Introduction
Vitiligo is an autoimmune disorder of pigmentation in which there is loss of functional melanocytes and melanin in the epidermis.1 It affects only 0.5-2% of world’s population with no ethnic or gender predilection. In normal individuals, the skin has a typical reticulate pigmentary pattern which corresponds to pigmentation along the rete ridges and pale areas signifying papillary dermis. 2 The reticulate pigmentary pattern of normal skin is altered in the lesions of vitiligo; 3 hence the dermoscopic examination is found helpful in the early diagnosis of the disease and is reversed in evolving lesions of vitiligo. 4
Various patterns observed on dermoscopy in lesions of vitiligo are:
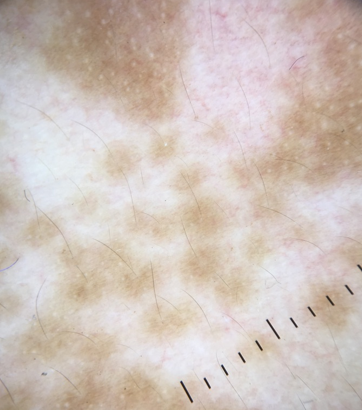
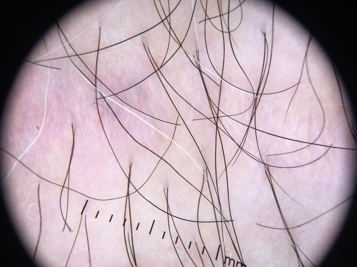
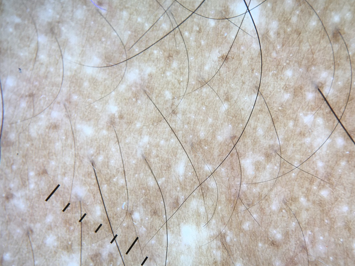
Perifollicular pigmentation (Figure 1)
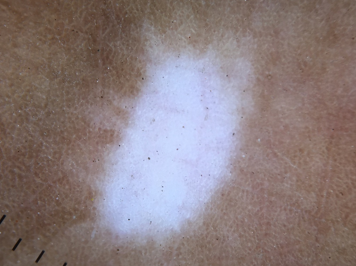
Perilesional/marginal hyperpigmentation (Figure 2)
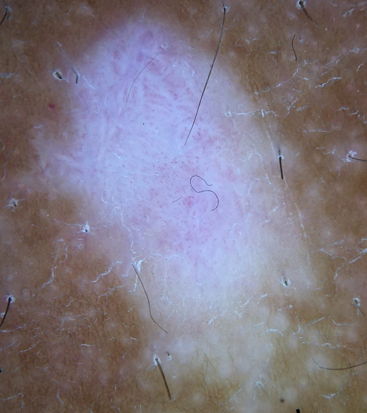
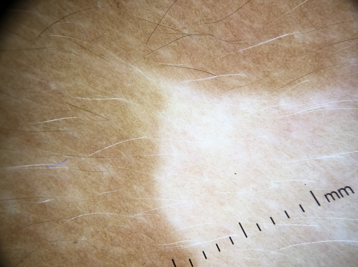
Intra/perilesional erythema with telangiectasia (Figure 3)
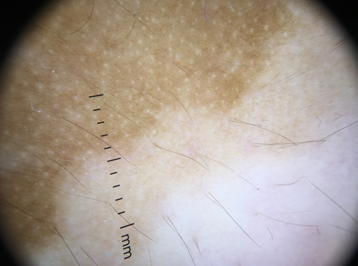
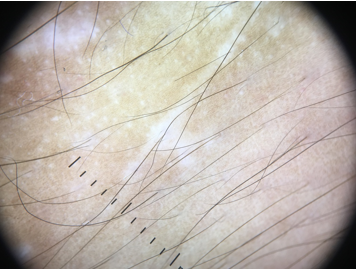
Perifollicular depigmentation (Figure 4)
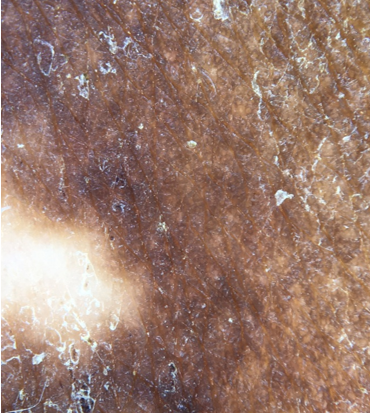
Trichrome pattern (Figure 5)
Leukotrichia (Figure 6)
Starburst appearance (Figure 7)
Comet tail appearance (Figure 8)
Micro koebner phenomenon (Figure 9)
Tapioca sago appearance (Figure 10)
Some dermoscopic patterns were found overlapping in the different lesions of the same patient. Stability in vitiligo is an important concept guiding direction of patient management. Dermoscopy might be useful to assess the evolution of stage of the disease (stability, progression, repigmentation) as well as the response to treatment. Current study is aimed to understand the various dermoscopic patterns present in vitiligo and its correlation with the stability of the disease.
Materials and Methods
Clinically diagnosed 50 patients of vitiligo were studied during a period of January 2019 – December 2019; which included both stable and unstable cases.
The criteria used to confirm stability of vitiligo included:
Absence of progression of old lesions since past 2 years.
No new lesions during the same period.
No history of recent koebner phenomenon.
Repigmentation affected areas by medical treatment.
This was an observational study. Detailed and informed consent was taken from the patient. detailed history was inquired and clinical and dermoscopic examination was performed maintaining the confidentiality of the patient. Dermlite DL4 dermoscope (10x) was used for magnification and pictures were captured using Apple iPhone SE (Figure 11). Findings were summarized and the dermoscopic data was analyzed using the Fisher’s exact test.
Inclusion criteria
Diagnosed patients of clinically stable and unstable vitiligo including patients on treatment.
Results
Among the clinically diagnosed 50 cases of vitiligo, most of them belong to age group of 15-30 years with no gender bias.
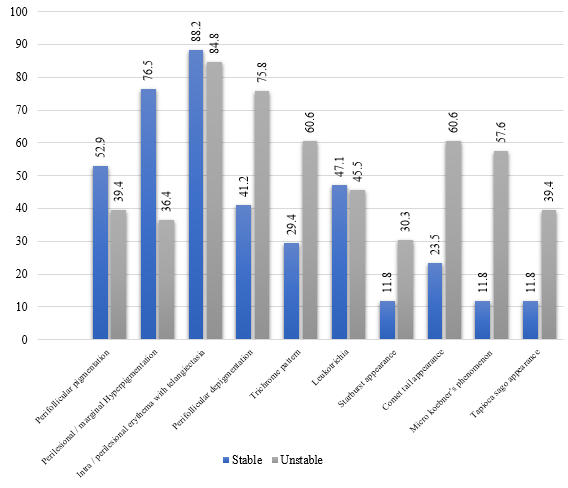
Out of 50 patients of vitiligo, 17 were of stable vitiligo while 33 were of unstable vitiligo. Dermoscopic patterns observed were perifollicular pigmentation (22 cases), perilesional/marginal hyperpigmentation (25 cases) and intra/perilesional erythema with telangiectasia (43 cases), perifollicular depigmentation (32 cases), trichrome pattern (25 cases), leukotrichia (23 cases), starburst appearance (12 cases), comet tail appearance (24 cases), micro koebner’s phenomenon (21 cases) and tapioca sago appearance (14 cases) were seen.
In clinically stable vitiligo (n=17), the most common significant finding observed was perilesional/marginal hyperpigmentation (p=0.016). Perifollicular pigmentation and intra/perilesional erythema with telangiectasia though are findings of stable disease, were observed in both stable and unstable disease in similar numbers.
In unstable disease (n=33), perifollicular depigmentation was the most common finding observed (p=0.028), while other significant findings (p<0.05) observed were trichrome pattern, comet tail appearance, micro koebner’s phenomenon and tapioca sago appearance. Leukotrichia and starburst appearance were present in both stable and unstable disease despite being the findings of unstable disease.
Table 1
Dermoscopic findings and its P value.
Discussion
In normal individuals, the skin has a typical reticulate pigmentary pattern which corresponds to pigmentation along the rete ridges and pale areas signifying papillary dermis. 2 The reticulate pigmentary pattern of normal skin is altered in the lesions of vitiligo. 3 It is difficult to distinguish the initial lesions of vitiligo clinically from other causes of hypopigmentation and depigmentation. Dermoscopic examination can detect minute changes in the pigmentary pattern which are not visible to naked eyes, helping in the early diagnosis of vitiligo. 3 The characteristic finding considered signifying focally active or repigmenting vitiligo is a pattern of depigmentation with residual reservoirs of perifollicular pigment. 5 The patient of vitiligo is diagnosed primarily clinically without the need of any diagnostic tools. However, non-invasive tests like dermoscopic evaluation are helpful:
When diagnosis is doubtful e.g. in evolving disease.
For objective evaluation of treatment response.
Dermoscopy (digital epiluminescence microscopy or "dermatoscopy") magnifies the clinical image manifold (10x) and allows appreciation of subtle features invisible to the naked eye. Chuh and Zawar described its use as an early diagnostic tool for localized vitiligo, in which they reported a pattern of depigmentation with residual reservoirs of perifollicular pigment being characteristic.5 In our study out of 50 cases of vitiligo, 17 were of stable vitiligo while remaining 33 were of unstable disease. In stable disease, perifollicular pigmentation was seen in 9 patients, perilesional/marginal hyperpigmentation in 13 cases and intra/perilesional erythema with telangiectasia in 15 cases. In unstable vitiligo, perifollicular depigmentation was present in 28 patients, trichrome pattern in 20 cases, leukotrichia in 15 cases, starburst appearance in 10 cases, comet tail appearance in 20 cases, micro koebner’s phenomenon in 19 cases and tapioca sago appearance in 12 cases. Meng et al. observed 176 patients with different types of depigmentation out of which 97 had vitiligo.6 They observed residual perifollicular pigmentation in 57 of 62 patients with unstable vitiligo and 22 of 35 in those with stable vitiligo. However, residual perifollicular pigmentation was non seen in the 79 patients with non-vitiligo depigmentation. Their study varied from ours, they included all types of vitiligo (evolving, stable and devolving) as well as other causes of hypopigmentation and depigmentation. Our study was focused on identifying dermoscopic signs in all the lesions of vitiligo.
According to our study, perilesional/marginal hyperpigmentation is the most common finding present in stable disease while perifollicular depigmentation was the most commonly seen in unstable vitiligo.
Conclusion
To conclude perifollicular pigmentation and perilesional/marginal hyperpigmentation, suggest stability and patterns like trichrome pattern, starburst appearance, comet tail appearance, tapioca sago appearance suggest unstability. Hence, we conclude that dermoscopy can be used as an aid to monitor the disease activity and hence prognosis of the disease. Some patterns like trichrome, tapioca sago, starburst, comet tail suggest the change in treatment modality.