Introduction
The World Health 0rganization 2020 report estimates that there are about 9.96 million new cases of tuberculosis (TB) each year and the deaths due to TB is estimated to be 1.4 million each year.1 It is an ancient disease and for more than 4,000 years has affected mankind. In developing countries it is one of the leading cause of morbidity and mortality, about 7% of all deaths are attributed to TB.2 A group of closely related bacterial species termed Mycobacterium tuberculosis complex causes TB and the principal cause of human tuberculosis is Mycobacterium tuberculosis. Other members of this complex are M. bovis, M. microti and M. africanum.3
Among the extra-pulmonary tuberculosis which is about 8.4-13.7% of all tuberculosis cases cutaneous tuberculosis is relatively uncommon and comprises of 1-1.5%. The prevalence of cutaneous TB in Indian children varies from 18 to 54%.4 Cutaneous TB manifestations are varied and typical dermatologic lesions are rarely seen. Cutaneous tuberculosis can present with unusual histopathological features and the bacteria is seldom identified by stain or culture causing difficulty in diagnosis. So cases are diagnosed based on strong clinical suspicion, family history of pulmonary/extrapulmonary TB, a positive Mantoux test and typical histopathological features. 5 The current study was aimed to describe various clinical pattern of cutaneous tuberculosis in children of paediatric age group attending a tertiary health centre.
Materials and Methods
Setting
The study was carried out in the Department of Dermatology at Silchar Medical College and Hospital, Assam.
Sample size
Total 11 diagnosed cases of cutaneous tuberculosis are included in study attending Silchar Medical and Hospital during study period.
Study Procedure
Cutaneous TB patients of age 1year to up to 13 year, satisfying the inclusion and exclusion criteria were included in the study. Their parents were informed about the purpose and nature of study and after obtaining written informed consent from them, demographic data, a detailed clinical history, family history of contact with TB disease, and physical examination for each child was recorded in a standardized format. Complete blood count, Mantoux test, Chest X-ray, histopathological examination and Ultrasound whole abdomen were done for all the cases. In Mantoux test induration of more than 10 mm was taken as suggestive of infection with Mycobacterium tuberculosis in non-vaccinated patients and 15 mm and above was taken in vaccinated child. All diagnosed patient of Cutaneous TB were put on directly observed treatment short course (DOTS) of anti-tuberculosis treatment under RNTCP (Revised National Tuberculosis Control Program).
Results
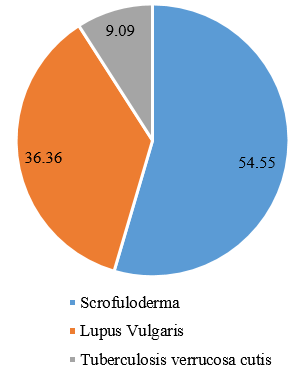
In the current study, 11 children with cutaneous tuberculosis were analysed to explore the clinical pattern of cutaneous TB. Out of them maximum 45.45% patients were within 11-13 years age followed by 6-10 years 36.35% and least 1-5 years 18.18%. The mean age of the patients was 9.63 years. The male is to female ratio was found to be 4.5:1. Commonest type of Cutaneous TB in the study population was scrofuloderma (54.55%), followed by lupus vulgaris (36.36%), and tuberculosis verrucosa cutis (9.09%). Lower limb involvement was commonest followed by involvement of neck.
Table 1
Cutaneous TB; Types and sites of presentation
|
Cutaneous TB type |
Site |
Number of cases |
Total cases |
|
Scrofuloderma |
Neck |
3 |
6 |
|
Axillae |
3 |
||
|
Lupus Vulgaris |
Lower Limb |
3 |
4 |
|
Upper Limb |
1 |
||
|
TBVC |
Lower Limb |
1 |
1 |
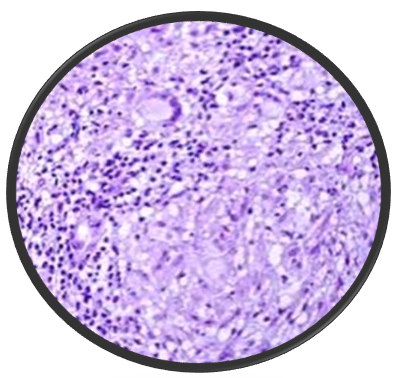
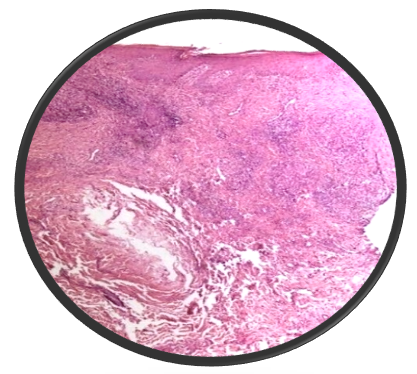
Majority of the patient presented with single lesion (72.73%) and the rest (27.27%) had involvement of multiple sites. All of the patient were from poor social strata. Lymph node involvement was seen in all 6 cases of scrofuloderma (54.55%) cases. Histopathology was consistent with cutaneous tuberculosis in all of the cases. Mantoux test was positive in 9 of the cases (81.82%). BCG vaccination was done in 8(72.72%) of the cases. 2 cases had positive family history of TB. None of the cases had systemic involvement of other organs.
Discussion
In this study the total number of patients included were 11.The male to female ratio was found to be 4.5:1 and the preponderance of infection in male is in accordance to study done by Muley P et al where the M:F ratio was 1.53:1. This could be because of the fact that male child are more ambulatory and in a developing country like India more attention paid to male child could also be the reason.6
Most of the cases belong to the age group 11 to 13 years (45.45%) which was also seen in study done by Sultana A et al where 46.7% patient were in age group 11-15 years.7 The most common cutaneous TB was scrofuloderma (54.55%), followed by lupus vulgaris (36.36%), and tuberculosis verrucosa cutis (9.09%). Scrofuloderma is the direct extension from an underlying tubercular focus, most commonly tubercular lymphadenitis or skeletal tuberculosis into the skin. They clinically presents as ulcerated lesions in the neck with discharging ‘cheesy’ material Scrofuloderma is found to be the most common and lupus vulgaris the second most common cutaneous TB in children in studies done by Singal A et al, Vashisth P et al and Sethuraman G.8, 9, 10
Study showed that all the patients 100% were from low socio-economic condition.11 A positive family history of tuberculosis was associated in 2 of the cases (18.18%) in our study as similar to study done by Panda M et al where it was13.64%.12 The most common site of cutaneous tuberculosis was lower limb in our study this was also seen in study done by Panda M et al.12
Conclusion
Cutaneous TB has varied clinical presentations and generally occurs due to direct inoculation into skin or sometimes due to underlying focus of infection. Therefore, high clinical suspicion is required to diagnose the case. Since children especially male child are more ambulatory they have greater incidence of cutaneous TB compared to adults and also the immune status of children is not well-developed. A rising incidence of cutaneous tuberculosis is a marker of active infection in the community. Early diagnosis based on strong clinical suspicion will help initiate early diagnosis and successful treatment. Thus to accomplish this the present study was undertaken.