Introduction
Diabetes mellitus (DM) is a common endocrine disorder, which affects all ages and socioeconomic groups.1 DM is known to be a chronic multisystem disorder. As the World Health Organisation (WHO) describes it, DM is a metabolic disorder of various aetiologies characterized by chronic hyperglycaemia with disturbances of fat, protein, carbohydrate metabolism which occur as a result of disturbance in insulin action, insulin secretion or both.2 The incidence and prevalence of DM is rapidly increasing, especially so in recently urbanized and developing countries, including India. 1 Diabetes was initially classified into two types: juvenile-onset diabetes mellitus (now known as type 1) and adult-onset diabetes mellitus (now known as type 2). This has expanded to include more than 50 subcategories caused by various pathogenic mechanisms or accompanying other diseases and syndromes. 3 DM includes a wide range of symptoms, with cutaneous manifestations being the most common. A cutaneous problem will arise in 30 to 70% of patients with DM at some time throughout the illness ranging from cosmetic changes to potentially fatal ones, depending on the severity of the condition. 4 While the pathogenesis of the majority of diabetes-related skin disorders is still unknown, aberrant glucose metabolism, changed metabolic pathways, atherosclerosis, microangiopathy, neuron degeneration, and compromised host mechanism are all implicated. Skin abnormalities could indicate prediabetes, poorly managed DM, or even undiagnosed diabetes. Diabetes-related skin problems can reveal information about past and present metabolic status aiding in prompt diagnosis and therapy, ultimately enhancing the overall prognosis.5 Cutaneous manifestations in DM are classified according to the following: vascular damage, neurological damage, infections, obesity and hyperlipidemia related, treatment related skin manifestations, disease associations and miscellaneous conditions. 6
Aim of the Study
To identify the pattern of various skin manifestations in patients with diabetes mellitus and to know their relation with HbA1c levels.
Materials and Methods
This is a cross-sectional, observational study done in patients attending the outpatient departments of Dermatology, General Medicine and those admitted under these departments from February 2024 - May 2024. Clearance from Institutional Ethics Committee was taken before the initiation of the study. Old and new cases (diagnosed based on ADA criteria) of DM of all age groups were included. Patients with HIV, any known malignancies and those not consenting to participate in the study were excluded in the study. A sample size of 100 was selected randomly based on inclusion and exclusion criteria. Written informed consent was taken from each study participant. A detailed history regarding duration of DM, type of diabetes, and treatment taken for DM, comorbidities and complications were taken followed by clinical examination. Investigations like RBS and HbA1c were done. The dermatological manifestations were divided into the above mentioned categories.
Results
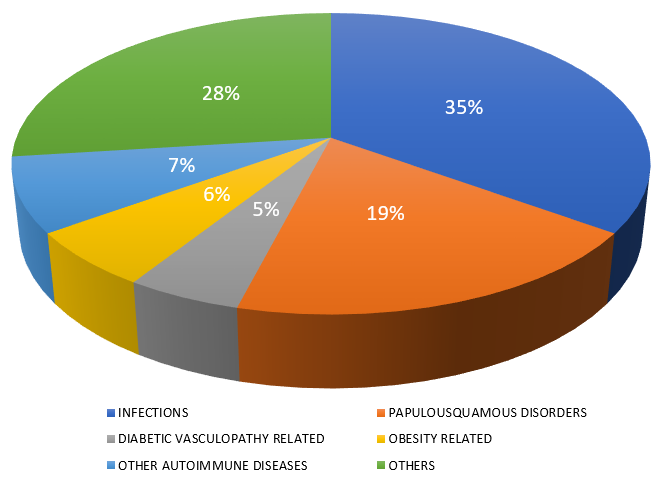
Of the total 100 study population, 96 patients were of non-insulin dependent DM and 4 patients were of insulin dependent DM. Among them, 60 were males and 40 were females. The commonest cutaneous manifestations were infections, seen in 35 patients. The next common cutaneous manifestations were papulo-squamous diseases (19) followed by autoimmune diseases (7), obesity related (6), diabetic vasculopathy related (5) and miscellaneous conditions (28) which include generalised pruritus, xerosis etc.(Figure 1)
Among infections, superficial fungal infections were seen in majority followed by bacterial infections and viral infections. Mean HbA1c of infections was 8.32 (Table-1). Dermatophytosis constituted majority of fungal infections. Among dermatophyte infections, tinea corporis (10) was the most common type followed by tinea cruris (2) and faciei (1). Candidal infections were the next common fungal infections which constituted intertrigo, balanitis, vulvovaginitis and non-dermatophyte onychomycosis.
Table 1
Types of skin infections and mean HbA1c
Papulosquamous diseases
Psoriasis was seen in 9% with mean HbA1c 8.97. The types of psoriasis and their mean HbA1c levels are tabulated in Table 2.
Table 2
Different patterns of psoriasis and mean HbA1c
|
Type of psoriasis |
Percentage |
Mean HBA1C |
|
Psoriasis vulgaris |
5 |
9.72 |
|
Palmoplantar psoriasis |
2 |
8.55 |
|
Scalp psoriasis |
1 |
7.6 |
|
Scalp and palmoplantar psoriasis |
1 |
7.5 |
Lichen planus was seen in 4% with mean HbA1c of 8.17.
Eczemas
They were observed in 6% with mean HbA1c of 7.08. Stasis eczema was seen in 2% (mean HbA1c 6.6), asteatotic eczema in 2% (mean HbA1c 7.05), and nummular eczema in 1% (mean HbA1c 8.3) and seborrheic dermatitis in 1% (mean HbA1c 6.9).
Obesity related manifestations
These accounted for around 6% with mean HbA1c 7.66. Acanthosis nigricans was seen in 3% with mean HbA1c of 7. Acrochordons were seen in 2% with mean HbA1c of 8.2. Xanthelasma palpebrum was seen1% with mean HbA1c of 8.6.
Autoimmune diseases
Seen in 7% of patients with mean HbA1c of 8.42. These constitute vitiligo, alopecia areata, granuloma annulare, morphoea. Their mean HbA1c levels are tabulated in Table 3.
Diabetic vasculopathy related manifestations
These were seen in 5%. Diabetic ulcers were seen in 3% (mean HbA1c 8.83). Diabetic dermopathy was seen in 2% (mean HbA1c 9.65).
Miscellaneous conditions
These account for 28%. These constitute generalised pruritus, xerosis etc; and their mean HbA1c levels are tabulated in Table 4.
Discussion
Diabetes mellitus (DM) is a group of metabolic diseases characterized by persistently elevated blood sugar levels. Type 1 diabetes stems from the body's inability to create enough insulin. Insulin resistance, a condition in which cells do not effectively respond to insulin, is the starting point for type 2 diabetes. As the condition worsens, insulin deficiency may develop. 7 The patho-mechanisms of various dermatoses in diabetic patients are multifactorial. Skin lesions may be caused by metabolic alterations such as hyperglycaemia and hyperlipidemia, increasing vascular damage, neurological damage, or immunological modification. In diabetics, excess glucose in the extracellular environment binds to intracellular and extracellular structural and regulatory proteins by non-enzymatic glycosylations (NEG). This enhances the production of advanced glycation end products (AGEs) which affect the structure and function of collagen, extracellular matrix, and endothelial cells leading to a variety of dermatological symptoms. Hyperinsulinemia increases proliferation in epidermal keratinocytes and fibroblasts via activating insulin-like growth factors-1 (IGF1) which is responsible for acanthosis nigricans. Type1 DM, or late stage of type 2 DM, has an insulin deficiency. Endothelial cells require insulin for appropriate lipoprotein lipase (LPL) action which is essential for digesting triglyceride-rich chylomicrons. This dyslipidemia eventually causes issues such as eruptive xanthoma.8 Individuals with diabetes are more likely to contract infectious diseases because the hyperglycemic environment increases the virulence of some pathogens, decreases production of interleukins in response to infection, reduces chemotaxis and phagocytic activity and immobility of polymorphonuclear leukocytes.9
Our data showed that 38% of the cases were infections. In a study on the cutaneous symptoms of diabetes mellitus, Furqan S et al.,10 discovered that skin infections were the most common finding, occurring in 29.7% of patients. Chatterjee N et al.,11 in their observational study of cutaneous manifestations in diabetes mellitus in a tertiary care hospital in Eastern India found infections to be the largest group(40.9%).
Fungal infections accounted for 19% of the illnesses that we investigated. Furthermore, the most common cause of 41.73% of cases was fungal infections, as found by Mandal N et al.,12 in their cross-sectional observational study on Cutaneous symptoms of diabetes mellitus and correlation with HbA1c level. In their investigation on the frequency and correlation between HbA1c and cutaneous symptoms of diabetes mellitus, Majeed M et al.,13 found that fungal infections were more common than bacterial infections. Umadevi V et al.,5 in their clinical study of cutaneous manifestations in diabetes mellitus found that majority had fungal infections (38%), followed by bacterial infections (11%). Gupta PL et al.,14 in their tertiary care hospital-based study of various skin manifestations in diabetes mellitus, skin infections were observed to be the most common consequences (46%) in cases of uncontrolled diabetes (HbA1c ≥ 7) with fungal infections(56%) being most prevalent followed by bacterial (19%).
In our study, the mean HbA1c values of 8.02 were found in most patients with fungal infections. The majority of the cases Mandal N et al.,12 examined had mean HbA1c readings in the range of 8 to 9.5. Gupta PL et al.,14 in their study observed skin infections to be the most common consequences (46%) in cases of uncontrolled diabetes (HbA1c ≥ 7).
Additionally, it was found in our study that 9% of all cases were psoriatic patients, and their mean HbA1c was 8.97. In their investigation on the relationship between the severity of psoriasis vulgaris and HbA1c, Adiguna MS et al.,15 discovered that patients with psoriasis vulgaris had higher HbA1c levels than those without the disease. Šipka SU et al.,16 in their study on association between skin manifestations and glycaemic control in patients with type 2 diabetes mellitus found that psoriasis was found in 15% of the study participants, with the mean HbA1c at 7.8 ± 1%. In a study to investigate the relationship between psoriasis and diabetes, Brazzelli V et al. discovered that patients with psoriasis had higher HbA1c values than controls and TNF-α, a pro-inflammatory cytokine increased in psoriasis, reduces insulin receptor tyrosine kinase activity and is thought to represent the pathogenetic link between psoriasis and type 2 diabetes. 17
Autoimmune disorders in our study were found to be 8% including Vitiligo (2%), Alopecia areata (3%), sarcoidosis (1%), Morphoea (1%).
In our study vitiligo patients had mean HbA1c of 10.45. Mandal N et al.12 in their study observed HbA1c values in most of their vitiligo patients to be between 9.5% and 11.0%. Hu S et al. 18 in their randomisation study on diabetes, glycaemic profile and risk of vitiligo discovered no statistically significant evidence to establish a causative relationship between dysglycaemia and vitiligo; nevertheless, their findings indicated a favourable causal relationship between T1 DM and vitiligo in the correlation analysis of those diabetic traits.
Acanthosis nigricans was seen in 3% in our study. Majeed M et al.13 observed lower prevalence of 1.5% of acanthosis nigricans in their study on frequency and association of cutaneous manifestations of diabetes mellitus with HbA1c. Gupta SK et al.19 in their study found that 10.9% had acanthosis nigricans. Bokhari M et al.20 in their study on frequency and association of dermatological manifestations of type 2 diabetes mellitus with body mass index and HbA1c levels; found 27.5% of their cases have acanthosis nigricans.
In our study, mean HbA1c of 7 was observed in patients with acanthosis nigricans. Shah M et al.21 in their study on case control study on association of acanthosis nigricans and type 2 diabetes mellitus reported that the frequency of acanthosis nigricans was higher in diabetic (60%) than non-diabetic controls (40%). Rafalson L et al.22 in their study on association between acanthosis nigricans and dysglycemia in an ethnically diverse group of eighth grade students observed acanthosis nigricans was associated with a 50% increased likelihood of dysglycemic state.
Diabetic dermopathy was seen in 2% of our cases. Niaz F et al.23 in their study on cutaneous manifestations of diabetes mellitus type 2: prevalence and association with glycemic control; had observed diabetic dermopathy at a frequency of 9% in their patients. However, others have reported diabetic dermopathy to be the most common and specific dermatological association of DM. 24, 25
In our study, xanthoma and granuloma annulare accounted for 1% each. Miscellaneous disorders such as pruritis and urticaria were reported in 9% and 5%, respectively. Niaz F et al.23 found that spontaneous blisters, granuloma annulare, lichen planus, and eruptive xanthomas accounted for less than 5%.
Conclusion
Many skin conditions like infections and papulo-squamous disorders like psoriasis are associated with raised HbA1c levels. Certain skin conditions like recurrent dermatophytosis and pyodermas gives a clue regarding diabetic status and also helps us in screening denovo diabetes. Skin involvement in diabetes guides the dermatologist and physician for prompt diabetic status check and prevent further complications.