Introduction
The metabolic syndrome is characterised by multifactorial abnormalities of metabolism including genetic and environmental factors, sedentary and stressful lifestyle and unhealthy dietary habits. It is also termed as Reaven syndrome, syndrome X, dysmetabolic syndrome X (ICD-9 code 277.7), and insulin resistance syndrome. Type 2 diabetes mellitus and multiple atherogenic cardiovascular system damage are two well-known health issues associated with metabolic syndrome (MeTS).1, 2 The criteria for diagnosing Metabolic syndrome were published by the National Cholesterol Education Program Adult Treatment Panel (NCEP-ATP) III. These criteria included an elevated waist circumference (>94 cm for males and >80 cm for females), low high-density lipoprotein (HDL) levels (<40 mg/dl for females and <50 mg/dl for males), high TG levels (TG >150 mg/dl), elevated blood pressure (BP >130/85 mmHg), and elevated fasting glucose (>100 mg). According to NCEP-ATP III.3 A diagnosis of metabolic syndrome is thought to be consistent with the presence of any three of the previously listed criteria. A number of dermatoses, including psoriasis, acne vulgaris, acanthosis nigricans, hidradenitis suppurativa, atopic dermatitis, androgenetic alopecia, lichen planus, Squamous cell carcinoma, Melanoma, Seborrhoeic dermatitis, Rosacea and Systemic lupus erythematosus are correlated with metabolic syndrome.4, 5, 6
Discussion
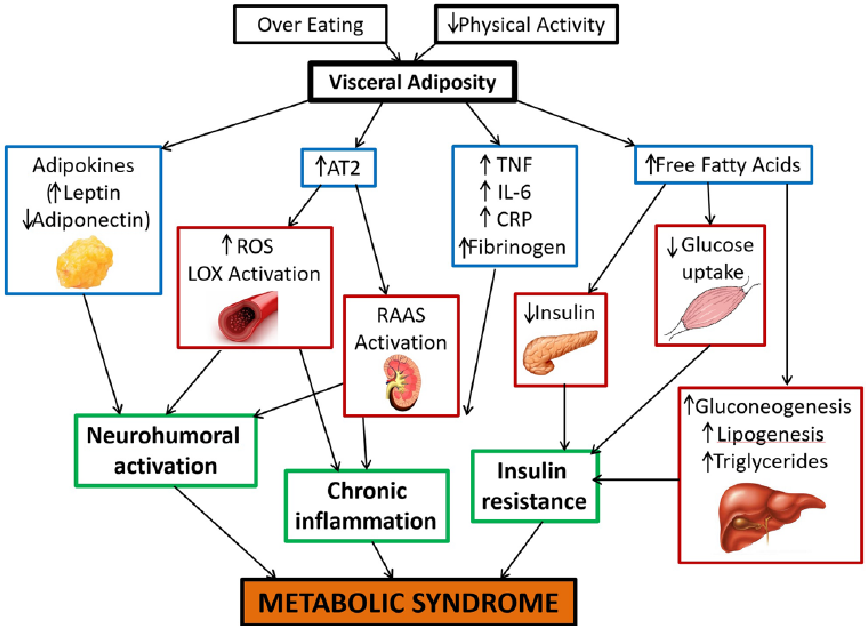
Pathophysiology [Figure 1]
Insulin resistance along with oxidative stress that is brought on by dyslipidaemia and low-grade chronic inflammation is the primary pathophysiological mechanism of the disease. This is attributed to unhealthy eating habits and a sedentary lifestyle. 1
Insulin resistance
Insulin is an anabolic hormone, which increases glucose uptake in liver, muscles, and adipose tissue while suppressing lipolysis and hepatic gluconeogenesis. Insulin resistance lowers the absorption of glucose and raises the amount of free fatty acids (FFAs). FFAs have an impact on PI3K activity linked with the insulin receptor substrate (IRS-1), which lowers glucose transporter type 4 (GLUT-4) translocation to the surface in muscles. Insulin's ability to absorb glucose from the blood is therefore compromised.7 FFAs that act simultaneously in the liver stimulate both lipogenesis and gluconeogenesis. Therefore, hyper-insulinemic state ensues to maintain glucose levels within normal ranges. But eventually, the adjustment fails, resulting in a drop in insulin levels, which worsens by the lipotoxic action of FFAs' on the pancreatic beta cells. 8, 9 Insulin resistance causes more fat deposition in the viscera compared to subcutaneous fat. 10 High levels of FFAs raise cholesterol esters, which causes the synthesis of triglycerides (TGs) and the creation of very low-density lipoproteins, (VLDLs), which are high in TGs. Activating cholesterol ester transfer protein (CETP) subsequently facilitates the transfer of TGs from VLDL to HDL, hence elevating HDL clearance and lowering its level. 8 After being exchanged for low density lipoprotein (LDL) cholesterol ester, triglyceride-rich LDL is produced. Lipoprotein lipase or hepatic lipase then hydrolyses this LDL to produce cholesterol-depleted small dense LDL particles (Sd-LDL). 10, 11 The hallmark of atherogenic dyslipidaemia brought on by insulin resistance in metabolic syndrome is all of these changes in lipoproteins. An imbalance in the levels of circulating androgens is also brought on by insulin resistance. Thus, skin conditions including hirsutism, alopecia, and acne vulgaris that are androgen-dependent are associated with MeTS.
Chronic inflammation
It is evident that Metabolic syndrome is a chronic inflammatory condition with increased levels of proinflammatory cytokines, inflammatory biomarkers, and altered adipokines. Due to insulin resistance there is hypoxia and apoptosis of adipocytes associated with monocyte infiltration. 12 There is increase expression of Leptin, plasminogen activator inhibitor-1, chemerin, IL-1, IL-6, IL-8, monocyte chemoattractant protein-1, tumor necrosis factor-a, C-reactive protein, fibrinogen, C-X-C motif chemokine ligand -1, C-X-C motif chemokine ligand -8 which are proinflammatory biomarkers, whereas anti-inflammatory adipokine like IL-10 and Adiponectin are decreased. 13, 14 IL-6 increases the production of CRP and fibrinogens with another acute phase reactant. 15 IL-6 promote the expression of vascular cell adhesion molecules (VCAMs) and local RAS pathway activation, leading to vascular wall atherosclerosis, inflammation, and dysfunction. 16 TNFα has major role in hampering insulin signalling pathway. 17, 18 There is also increase expression of TL2, TL4 expression on monocytes which leads to inflammatory cascade.19, 20 Other etiopathogenesis of metabolic syndrome includes neurohumoral activation, G- protein coupled receptors Gene Expression, underlying Genetic Predisposition for Metabolic syndrome and oxidative stress due to mitochondrial dysfunction are also explained.
Dermatoses Associated with Metabolic Syndrome
Psoriasis
About 125 million individuals worldwide suffer with psoriasis, a multisystemic chronic inflammatory disease with a frequency of 0.63–0.6% in various racial groups. Studies have linked psoriasis to a higher risk of cardiovascular disease and type 2 diabetes because of the same genetic background, several metabolic risk factors, and similar pathogenic pathways. Moreover, those patients with metabolic syndrome had higher PASI scores. 20, 21, 22 Previous research indicates that, when compared to age and gender-matched controls, children with psoriasis had a statistically significant higher risk of Metabolic Syndrome inclusive of mainly obesity, hyperlipidaemia, and diabetes. 23 Other risk factors include unhealthy lifestyle choices like alcoholism, smoking, and reduced physical exercise. This explains how the pathophysiology of both illnesses involves comparable inflammatory cytokines. In psoriatic conditions, cytokines of the Th1 pathway—TNF-α, IL-2, IL-12, and interferon-γ—dominate. In psoriasis, adhesion molecules such as vascular cell adhesion molecule VCAM-1 and intercellular adhesion molecule-1 (ICAM-1) are increased. This promotes the adherence of inflammatory cells to the vascular endothelium, which in turn induces insulin resistance. 24 Patients with coronary artery disease also had higher levels of IL-17 in their sera. 25 Dysregulation of T-cell interactions is caused by proinflammatory glycoproteins such as osteopontine, peptide hormones such as leptin and adiponectin, and other markers such as homocysteine and CRP. Overexpression of proinflammatory cytokines also causes hyperproliferation of keratinocytes and activation of neutrophils in the epidermis. T-cell activation, a protracted cycle of inflammation, and the development of psoriatic plaques are the outcomes of this.
MetS is more common in psoriatic patients with higher Psoriasis Area Severity Index scores, and it has also been shown that individuals with MetS had longer disease durations than those without Met S. After the age of 40, patients of psoriasis have a much-increased incidence of Met S. 24, 26 When compared to untreated controls, methotrexate lowers the incidence of cardiovascular events in people with rheumatoid arthritis, psoriasis, and psoriatic arthritis. TNF-α antagonists increase insulin sensitivity in individuals with co-existing diabetes and lowers CRP levels in obese people. 27, 28, 29
Acne vulgaris
The connection between Acne vulgaris and Metabolic Syndrome (MetS) is believed to stem from oxidative stress (OS), which is implicated in the underlying mechanisms of both conditions. In acne, dysfunctional follicular walls may release reactive oxygen species (ROS), escalating the inflammatory reaction. Various medications, such as metronidazole, minocycline, erythromycin, and tetracycline, are commonly used to address acne by diminishing hydrogen peroxide (H2O2) and oxygen (O2) levels.30 There are numerous components to the pathophysiology of metabolic syndrome, and it is currently unclear how these components interact together. The primary pathophysiological basis consists of elements including insulin resistance, hypertension, dyslipidemia and visceral adipose tissue (VAT) and its endocrine mediation. Recently, endothelial dysfunction, chronic oxidative stress, systemic inflammation, and atherothrombotic events have also been added. 31, 32, 33 The prevailing theory regarding the development of Metabolic Syndrome (MetS) suggests that visceral obesity serves as the primary catalyst. This triggers a cascade of events, including insulin resistance and chronic inflammation, which are key factors in both initiating and advancing the disease process. Metformin, an oral antidiabetic drug and an mTORC1 inhibitor caused a reduction of acne in young males who adopted a hypoglycemic diet in conjunction with the drug. 34, 35
Hirsutism
Hirsutism is characterised by excessive growth of terminal hair in a male pattern seen in women. A surplus of androgens resulting from several disorders, including idiopathic, polycystic ovarian syndrome, adrenal or ovarian tumours, or adrenal hyperplasia, is the aetiology of this illness. One of the most common forms of hirsutism is believed to be idiopathic hirsutism (IH). It has been demonstrated that insulin resistance and hyperinsulinemia occur in women with polycystic ovarian syndrome. Idiopathic hirsutism is also associated with metabolic abnormalities that are consistent with insulin resistance. 36 Sixty hirsute women were involved in a previous study; thirty of these patients were diagnosed with IH, which designated group 1, and thirty of these patients were diagnosed with PCOS, which designated group 2. The experiment included thirty more healthy, age-matched women in a control group. Following participant examination, the results revealed that the PCOS group had significantly higher WC and diastolic blood pressure (P = 0.028 and 0.005, respectively) than the control group, while the PCOS group had significantly higher systolic blood pressure (P = 0.015 and 0.002, respectively) than the IH group and the control group. Additionally, there was a significant difference in BMI and mFG score between the PCOS group and the control group (P = 0.002 and P < 0.001, respectively), as well as between the PCOS group and itself (P < 0.001, and < 0.001, respectively). 37
Acanthosis nigricans
Acanthosis nigricans is a tell-tale cutaneous sign of underlying insulin resistance. It presents as velvety, hyperpigmented plaques in skin creases, with mucosa only infrequently affected. Acanthosis nigricans is seldom a symptom of internal cancer, although it is frequently linked to diabetes, insulin resistance, and hormonal issues. It is often concomitantly present with skin tags. An increase in blood insulin levels causes activation of IGF-1 receptors (Insulin-like growth factor 1) which in turn leads to Proliferation of dermal fibroblasts and keratinocyte. Insulin also has the potential to displace IGF-1 from IGF binding protein at high doses.38 One hundred patients of acanthosis nigricans and one hundred controls were included in the case-control research where they assessed the presence of metabolic syndrome using laboratory testing and an examination of the demographic profile. The results indicate a significant link between the severity of AN over the neck and metabolic syndrome, as well as a robust association between an increase in waist circumference and an increase in AN severity (P < 0.0001). 39
Atopic dermatitis
Atopic dermatitis usually manifests in early infancy and has been linked to the development of other atopic disorders such as food allergies, asthma, and allergic rhinitis.40, 41 The pathophysiology of atopic dermatitis is multifaceted and involves immune dysregulation, environmental variables, genetic factors, disruption of skin barrier function, and infectious factor triggers. The pathways for Th1, Th2, Th9, and Th 17 are overexpressed. Thus, IL-4, IL-13, IL-5, and IL-31 are components of the inflammatory cascade. 42 The study included AD patients and a control group in which the prevalence rates of the metabolic syndrome (17.0% vs. 9.4%), its components (15.9% vs. 9.2%; obesity: 22.2% vs. 18.6%; diabetes: 15.9% vs. 9.2%; hypertension: 27.9% vs. 15.3%; dyslipidaemia: 47.1% vs. 28.5%, all P values < 0.001) and cardiovascular morbidity (all P values < 0.001) were higher for patients with moderate and severe AD, respectively. Multivariate analysis showed that individuals with moderate-to-severe AD had a substantial over-representation of the metabolic syndrome (P = 0.04), suggesting that these patients may have undiscovered components of the metabolic syndrome. 43
Lichen planus
lichen planus falls under papulo-squamous group of skin disorders characterised by distinctive clinical and histological features. The form and location of lesions determine the classification of lichen planus. 44 According to a cross-sectional investigation, there was a 29.4% recurrence rate and a 35.7% frequency of metabolic syndrome in LP. There was positive correlation of components of metabolic syndrome and chronicity of lichen planus with increased risk for cardiovascular system. 45, 46 Patients with lichen planus have been demonstrated to have a higher incidence of dyslipidemia, which puts them at risk for cardiovascular disease. Furthermore, compared to controls, patients with lichen planus were shown to have greater indicators of both metabolic and cardiovascular risk factors; this is most likely because the condition is associated with chronic inflammation. 47
Androgenetic alopecia
Androgenetic alopecia (AGA) is type of a patterned hair loss that mostly affects men. It is brought on by a progressive miniaturisation of the hair follicle as a result of changed hair cycle dynamics. Elevated androgen, increased 5 α reductase activity, and excess DHT are all present in the balding scalp. 48 In younger people, alopecia has also been shown to occur early because to inflammation. 49 Furthermore, a statistically significant correlation has been shown between the metabolic syndrome, high blood pressure, low serum HDL levels, waist circumference, and the early onset of AGA in the patients. 50, 51, 52 Matilainen et al. in 2000. found that earlier AGA was linked to higher insulin resistance. 53 Banger et al. conducted a case control study with 100 young male patients, and found a statistically significant difference between the AGA group and the control group with regard to the number of persons in the AGA group meeting the Metabolic syndrome criteria. El Sayed et al.'s investigation of ninety female patients with AGA revealed a statistically significant increase in female pattern hair loss incidence and severity, particularly when compared to obesity and hypertension (as determined by NCEP-ATP III criteria). 54 On the other hand, aside from a variation in systolic pressure between disease-based groups, a different study by Ozbas Gok et al. failed to demonstrate a relationship between AGA and Metabolic syndrome. 55
Hidradenitis suppurativa
Hidradenitis Suppurativa (HS) mainly affects parts of the body rich in apocrine glands and is characterised by painful nodules, abscesses, and sinus tracts. The main reason is a follicular structural defect that dilates and distorts the upper infundibular tract, obstructing the hair follicles and causing inflammation and bacterial infection as a result. 56 There are several causes that might cause an overactive inflammatory response, including genetic, anatomical, immunological, and environmental ones. Through the effects of IL-23 and IL-12 as well as a Th17 immune response, increased activity of dendritic cells and T cells leads to keratinocyte hyperplasia. Interleukin (IL)-1, tumour necrosis factor (TNF), IL-17, caspase-1, S100A8, S100A9, and IL-10 levels rise in the tissue as HS worsens, and neutrophils, mast cells, and monocytes are drawn in. 57 The increased frequency of HS in PCOS patients with metabolic disturbances and endocrine disorders implies that obese persons may have an inflammatory state and a high body mass index.58, 59, 60 Because metabolic syndrome is associated with a high level of inflammation, it has also been linked to autoimmune bullous disorders, vitiligo, lupus erythematosus, and chronic urticarial. 61
Rosacea
Rosacea is a chronic inflammatory skin condition presenting with flushing, erythema and papulo-pustular eruption that has been linked to Metabolic syndrome. Specifically, rosacea and CVD risk variables were linked in the Akin Belli et al. study. 62 Blood hypertension, the testosterone effect, and dysregulation of the sympathetic nervous system are observed in Rosacea and Metabolic syndrome cases. 63
Cutaneous tumours
Nagel et al. looked at the connection between skin cancer and Metabolic syndrome characteristics in 2012. Women with elevated blood pressure and malignant melanoma (MM) were found to be positively correlated. Additionally, the body mass index (BMI) of men with MM is typically greater. Women with non-melanoma squamous cell carcinoma skin cancer tended to have higher TG and glucose levels. Furthermore, the development of tendon xanthomas and xanthelasmatas—disorders that resemble tumors but are clearly not proliferative—is a common feature of congenital hyperlipoproteinemias.
Skin ageing
Nagase et al. investigated the skin aging process in animal models with Metabolic syndrome. They found evidence of both oxidative stress and upregulated inflammatory markers as well as increased expression of mineralocorticoid receptors in the skin. They propose a similar mechanism of aging to the one adopted for internal organs in Metabolic syndrome. More specifically, oxidative stress and inflammation are related to Metabolic syndrome, consequently, free oxygen species damaging DNA, mitochondrial function and producing hormonal dysregulation (including insulin resistance) have been associated with the aging process. 64 It appears that skin collagen glycation is related to both Metabolic syndrome parameters and aging. Glycation products cross-link with collagen bundles interfering with its function. This phenomenon becomes more intense in diabetics, accelerating skin aging. Intrinsic factors like the Maillard reaction but also oxidative stress affect fibroblast gene expression reducing levels of metalloprotease inhibitors and increasing production of metalloproteases that degrade collagen. Moreover, collagen itself becomes stiffer with an altered function. Based on this theory, many studies propose antioxidants and inhibitors of collagen glycation as preventive treatments. This condition, along with oxidative stress, inflammation and endothelial dysfunction, has been studied in relation to diabetes. Antidiabetic medication for patients with T2DM would theoretically reduce the reactions extend by controlling blood glucose levels. 65 In general, collagen glycation is considered a platform for research on the pathogenesis of skin aging. 66 Skin autofluorescence showed to be effective on detection of individuals with advanced glycation end products and predisposition to Metabolic syndrome. This could be a promising method for research and future population studies.
Conclusion
Skin serves as a mirror of underlying metabolic menace. Many epidemiological studies show direct co-relation of metabolic syndrome and dermatoses like psoriasis, acne vulgaris, acanthosis nigricans, atopic dermatitis, androgenetic alopecia, lichen planus. Early diagnosis and treatment of Metabolic syndrome prevents long term complications and the dermatoses also respond better to treatment if underlying metabolic problems are corrected. Thus, every patient of these dermatoses should be screened for metabolic syndrome if one or more component of MeTS is present.