Introduction
Skin being the largest organ of the body, is subjected to constant environmental insults through various direct and indirect targets. This explains the vast number of diseases that can occur in skin and these cutaneous lesions can be categorized broadly as non-neoplastic and neoplastic diseases. By far, non-neoplastic lesions outweigh the number of neoplastic lesions in the practice of clinical dermatology. Due to the varied presentations of these non-neoplastic lesions, and the myriad of diseases categorized under them, it is understood that an expertise knowledge is required for an accurate diagnosis.1, 2, 3 Hence this study was undertaken with an intention to learn various cutaneous non-neoplastic lesions which were submitted for histopathological analysis by a simple minimally invasive punch biopsy procedure.
Aims & Objectives
To describe the various non-neoplastic lesions of skin with respect to their demographical profile and to categorize them based on histopathological patterns.
Materials and Methods
A two year retro-prospective cross-sectional study was undertaken in a tertiary care medical college hospital from 1st of January 2018 till 31st of December 2019, in the Department of Pathology. Institutional ethical clearance was obtained prior to the commencement of the study. Patients with skin diseases which required histopathological diagnosis were subjected to a 4mm punch biopsy procedure done at an out-patient setup in the Department of Dermatology & Venereology. The tissues obtained were fixed immediately in 10% formalin and sent to the Department of Pathology for histopathological analysis. Biopsies were processed routinely in an automated tissue processing and embedding system. Sections were cut at 3-4 micrometer thickness using a semi-automated microtome and stained by routine Hematoxylin and Eosin stain. Special stains were done when and where required. Demographic parameters were obtained from the case records. All punch biopsy specimens which were diagnosed as non-neoplastic skin diseases of any age group were taken as inclusion criteria. Those cases which were subjected to non-punch biopsy procedures which even though had a non-neoplastic pathology were excluded from the study. Sample size of 82 cases were studied in a period of 2 years. Simple descriptive statistics was applied after computing the collected data in Microsoft Excel software.
Results
Out of the 82 cases studied, 46(56%) were males and 36(44%) were females, with a male to female ratio of 1.27:1. (Figure 1a). Age wise distribution is represented in (Figure 1 b). Maximum number of cases (n=23) were seen in 21-30 years of age which corresponded to 28% of the total cases. Youngest patient’s age was 5 years, while the oldest one was 69 years. Most prominent site of lesions biopsied were from lower limb (23 cases) with legs being the commonest among them (9 cases).
Cutaneous infections (n=25) was the most common clinical category, with mycobacterial lesions as the prominent subcategory (n=16). Out of these 16 cases, the most prominent cases were of leprosy (n=10), with their varied presentations in histology. Among these 10 cases, 7 cases were biopsied in young patients of 21-30 age group, out of which 6 of these patients were males. The M:F ratio of leprosy patients subjected to punch biopsies was 7:3. Eight of ten cases showed granulomatous lesions in histology, among which 6 cases were diagnosed as Borderline Tuberculoid leprosy and 2 were categorized as Tuberculoid leprosy. The other two out of ten leprosy cases showed lepromatous pattern with diffuse infiltrate of foamy macrophages. Acid fast bacilli were noted in 8 out of 10 cases of leprosy.
Out of 25 cases of cutaneous infections, eight cases were due to viral infections, 7 of which manifested as verrucous proliferations, either as verrucous hyperplasia or verruca vulgaris. Interestingly, 6 of those cases were noted in males in varying age range, and 5 of such cases occurred in foot/palms presenting clinically as warty outgrowths. One case of verrucous hyperplasia was observed in nose. Histopathologically all these cases were observed to possess koilocytotic keratinocytes and verruciform hyperkeratosis. One case of HIV infection presented with multiple skin colored itchy papules with central crusting was noted in upper limb of 35-year-old male, which was diagnosed histopathologically as pruritic papular eruption. One case of cutaneous leishmaniasis was noted as generalized erythematous papulonodular lesions with shiny surface, histology of which showed leishmanial organisms in macrophages.
There were 6 cases of Mycobacterium Tuberculous infection, all were diagnosed histopathologically as Lupus vulgaris. Face was most common site of occurrence of Lupus vulgaris with 2 cases each in cheek, and nose, one in paranasal skin, and one in upper limb. Clinically these lesions were erythematous in nature with two cases presenting as plaques with central clearance whereas the other two cases presented as papulonodular lesions. Histopathologically all these cases were composed of granulomatous reaction pattern, which were confirmed by Ziehl Neelson’s acid fast staining for Mycobacterial organisms.
Out of 82 cases, 14 cases were clinically categorized purely into papulo-squamous in nature, while 3 cases were having mixed clinical patterns. Out of these 14 cases, predominant spongiosis pattern was observed in 8 cases, lichenoid pattern was noted in 5 cases, and a single case of psoriasiform reaction pattern. Among the 8 cases with spongisosis, 3 cases had pityriasiform spongiosis, with pityriasis rosea as the commonest disease among them. Erythematous patches to nodules were the commonest clinical presentation of pityriasis rosea Other 5 cases of spongiosis were allergic contact dermatitis(n=1) and small plaque parapsoriasis (n=4). Five cases of lichenoid reaction pattern were recorded, with classic lichen planus, lichen planus pigmentosus, annular lichen planus, hypertrophic lichen planus, and systemic lupus erythematosus each contributing to one case each. Out of these 5 cases, former 4 cases were noted in 3rd decade and all of them had hyperpigmentation with itchy macules to plaques in their clinical presentation, while latter one case of systemic lupus erythematosus was noted in 2nd decade in a male patient interestingly. One case of psoriasis was noted, clinically presenting as generalized erythroderma in a 53-year-old male patient, biopsy of which revealed classic features of psoriasis such as regular elongation of rete pegs with micro-munro neutrophilic abscesses.
Three cases had a mixed pattern of presentation, as lichenoid together with spongiotic patterns (Lichenoid contact dermatitis, prurigo nodularis and prurigo simplex), all of which had multiple lesions associated with itching and hyperpigmented macules to nodules on clinical presentation.
Of the 82 cases, 9 cases had predominantly vasculopathic reaction pattern in histopathology, manifesting clinically as cutaneous vasculitis. Some of the vasculitis biopsied were hypersensitivity vasculitis (n=5), urticarial vasculitis (n=2), small vessel vasculitis and chronic lymphocytic vasculitis (each n=1). All cases of hypersensitivity vasculitis were diagnosed to be leucocytoclastic vasculitis on histopathology, with 4 of them presenting as purpurae while one was presenting as petechiae clinically. Multiple erythematous and edematous papules/plaques was the most common presenting symptom of urticarial vasculitis. One case of erythema elevatum diutinum in a 28-year-old male presented to have multiple tender erythematous fleshy plaques in his forearm. A case of pyoderma gangrenosum was noted in a 45-year-old male as multiple hyperpigmented crusted plaques in his forearm. Histopathologically it was evident to have lymphocytic vasculitis with focal epidermal necrosis.
Vesiculo bullous diseases constituted 7 out of 82 cases, 5 of which occurred in females, with M:F ratio of 5:2. Most commonly diagnosed vesiculobullous disease was happened to be epidermolysis bullosa, one in 12-year-old female and other in 55-year-old male patient. The former patient had an inherited history of epidermolysis bullosa, while the latter was an acquired disease. Bullous pemphigoid, pemphigus vulgaris and sub-corneal pustular dermatosis were other blistering diseases (each n=1) exhibiting sub-epidermal, supra-basal and sub-corneal bullae respectively on histopathology. Two cases of Genodermatoses were encountered, one case was having multiple itching papules, pustules and crusts in axilla of 45-year-old male patient, while the other case was having cystic swelling in the lower lip of 33-year-old female patient. Both of which were diagnosed to be hailey-hailey disease and darrier’s disease respectively, by the presence of acantholytic cells in a dilapidated brick-wall pattern in the former while the latter had dyskeratosis with acantholysis, accompanied by corps ronds and grains.
Eight out of 82 cases had septal/lobular inflammation of the subcutaneous fat (histologically refers to panniculitis). All 6 cases out of 8 had predominantly septal distribution of inflammatory cells, while 2 cases had predominantly lobular inflammation. Clinically the former correlated to have erythema nodosum and latter, erythema induratum with nodular vasculitis. One of these cases of erythema nodosum had leprosy as clinical diagnosis, which was finally diagnosed to be erythema nodosum leprosum, after confirmation with acid fast stain for lepra bacilli. Exclusively all these cases of erythema occurred on limbs, especially on legs.
There were 7 cases of cutaneous appendageal disorders of which alopecia constituted the majority (n=6) in number. Out of these, idiopathic scarring alopecia (pseudo pelade of Brocq) consisted of 4 cases and non-scarring alopecia (alopecia areata) consisted of 2 cases. Most of these alopecias had common presentation of patchy hair loss and M:F ratio was found to be 1:2. The other appendageal disorder had erythematous follicular papules in skin of breast with discharge from the lesion, which was diagnosed histopathologically as Fox- Fordyce disease (Apocrine miliaria).
There were 9 cases of miscellaneous diseases, which included bowen’s disease (n=2), polymorphous light eruption (n=2), and single case of morphea, photodermatosis, lichenoid drug eruption, idiopathic macular eruptive hyperpigmentation and cutaneous lymphoid hyperplasia respectively.
Few cases of interest are depicted in the Figure 2 a-f.
Table 1
Categorization of Non- neoplastic diseases of skin with respect to broad clinical categories
Table 2
Classification of diseases based on Major Tissue reaction patterns.
Table 3
Classification of diseases based on Minor reaction patterns
Figure 1
a: Distribution of cases with respect to gender; b: Distribution of cases with respect to Age.
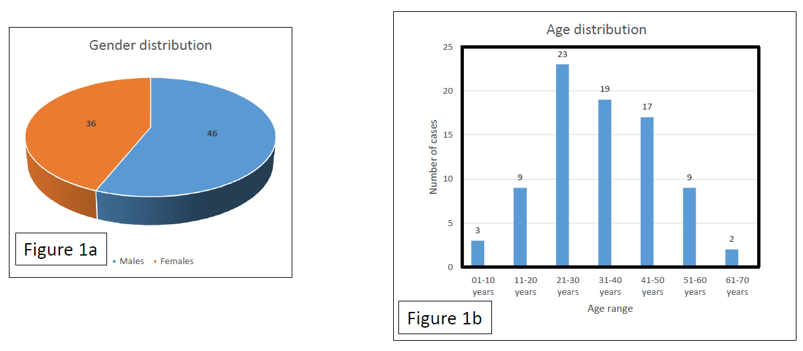
Figure 2
a: HaileyHailey disease, (acantholytic dyskeratosis with dilapidated brick wall pattern) (H&E; 40X); b: Darrier’s Disease, (prominent corps ronds & grains) (H&E; 100X); c: Pemphigus vulgaris suprabasal clefting and acantholysis (H&E;100X); d: Leucocytoclastic vasculitis, (leucocytoclasis with neutrophils & extravasation of fibrin) (H&E 100X); e: Lupus Vulgaris (well-formed epithelioid cell granulomas in dermis) (H&E 100X); f: Cutaneous Leishmaniasis, (Leishmanial Organisms in histiocytes) (H&E 400X)

Discussion
The present study was retro-prospective one with a total number of cases accounting to 82 in a period of 2 years. In a study by Veldhurthy VS et al, the total number of cases studied were 92, while study by Reddy et al accounted to 80 cases.4, 5 In a study by Singh et al a total of 112 cases were studied.6 The present study was conducted on 82 patients which was in par with most of the above mentioned studies in the literature. Forty-six cases (56.09%) were males and thirty six (43.9%) were females with M:F ratio of 1.27:1. This was similar to study by Singh et al, where 61 % of cases were males and Gupta et al where M:F ratio was 1.05:1.7 Considering age, present study shows maximum number of cases in 21-30 years of range (3rd decade, n=23 which accounted 28% of total number of cases), which was similar to Veldhurthy et al and Younas et al.8 Reddy et al & Gupta et al documented large number of cases in the 4th decade. Among the various sites, 23 cases fallen in the category of lower limbs with legs being the commonest of all. This was followed by upper limb, head and neck, multiple sites, trunk and perineum in the descending order respectively. This is in accordance with D’costa et al where lesions most commonly occurred in extremities.9
Considering the histopathological reaction pattern analysis, the most common major tissue reaction pattern was granulomatous in nature with a total of 17 cases, followed by spongiotic (n=8) vasculopathic (n=9) vesiculobullous (n=7) and lichenoid (n=5) respectively. In the study by Singh et al, granulomatous reactions constituted 2nd most common pattern analyzed, with 23.5% of cases, while in the study by Veldhurthy et al, 36.9% had lichenoid reactions which constituted the bulk of cases in them. In the study by Reddy et al, psoriasiform reactions constituted the maximum number of cases with 42.5% of cases followed by Lichen planus. The reason for decrease in number of biopsies of psoriasis and lichen planus compared to other studies is that, not all cases of clinically evident diagnosis were subjected to punch biopsy.
The presentation of large number of patients with infectious granulomatous reaction pattern may be attributed to the demographical and socio-economic status of Indian subcontinent, such as over-crowding, population explosion and improper hygiene in underdeveloped areas. Leprosy is still the most common cause of infectious granulomatous condition. Hypo-aesthesia is the prominent clinical symptom presented in 8 patients while the most common accompanying symptom was hypopigmentation. One case was presented with nerve thickening, which was identified to have an intra-neural granuloma on histology. Among individual cases, the maximum number of cases was shared by borderline Hansen’s (6 / 82) similar to Kumar et al and Lupus vulgaris (6/82), trailed by leucocytoclastic vasculitis (5/82).10 All those cases of lichenoid reaction pattern had either interface dermatitis or basal vacuolar change with inflammation as their histologic manifestations.
Among those less common diseases encountered, bowen’s disease had full thickness dysplasia of epithelium, both polymorphous light eruption and photodermatitis shared a common feature of phototoxic reaction to sunlight with subepidermal edema and vesiculation of epidermis along with inflammatory cells. Idiopathic macular eruptive hyperpigmentation had increased pigment in basal layer, pigmentary incontinence & perivascular lymphohistiocytic infiltrate.
Conclusion
Non–neoplastic lesions of skin include a vast array of disease categories and studying them in a methodical approach, like understanding the various histopathological reaction patterns and clinical categorizations with demographic profiles helps in arriving accurate diagnosis. Nevertheless, discussion with dermatologists is of utmost importance for understanding various clinical presentations of diseases with respect to specified tissue reaction patterns observed histopathologically and vice versa.
