgical grafting which needs to be further explored.
Materials and Methods
This study is a prospective study conducted at the department of Dermatology, Venerology and Leprosy of Rajah Muthiah Medical College and Hospital, Chidambaram during the period between October 2018 to October 2020. Ethical clearance was sought from the Institutional Ethical Committee. 26 cases of stable vitiligo who did not respond to conventional medical management were included for the study. The exclusion criteria for this study included patients with unstable vitiligo, keloidal conditions and coagulopathies. Complete blood count, renal parameters, blood sugar were done before surgery.
Preparation of the cell suspension
Under strict sterile aseptic conditions split skin graft was harvested from the medial thigh with a Humby’s knife. The graft obtained is cleansed with saline and exposed to trypsin and kept in an incubator at 37 degree Celsius for 45 minutes. The resulting graft is neutralized with anti-trypsin and agitated to separate the epidermis and dermis. The cellular graft obtained is treated with DMEM solution and kept in a centrifuged at 3500 rpm for 15 minutes and the pellet is obtained.
Transferring the graft onto the recepient site
The recipient site was prepared by debrading the dermis superficially either manually or by a dermabrador. Satisfactory debrading was said to be achieved when pin-point bleeding was seen. The graft harvested is applied over the dermabraded site following which dry collagen sheets are applied over it. Patients are advised immobilization for a period of one hour following surgery and were subsequently asked to restrict mobilization for a period of one week. Patients were given prophylactic antibiotics, analgesics and NSAID’s for a period of one week.
Follow Up
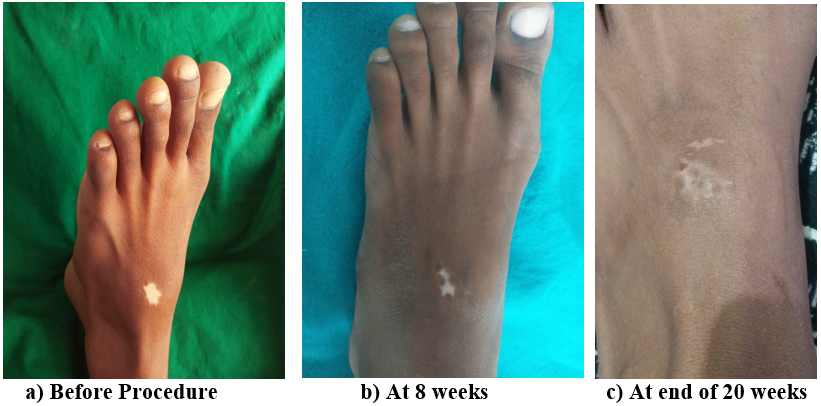
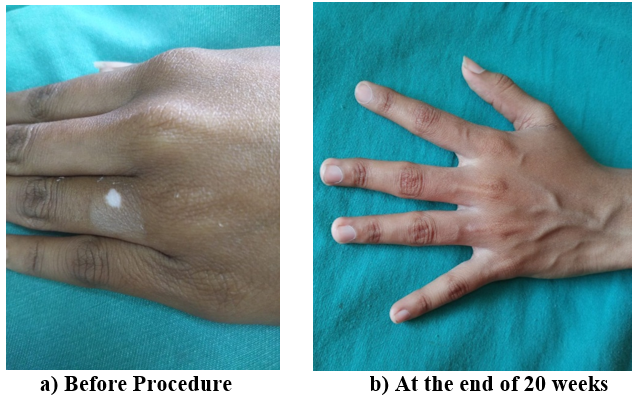
The patients were asked to review on the 8th postoperative day, followed by 2 weeks and 4 weeks and subsequently on a monthly basis. At every visit patients were checked for evidence of repigmentation, donor site complications and to make sure that the patient is not under any other medications. Photographs were taken prior to the procedure, intraoperatively and at each visit postoperatively. Results were assessed at 4 weeks, 8 weeks, 12 weeks, 16 weeks and 20 weeks. The repigmentation status was assessed using the Visual analogue system score which was classified as 0-24% = very poor, 25-49%= poor, 50-74%= fair, 75-89%= good and >90% = excellent.
Results
Most of the patients had a focal patch of vitiligo. The highest number of vitiligo lesions were found on the lower limb followed by upper limb, followed by trunk and face. The site from which the graft was harvested re-epithelialised within 10 days and no further dressing was needed. In our study, at the end of 20 weeks, out of 26 cases, 9(34.6%) cases showed excellent repigmentation. Good repigmentation were seen in 7 cases (26.9%) and fair repigmentation in 5 cases (19.3%). Poor repigmentation in 2 (7.7%) cases and very poor in 3 (11.5%) cases. In around 16 (61.5%) cases repigmentation started at 8 weeks post NCES and in 8 (30.8%) cases repigmentation started at around 4 weeks. 3(11.5%) cases showed very poor repigmentation of which 2(7.7%) showed absolutely no pigmentation at all even at the end of 20 weeks. All the cases which is repigmented in our study shown diffuse types of repigmentation. Of the 17 cases which showed more than 75% repigmentation, 15 cases (88%) showed even pigmentation similar to surrounding skin while 2 cases (7.7%) showed hyperpigmentation.
|
Percentage of re-pigmentation |
4 week |
8 week |
12 week |
16 week |
20 week |
|
No pigmentation |
2 (7.7%) |
2 (7.7%) |
2 (7.7%) |
2 (7.7%) |
2 (7.7%) |
|
< 25 (Very poor) |
21 (80.8%) |
10 (38.5%) |
1 (3.8%) |
1 (3.8%) |
1 (3.8%) |
|
25-49 (Poor) |
3 (11.5%) |
10 (38.5%) |
3 (11.5%) |
2 (7.7%) |
2 (7.7%) |
|
50-74 (fair) |
0 |
4 (15.4%) |
16 (61.5%) |
6 (23.1%) |
5 (19.3%) |
|
75-89 (Good) |
0 |
0 |
4 (15.4%) |
10 (35.5%) |
7 (26.9%) |
|
90-100 (excellent) |
0 |
0 |
0 |
5 (19.2%) |
9 (34.6%) |
|
Total |
26 (100%) |
26 (100%) |
26 (100%) |
26 (100%) |
26 (100%) |
|
p value |
0.001 |
Discussion
Vitiligo is the most common depigmentation disorder and it is generally acquired and of idiopathic origin. It is mainly defined by its sharp areas of depigmentation which are of different sizes and shapes. Although various modalities of management, both medical and surgical, are available, no modality has so far been successful. An ideal procedure is one which not only provides adequate repigmentation but also has minimal or zero donor site complications with special mention to permanent scarring. Non cultured epidermal cell suspension is a single-time daily care procedure. It allows for treatment of a depigmented area far greater in size than the donor site. [5] It was introduced in 1992 by Gauthier and SurleveBazeille. [6] Ever since its inception this technique has undergone many modifications. Multiple studies at various centres by Van Geel N et al. [7] and Mulekar et al. [4] have emphasized Non cultured cell epidermal cell suspension has the gold standard for the stable form of Vitiligo. This article is our experience of this novel modality in patients with stable vitiligo. In our study, at the end of 20 weeks, out of 26 cases, 9(34.6%) cases showed excellent repigmentation. Good repigmentation were seen in 7(26.9%) and fair repigmentation in 5 cases (19.3%). Poor repigmentation in 2(7.7%) cases and very poor in 3(11.5%) cases. In around 16(61.5%) cases repigmentation started at 8 weeks post NCES and in 8(30.8%) cases repigmentation started at around 4 weeks. 3(11.5%) cases showed very poor repigmentation of which 2 showed absolutely no pigmentation at all even at the end of 20 weeks. This study was comparable to the study conducted by N.Geel et al [7] who observed 70% repigmentation at the end of 20 weeks. The highest rates of repigmentation was reported by Singh C et al. [8] who demonstrated 92% of cases with more than 75% repigmenattion. Even though our study could not achieve these rates, we could still achieve more than 65% of cases with repigmentation rates of greater than 75%.
The advantage of this novel technique is that it produces even pigmentation similar to that of surrounding skin which was the major disadvantage with most tissue based grafts.
The author feels that the major learning curve in this modality would be the accuracy of harvesting a epidermal graft without causing substantial donor site morbidity.
Source of Funding
No financial support was received for the work within this manuscript.
Conflict of Interest
The authors declare they have no conflict of interest.
.
References
- Glassman S. Vitiligo, reactive oxygen species and T-cells. Clin Sci. 2011;120(3):99-120. [Google Scholar] [Crossref]
- Taïeb A, Picardo M, . The definition and assessment of vitiligo: a consensus report of the Vitiligo European Task Force. Pigment Cell Res. 2007;20(1):27-35. [Google Scholar] [Crossref]
- Prasad D, Gupta S. Standard guidelines of care in vitiligo surgery. Indian J Dermatol Venereol Leprol. 2008;74:37-45. [Google Scholar]
- Geel N, Goh B, Wallaeys E, Keyser S, Lambert J. A review of non-cultured epidermal cellular grafting in vitiligo. J Cutan Aesth Surg. 2011;4(1):17-22. [Google Scholar] [Crossref]
- Paul M. Autologous Non-cultured Basal Cell-Enriched Epidermal Cell Suspension Transplantation in Vitiligo: Indian Experience. J Cutan Aesthet Surg. 2011;4(1):23-8. [Google Scholar]
- Gauthier Y, Surleve-Bazeille JE. Autologous grafting with noncultured melanocytes: A simplified method for treatment of depigmented lesions. J Am Academy Dermatol. 1992;26(2):191-4. [Google Scholar] [Crossref]
- Geel Nv, Ongenae K, Mil MD, Haeghen YV, Vervaet C, Naeyaert JM. Double-blind Placebo-Controlled Study of Autologous Transplanted Epidermal Cell Suspensions for Repigmenting Vitiligo. Arch Dermatol. 2004;140(10):1203-8. [Google Scholar] [Crossref]
- Singh G, Ansari Z, Dwivedi RN. Letter: Vitiligo in ancient Indian medicine. Arch Dermatol. 1974;109(6). [Google Scholar]
How to Cite This Article
Vancouver
Azharudeen M, Kaviarasan PK, K K, B P, C A. A prospective study to evaluate the repigmentation in vitiligo after noncultured epidermal cell transplant followed by puva [Internet]. IP Indian J Clin Exp Dermatol. 2020 [cited 2025 Oct 09];6(4):325-327. Available from: https://doi.org/10.18231/j.ijced.2020.065
APA
Azharudeen, M., Kaviarasan, P. K., K, K., B, P., C, A. (2020). A prospective study to evaluate the repigmentation in vitiligo after noncultured epidermal cell transplant followed by puva. IP Indian J Clin Exp Dermatol, 6(4), 325-327. https://doi.org/10.18231/j.ijced.2020.065
MLA
Azharudeen, Mohammed, Kaviarasan, P K, K, Kannambal, B, Poorana, C, Abhirami. "A prospective study to evaluate the repigmentation in vitiligo after noncultured epidermal cell transplant followed by puva." IP Indian J Clin Exp Dermatol, vol. 6, no. 4, 2020, pp. 325-327. https://doi.org/10.18231/j.ijced.2020.065
Chicago
Azharudeen, M., Kaviarasan, P. K., K, K., B, P., C, A.. "A prospective study to evaluate the repigmentation in vitiligo after noncultured epidermal cell transplant followed by puva." IP Indian J Clin Exp Dermatol 6, no. 4 (2020): 325-327. https://doi.org/10.18231/j.ijced.2020.065
