Introduction
Sexually transmitted diseases (STDs) are a group of communicable diseases that are transmitted predominantly by sexual contact and are caused by a wide range of bacterial, viral, protozoal and fungal agents and ectoparasites. The Centres for Disease Control and Prevention (CDC) estimates that there are approximately 20 million new STD infections each year, almost half of them among young people aged 15 to 24.1
The general public is largely unaware of the health consequences of STDs. STDs are hidden epidemics for various reasons – most STDs initially are often asymptomatic and thus go undetected. Major health consequences, such as infertility, certain cancers, and other chronic diseases, occur years after the initial infection, so there is a lack of awareness of any link to the original STD. Also, the stigma associated with having a STD inhibits adequate public discussion and education.
It is imperative to understand the current trends of STDs in various parts of our country in order to plan and implement various strategies to combat this problem. Even today, in spite of new diagnostic techniques having been introduced so as to improve the diagnostic yield of various STIs, the assessment and management of patients is still largely based on syndromic approach given by the National AIDS Control Organization (NACO) owing to lack of resources in majority of the health care centres.
The present study aims to understand the pattern of non-retroviral STDs in patients attending Dermatology department in a tertiary care hospital in North east India.
Materials and Methods
This is a hospital based study which was conducted over a period of 12 months from July 2019 to June 2020 to find the pattern of non-retroviral STDs in patients attending Dermatology department of Silchar Medical College and Hospital, Silchar, Assam. In the given period, all patients who presented to the Dermatology department with sexually transmitted diseases were evaluated after due consent, with relevant and detailed clinical history and examination. Data such as demographic information – age, marital status, sexual orientation, complaints at the time of presentation, duration of complaints and any treatment taken for the complaints were collected at the first visit. The diagnosis was confirmed with relevant laboratory investigations. Patients with positive retroviral serology were excluded from the study. Thus, 248 patients were included in the study. Gram stain was done in all cases of urethral discharge. KOH preparation and wet mount examination were done wherever required. Venereal disease research laboratory (VDRL) by Rapid plasma reagin test (RPR) test was done in necessary cases. If VDRL test was positive, it was confirmed by Treponema pallidum haemagglutination (TPHA) test. A syndromic and clinical diagnosis was made on the basis of clinical features and laboratory investigations. Treatment was provided to the patient as per NACO’s guidelines. Partner notification and condom promotion were done.
Results
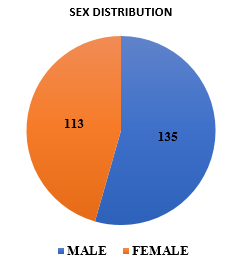
During the one-year study period, out of the total 41,797 patients who attended Dermatology department, 248 patients presented with non-retroviral sexually transmitted diseases. Thus, the overall incidence was found to be 5.93 per 1000 patients attending Dermatology department. Out of the total number of patients, 135(54.43%) were male and 113(45.57%) were female. Male to female ratio was 1.19:1. Majority of the patients were from urban background (84.7%) while the rest (15.3 %) were from rural area. Most of the males were daily wage workers (66.66 %), followed by farmers (22.22%) and private firm employees (11.11%). Majority of the female patients (61.94%) were homemakers. Most of the cases were seen in 21- 30 years age group accounting for 116 cases (46.77%).
200 (80.64%) patients in the study were married while 48 (19.35%) were unmarried. Most patients (95.9%) gave history of heterosexual contact while 10 patients (4.03%) gave history of homosexual contact. Only 80.65 % patients regularly used barrier contraception. A total of 50 males (20%) confessed to having had contact with sex workers. Patients who could sign and were able to read were considered as literates. 2 Around 70 % of the patients were literate.
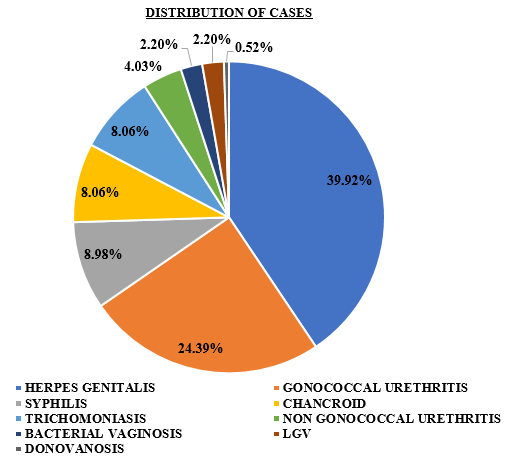
Maximum number of cases were herpes genitalis (39.92%), followed by gonococcal urethritis (24.39%) and syphilis (8.98%). 8.06% cases had chancroid and trichomoniasis respectively. 4.03% were suffering from non- gonococcal urethritis. 2.20 % had bacterial vaginosis and Lymphogranuloma Venereum (LGV) each. Donovanosis was seen in 0.52 % of the patients.
Discussion
“Venereal disease is the most formidable enemy of the human race; an enemy entrenched behind the strongest human passions and deepest social prejudice.” - Sir William Osler.3 The physical,mental and social burden caused by STDs is tremendous. They have very dynamic epidemiological changes and it is imperative that these changes are kept track of, especially in a huge and populous nation like India.
A number of epidemiological studies have been done on the pattern and changing trends of STDs.4, 5
In the present study, maximum cases were seen in 21- 30 years age group. This is similar to studies done by Kavina BK et al, Murugesh SB et al and Chandra Gupta et al.6, 4, 5 This age group is probably more vulnerable to STD acquisition as they generally show higher sexual activity, increased inherent curiosity, higher number of sexual partners and more change of partners than the older age groups.
In our study, the male: female ratio was found to be 1.19:1. In a study by Mehta B, male to female ratio was found to be 4.55:1.7 The number of female patients being less could be due to social and cultural restrictions, the asymptomatic nature of disease in females and that many of them prefer to attend gynaecology department.
In our study, most of the males were daily wage workers (66.66%), followed by farmers (22.22%) and private firm employees (11.11%). Majority of the female patients (61.94%) were homemakers. This is similar to the results of study by Banger et al. 8
In this study, most common STD found was herpes genitalis, followed by gonococcal urethritis and syphilis. This is similar to the findings in the study conducted by Jain et al., where herpes genitalis was found to be the commonest STI.9 In another study by Nayyar C et al, the most common STD was found to be chlamydial urethritis (8%), followed by gonorrhoea (7.5%). 10
The most important strategy to achieve effective control of STDs is prevention. Higher literacy rates, introducing formal sex education in the school curriculum and mass education about safe sex practices including avoidance of promiscuity and regular use of barrier contraceptives are some of the methods for primary prevention. Secondary prevention, that is early diagnosis and treatment is especially important in order to reduce further morbidity and overall disease burden.
Conclusion
The present study was an attempt to provide an insight and overview about the pattern of non-retroviral STDs in patients attending Dermatology department in a tertiary care hospital in North east India. A comprehensive understanding of the various STDs and their aetiology and presentation is essential to avoid their much preventable long-term sequelae relentless efforts must be made to raise awareness and educate the general population about these diseases. Focussed counselling sessions, contact tracing and prompt management of the partners are also integral parts of treatment.