Introduction
According to WHO a new-born infant, or neonate, is a child under 28 days of age.1 The neonatal period is described as the 1st 28 days after birth and may be further subdivided into the very early (birth to <24 hr), early (birth to <7 days), and late neonatal periods (7 days to <28 days).2 The term ‘dermatoses’ is used like the term phylum to cover the full spectrum of cutaneous disorders carrying from inflammatory to neoplastic to congenital.3 The skin of the term new-born is structurally mature and possesses an intact epidermal barrier.4 Many aberrations varying from physiological (like Mongolian spots) and transient (erythema toxicum neonatorum) to grossly pathological (neonatal lupus erythmatosus) are seen in the skin of neonates. It is necessary to differentiate between benign and clinically significant pathological cutaneous lesions in the neonate. Majority of the neonatal cutaneous lesions are physiological and transient and does not require any therapy. The neonatal skin changes show a wide geographic and ethnic variation. Some skin lesions are common in darker skin and some in white skin. It is important to know the pattern of dermatoses prevalent among Indian children during the neonatal period.5, 6
Background
The thickness of the epidermis is 40 microns in term babies whereas its 20 microns in premature babies. The full thickness of the skin is around 1.2 mm in term babies as compared to 0.9 mm in premature babies. The TEWL is approximated 45 g/m2 per hour at 26 weeks, as compared to 5 g/m2 per hour in term neonates. The acid mantle is complete in term babies as compared to premature babies. The percutaneous absorption is much higher in term babies as compared to the premature infants. The pH of the skin surface of term and preterm neonates is more alkaline (6.5–7.5) but declines in the 1st week to values comparable to adult skin (4.0–5.5).7 The skin serves several critical roles including primary barrier against infection, thermoregulation, and electrolyte balance. The transition from intrauterine aqueous, sterile, atmosphere to comparatively dry pathogen rich environment gives a dramatic challenge to the neonatal skin. If there is disruption because of genetic mutation, injury, or prematurity there can be compromise with the normal functioning of the skin. Healthy full-term new-borns’ skin is developed. Premature infants, have an ineffective barrier that increases risk of invasive infection, dehydration, cutaneous injury, and toxic absorption. A normal full‐term infant’s TEWL is somewhat higher in the first few days of life, but this rapidly improves. Toxicity resulting from percutaneous absorption in the full‐term neonate is less dependent on impaired barrier function per se and is more often related to the increased ratio of surface area to volume as compared to an adult. Transepidermal absorption correlates inversely with gestational age, but barrier function appears to improve rapidly after birth in the preterm infant, and will generally be normal by the end of the second or third week after birth. TEWL is greatly increased in preterm compared to full‐term babies. The resulting outward passage of water can lead to high rates of heat loss by evaporation, which may even exceed the baby’s resting rate of heat production. It is possible that immaturity of the skin also predisposes the premature neonate to penetration of the skin by microorganisms, leading to systemic infection.8, 9
Materials and Methods
Patients and methods
Source of data: Neonates brought to Department of Dermatology of SMCH and neonates hospitalised at Department of Paediatrics who developed cutaneous lesions.
Duration of the study: 1 year
Inclusion criteria
Neonates (day 0 up to 28 days of birth) either born in Silchar Medical College or born outside.
Exclusion criteria
Critically sick neonates admitted in Paediatrics Ward, Neonatal ICU.
Neonates whose birth weights and maturity at birth were unknown due to unavailability of birth records.
Neonates receiving phototherapy.
Neonate born to mothers with a history of drug and alcohol abuse and maternal illness.
Still born
Parents or guardians who refused for inclusion in the study.
Statistical methods
Sample size: 150 neonates.
Study design: Cross sectional hospital based study.
Proportion of each dermatoses was calculated using the following formula.
Proportion of each dermatoses was calculated using the following formula
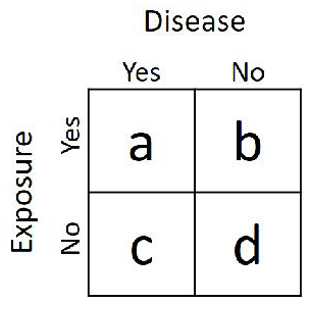
Prevalence Ratio (PR) was calculated using the following formula for calculation of association disease with different variable analysed.
If the prevalence is the same, the ratio will equal 1.0.
If disease prevalence is higher in those with the exposure (placed on top in the ratio), the ratio will be greater than 1.0.
If the prevalence is lower in those with the exposure, the ratio will be less than 1.0.
Prevalence ratio was not calculated for those dermatoses where there was no patient in either group to be compared.
Results
Table 1
Proportion of each group of neonatal dermatoses
Table 2
Neonates with one or multiple dermatoses
Table 2 depicts that 118 (78.67%) neonates had only one dermatoses, 31 (20.67%) neonates had two dermatoses at presentation and only one neonate (0.67%) had three dermatoses on examination.
Table 3
Sex distribution
|
Sex |
Total number of neonates |
Percentage |
|
Male |
81 |
54 % |
|
Female |
69 |
46 % |
|
Total |
150 |
100 % |
Table 4
Distribution of neonatal dermatoses according to gender
Table 5
Distribution of neonates according to birth weight
|
Birth weight |
Total number of neonates |
Percentage |
|
<2.5 kg |
43 |
29 % |
|
≥2.5 kg |
107 |
71 % |
|
Total |
150 |
100 % |
Table 5 depict that in our study of 150 neonates, 43 (29%) neonates had low birth weight i.e. birth weight <2.5kg and rest and 107 (71%) neonate had birth weight ≥2.5 kg.
Table 6
Transient physiological changes according to birth weight andprevalence ratio to calculate its association with birth weight
Table 6 depicts a positive association between low birth weight and vernix caseosa, miliaria, physiological jaundice, sebaceous gland hyperplasia, neonatal acne, sucking blisters, miniature puberty, Epstein pearls/ Bohn's nodules and infantile acropustulosis in our study.
Table 7
Congenital disorders and genodermatoses according to birth weight and prevalence ratio to calculate its association with birth weight
Table 7 depicts a positive association between low birth weight and salmon patch and Mongolian spot in our study
Table 8
Complications of medical procedures on foetus and newborn according to birth weight and prevalence ratio to calculate its association with birth weight
Table 8 depicts a positive association between low birth weight and caput succedaneum and cephalohematoma in our study.
Table 9
Acquired skin diseases according to birth weight and prevalence ratio to calculate its association with birth weight.
Table 9 depicts that no association was found between low birth weight and any acquired skin diseases in our study.
Table 10
Neonatal infections according to birth weight and prevalence ratio to calculate its association with birth weight
Table 10 depicts that a positive association between low birth weight and candidiasis and bullous impetigo in our study.
Table 11
Miscellaneous diseases according to birth weight and prevalence ratio to calculate its association with birth weight
|
S. No. |
Diagnosis |
Number of patients according to birth weight |
Total |
Prevalence ratio |
|||
|
< 2.5 kg |
≥ 2.5 kg |
||||||
|
M |
F |
M |
F |
||||
|
1. |
Erythroderma |
- |
1 |
2 |
- |
3 |
1.24 |
Table 11 depicts a positive association between low birth weight and erythroderma in our study.
Table 12
Distribution of neonates according to maturity
|
Maturity |
Total number of neonates |
Percentage |
|
Pre-term |
33 |
22 |
|
Term |
112 |
74.67 |
|
Post-term |
5 |
3.33 |
|
Total |
150 |
100 % |
Table 12 depict that in our study of 150 neonates, 33 (22%) neonates were born pre-term, 112 (74.67%) neonates were born at term and 5 (3.33%) neonates were born post-term.
Table 13
Transient physiological changes according to maturity andprevalence ratio to calculate its association with maturity
Table 13 depict that in our study a positive association was found between preterm neonates and vernix caseosa, miliaria, physiological jaundice, neonatal acne, sucking blisters, miniature puberty and Epstein pearls/ Bohn's nodules. A positive association was found between post-term neonates and physiological desquamation.
Table 14
Congenital disorders and genodermatoses according to maturity and prevalence ratio to calculate its association with maturity
Table 14 depict that in our study a positive association was found between preterm neonates and Mongolian spots only.
Table 15
Complications of medical procedures on foetus and newborn according to maturity and prevalence ratio to calculate its association with maturity
Table 15 depict that in our study a positive association was found between preterm neonates and caput succedaneum and cephalohematoma.
Table 16
Acquired skin diseases according to maturity and prevalence ratio to calculate its association with maturity
Table 16 depict that in our study we found a positive association between post-term neonates and diaper dermatitis but no such association with pre-term neonate was found.
Table 17
Neonatal infections according to maturity and prevalence ratio to calculate its association with maturity
Table 17 depict that a positive association was found between preterm neonates and candidiasis in neonates.
Table 18
Miscellaneousdiseases according to maturity and prevalence ratio to calculate itsassociation with maturity
|
S. No. |
Diagnosis |
Number of patients according to maturity |
Total |
Prevalence ratio |
||||||
|
Pre term |
Term |
Post-term |
||||||||
|
M |
F |
M |
F |
M |
F |
|
For Pre-term |
For post-term |
||
|
1. |
Erythroderma |
- |
1 |
2 |
- |
- |
- |
3 |
- |
- |
Table 18 depicts that a positive association was found between preterm neonates and erythroderma in neonates.
Table 19
Frequency of neonatal dermatoses in descending order
Results and Discussion
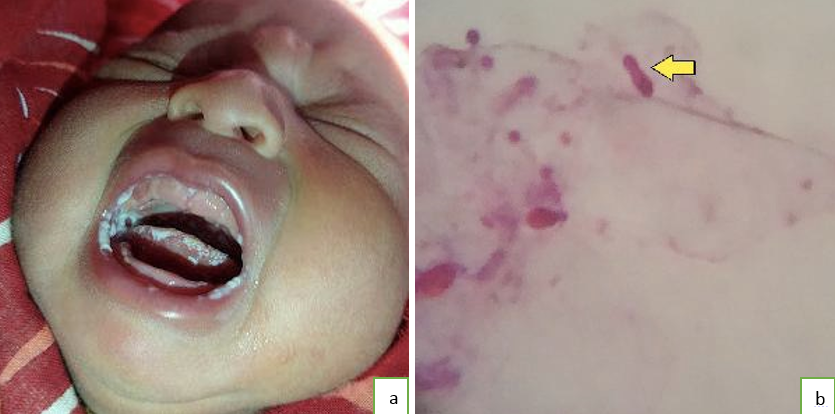
One hundred and fifty new-borns were examined in the study period of one year from. All the babies were examined within 28 days of birth. Out of the 150 neonates 81 (54%) were male and 69 (46%) were female infants. Among 150 neonates, 43 (29%) were low birth weight at birth, i.e. weighing < 2.5 kg at birth. In our study, term neonates were 112 (75%), 33 (22%) were preterm and five (3%) neonates were post term. Vernix Caseosa was seen in eight (5.33%) of neonates. Our findings were almost similar to other Indian studies. 10, 11 Miliaria was found in 21 (14%) neonates and was the second most common dermatoses found in our study. In different Indian studies the frequency varies from 13.2%-24%. 11, 12, 13, 14 There was no seasonal variation. Common sites of involvement were forehead, neck and trunk comparable with other studies. We did not notice any sex predilections or any positive association with low birth weight or prematurity and similar observations were made in other Indian studies. Erythema toxicum neonatorum (ETN) was found in 20 (13.33%) newborns, which was lower than other Indian studies. [Figure 2] In other studies frequency ranged from 21% to 38 %. The lower number of ETN in our study can be attributed to the awareness of the parents regarding the benign nature of ETN. In our study, we observed lesions more commonly on day 2 to day 4. The most common sites of involvement was trunk, extremities and face. We did not notice any relation to lbw or pre maturity. Similar observations were made by other Indian studies.11, 12, 13, 14 Physiological jaundice was noted in 7 (4.67%) neonates which was seen in first 2 days after birth. The frequency as compared to other studies was less. Dash K et al reported physiological jaundice in 20 % neonate whereas Sachdeva M et al reported in 25.6% neonates.13, 14 The underreporting of physiological jaundice in our study can be attributed to the fact that parents and guardians approach Pediatricians for jaundice and yellowish discolouration, rather than Dermatologists. We observed higher incidence of physiological jaundice in lbw neonates and preterm neonates. Sebaceous gland hyperplasia (SGH) was found in nine (6%) neonates. [Figure 3] It was very low as compared to other Indian studies where incidence varies from 21.4% to 62 %. (11)(14) Three out of nine neonates with SGH were low birth weight (lbw) babies indicating a positive association between lbw and presence of SGH but we didn’t find any positive association of SGH with maturity at birth. In a study conducted in 1989 conducted by Nanda A et al higher incidence of SGH was reported in preterm without any comments on the birth weight.15 Nevertheless, it should be kept in mind that prematurity is a cause of lbw. Neonatal Acne was found in three (2%) neonates.[Image 3] Out of the three neonates with acne, two were male and one was female. We did not notice any positive association of neonatal acne with low birth weight but a positive association was found with prematurity. It was comparable to other Indian study by Jain N et al who reported the incidence of neonatal acne as 2.5 %.11 However, in the study by Baruah CM et al the incidence was 0.2%.12 Sucking blisters were found in five (3.33%) neonates. Out of the five neonates, three were male and two were female. Four out of five neonates were lbw and pre-term at birth indicating strong positive association between sucking blisters and lbw and prematurity. Very less reporting has been done regarding sucking blisters in previous studies. Cutis marmorata was seen in 7 (4.67%) neonates. We did not notice any sex predilections or any positive association of cutis marmorata with low birth weight or prematurity. In other Indian studies prevalence of cutis marmorata varies from 1% to 16%.10, 13, 16 Miniature puberty was seen in three (2%) neonates. Out of the three cases, two were female and one was male. Genital hyperpigmentation was the sign of miniature puberty in the single male case. Clitoral hypertrophy was the sign of miniature puberty in both the female with miniature puberty. Out of the three neonates, two were prematurely born with lbw indicating a positive association of miniature puberty with lbw and maturity. In other Indian studies, the incidence of premature puberty varies from 13.3% to 71%.10, 11, 16 Epstein’s pearls (EP) and Bohn’s nodules (BN) were observed in seven (4.67%) neonates. Epstein’s pearls were seen in five neonates and in all the cases, their location was over the hard palate. [Figure 5] Bohn's nodules were seen in 2 cases and in both the cases their location was on the inner maxillary alveolar ridge. We did not notice positive association of EP/BN with low birth weight but a positive association was found with prematurity. In other Indian studies, the incidence of EP was much higher and variable ranging from 17.5% to 88.7%.10, 11, 15 Physiologic desquamation (PD) was noted in four (2.67%) neonates. [Figure 6] The incidence of physiological desquamation is highly variable in different Indian studies. Gudurpenu S et al reported PD in 5.9% neonates whereas Baruah CM et al reported PD in 83% neonates.10, 12 We did not notice any positive association of PD with low birth weight unlike Sachdeva M et al who found PD to be more common in lbw. 14 A strong positive association was observed between PD and neonates who were post term. Such association was not reported in previous studies. This can be attributed to lower amount of vernix caseosa in post-term neonates. The most common sites of PD were palm, soles, wrists, ankles and lower abdomen. Neonatal occipital alopecia (NOA) was observed in three (2%) cases. [Figure 7] We did not notice any sex predilections or any positive association of NOA with lbw or prematurity. Our findings were comparable with study by Jain N et al who reported NOA in 2% cases whereas Gudurpenu S et al reported NOA in 0.5 % of cases. 10, 11 Infantile acropustulosis (IA) was seen in two (1.33%) patients and both the babies were of male gender. There was no association of IA with lbw or prematurity. Our findings were comparable with study by Gudurpenu S et al who reported IA in 0.9 % cases. 10 Milia was observed in four (2.67%) neonates.[Figure 8] In different studies, incidence of milia has been found to vary from 6.8% to 93.1%. 10, 12 In our study out of the four neonates with milia two were male and two were female. Observations made by Gokdemir G et al in Turkish neonates suggests female preponderance. 17 Milia was found in only those mature babies and those weighing ≥2.5kg. In all the four cases, more than two sites were involved. Lanugo was observed in four (2.67%) neonates. [Figure 9] All the four neonates who presented with lanugo were prematurely born with lbw. Incidence of lanugo varies in different Indian studies from 7% to 14.4%.13, 14 Harlequin colour change and natal teeth was found only in one neonate (0.67%) each. Both the neonates were prematurely born male babies and lbw. Harlequin colour change was reported in 0.4%- 1.4% neonates in other Indian studies. 10, 16 Natal teeth was reported in 0.5% neonate by Jain N et al. 11 Vascular birthmarks observed in our study were haemangioma and salmon patch. Haemangioma and Salmon patch was present in two (1.33%) neonates each. Among the two neonates with haemangioma one was male and one was female.[Figure 10] The sites of involvement of haemangioma were face and buttocks. The incidence of haemangioma was slightly higher then other Indian studies. The higher number of haemangioma in our study can be attributed to racial variations. Hemangioma had no association with low birth weight or prematurity. Both the neonate with hemangiomas were screened for multiple haemangioma. Multiple hepatic hemangiomas have been reported in the female neonate. Considering other Indian studies Haveri FT et al reported haemangioma in 0.2 % cases, Baruah CM et al in 0.2 cases and Jain N et al in 0.5% cases.11, 12, 16 Salman patch was seen only in male neonates. They were seen as poorly defined faintly pink macule. Salmon patch was present over neck in all the cases. The incidence of salmon patch in other Indian studies varied from 4.1% to 35%.11, 10 Salmon patch had no association with low birth weight or prematurity like other Indian studies. Mongolian spots (MS) were seen in nine (6%) neonates in our study out of which five were male and four were female. [Figure 11] In other Indian studies the incidence of Mongolian spot is quite high. 10, 11, 12 The variation in the reporting may be due to the racial variations. The most common site of MS in our study was lumbo-sacral area followed by trunk. One or more Mongolian spots at different sites were noticed in the same baby in 4 neonates (three male and one female). We found a positive association of lbw and prematurity with MS. Café-au-lait macule (CALM) was present in single male baby (0.67%) born at term with weight ≥2.5 kg. [Figure 12] In this neonate, solitary CALM was present over face. In a study by Baruah CM et al, CALM was seen in 7.8% of patients.12 Nevus depigmentosus (achromicus) was present in single female baby (0.67%) which was born at term with weight ≥2.5 kg. Nevus depigmentosus was present over chest. [Figure 13] Dash K et found a single case of nevus depigmentosus in a study done on 100 neonates and Baruah CM et al reported one case of nevus depigmentosus in a study on 500 neonates.12, 13 No association was found between lbw and prematurity with presence of CALM or nevus depigmentosus. In our study, we found couple of cases of lamellar ichthyosis who presented as classic collodion baby. [Figure 14] Both of them were male neonates born at term with weight ≥2.5kg. Nanda A et al in a study on 900 neonates found 2 cases of collodion baby due to lamellar ichthyosis.15 Complications of medical procedures on foetus and newborn was present in 4.67 % neonates. Cephalohematoma was present in 3 (2%) neonate (two male and one female), caput succedaneum in 3 (2%) neonate (two male and one female) and subcutaneous necrosis was present in 1 neonate (female). Out of the two male neonate with cephalohematoma one was preterm with lbw and one was born at term with lbw. The female neonate with cephalohematoma was born at term with birth weight ≥2.5kg. In all cases cephalohematoma occurred following use of forceps as a birth-assisting tools. All three caput succedaneum cases had history of prolonged second stage of labour. Subcutaneous necrosis, which we found in a single case, was due to application of alcohol-based cleanser in a preterm female neonate. Almost no reporting has been done in previous studies done regarding the iatrogenic dermatologic complications. Jain N et al reported bruise in 17.5% cases, erosion in 1% case, and irritant contact dermatitis in 0.5 % cases. 11 Infantile seborrheic dermatitis (SD) was the fourth most common dermatoses in our study constituting 19 (12.67%) of neonates. There is a variation in incidence of infantile SD in different Indian studies from 4% to 15%. 11, 13 Infantile SD was in the form of cradle cap. [Figure 15] There was no sex predilection in our study. There was no association of infantile SD with either lbw or prematurity of the neonates. Sachdeva M et al reported higher incidence of infantile SD in term babies and in high weight babies. 14 Diaper dermatitis was the most common dermatoses in our study.[Figure 16] It was present in 26 (17.33%) neonates, much higher than other Indian studies (0.1% to 5%).10, 11, 15, 16 It shows that diaper dermatitis is a new phenomenon, which is in rise due to faulty infant rearing practices. There was no association of lbw babies with diaper dermatitis but a positive association was found between post term neonates and occurrence of diaper dermatitis, a finding not shown in previous studies. In our study we found one case of neonatal psoriasis and sclerema neonatorum, which were not reported in previous Indian studies reviewed. Grattage test was done in case of neonatal psoriasis. [Figure 17] Histopathological findings confirmed our diagnosis. Cutaneous Infections were seen in 12 (8%) neonates. The most common infection was candidiasis, seen in four (2.67%) neonates. [Figure 18a] The diagnosis of candidiasis was confirmed by the presence of pseudohyphae under microscope. [Figure 18b] Two were male and two were female. Out of the four neonates, three were lbw indicating a positive association of lbw and occurrence of cutaneous candidiasis. Similarly, a positive association was found between pre maturely born babies and cutaneous candidiasis. This association might be attributed to the immature immune status of premature and pre-term babies. The incidence of candidiasis in different Indian studies varied from 0.2% to 4.5% neonates.10, 12 The next common neonatal infection was bullous impetigo, which was present in three (2%) neonates, of which one was male and two were female. A positive association was found between lbw and bullous impetigo but no such association was found between non-bullous impetigo and prematurity. We also found one case (0.67%) each of staphylococcal scalded skin syndrome (SSSS), [Figure 19 a] non-bullous impetigo, varicella, dermatophyte infection [Figure 20a] and breast abscess. Due to single case, the strength the prevalence ratio was not calculated. Gram staining along with culture was done for SSSS, impetigo and breast abscess for confirmation. [Figure 19b] KOH test was performed for confirming dermatophyte infection.[Figure 20b] Tzanck test was done for varicella but no Tzanck cells were found. Gudurpenu S et reported 0.5 % neonates with bullous impetigo.10 Jain N et al reported neonatal varicella syndrome in 0.5% cases.11 In our study, we found erythroderma in 3 (2%) cases. Two cases were due to lamellar ichthyosis (also known as non-bullous congenital ichthyosis) and one case of erythroderma was due to staphylococcal scalded skin syndrome (SSSS). The etiological factors of erythroderma and their association have been discussed above.
Summary
The present study was conducted at Silchar Medical College & Hospital, Silchar, for a period of one year. The study was undertaken to study the clinical pattern of various dermatoses in neonatal period and the relationship/ association of neonatal dermatoses with maturity and birth weight of neonates. One hundred fifty neonates were examined in our study at our Hospital. 54.2% neonates were male and 45.8% were female. The diseases were not mutually exclusive in occurrence in neonates as some neonates had more than one type of dermatoses. 78.67% neonates had only one dermatoses, 0.67% neonates had two dermatoses at presentation and only one neonate 0.67% had three dermatoses on examination Out of the 150 neonates, 66 % neonates had transient physiological changes, 11.33% had congenital disorders and genodermatoses, 4.67% had iatrogenic complications, 30% had acquired skin diseases, 8% had neonatal infections and 2% had other miscellaneous diseases. The five most common dermatoses overall were diaper dermatitis (17.33%), miliaria (14%), erythema toxicum neonatorum (13.33%), infantile seborrheic dermatitis (12.67%), sebaceous gland hyperplasia (6%) and Mongolian spot (6%). Slight female preponderance was found in miliaria, erythema toxicum neonatorum, physiological jaundice, miniature puberty, physiological desquamation, milia, lanugo, haemangioma, diaper dermatitis, candidiasis and bullous impetigo. Low birth weight babies had predilection for vernix caseosa, sucking blisters, candidiasis, miniature puberty, caput succedaneum, cephalohematoma, physiological jaundice, infantile acropustulosis, salmon patch, Epstein’s pearls/ Bohn's nodules, miliaria, sebaceous gland hyperplasia, neonatal acne, mongolian spot, bullous impetigo, erythroderma. Preterm neonates had predilection for vernix caseosa, sucking blisters, miniature puberty, candidiasis, Mongolian spot, caput succedaneum, cephalohematoma, erythroderma, miliaria, Epstein’s pearls/ Bohn's nodules and a positive association was seen between post-term neonates and physiological desquamation, diaper dermatitis. Neonatal psoriasis and neonatal dermatophyte infection were the unusual findings which we found in our study.
Conclusion
Neonatal skin differs from normal adult skin in many aspects. Similarly, skin manifestation at birth and neonatal period differs from adult skin. Hence, we should have a clear knowledge while dealing with neonatal skin. In most of the times, in the neonatal period the neonate may have physiological and self-limiting skin manifestations, which do not require any active intervention. Hence, unnecessary exposure to medications or interventions can be avoided. Many cutaneous manifestations in neonatal period may reflect other systemic disease as well.
However, early intervention and follow up of pathological skin disease can prevent further complication.