Introduction
Over the last few decades, skin has been appreciated as a surprisingly complicated organ, where precisely regulated cellular and molecular interactions govern many essential processes.1 Apart from which, it also acts as a specialized immune system where immune reactions are noted at various locations in skin. The field of immunopathology has seen an enormous development in the last decade, where identification of antibodies is of great pathologic significance. 1
The diagnostic accuracy of skin conditions by clinical findings alone varies with significant overlap. Histopathological examination (HPE) is diagnostic in most of these conditions; however, in some cases it could only provide diagnostic clues and narrow down with differentials. Certain conditions are histo-morphologically indistinguishable from each other, where immunofluorescence is crucial for definitive diagnosis. 2
Direct immunofluorescence (DIF) tests for tissue bound auto antibodies, is a useful aid in the diagnosis of autoimmune-bullous disorders. However, in conjunction with histopathology, DIF can be a useful supplement to clinical examination in the diagnosis of a variety of non-bullous dermatological conditions such as vasculitis, lichen planus, connective tissue diseases and psoriasis. DIF is a technique which uses Fluoro-isothiocyanate (FITC) labeled antibodies to detect specific antigens where, the location of immune complexes, pattern of reactivity and the reacting antibody can be identified and quantified.3 DIF is a simple, yet accurate technique in the diagnosis of a variety of skin conditions including bullous and non-bullous lesions. DIF tests can add to the certainty of the diagnosis, sometimes modify it and occasionally point towards a different diagnosis.
This study was undertaken to evaluate the clinical features, histopathological and DIF findings in various non-bullous skin diseases. We also evaluated the role of DIF in confirmation of a variety of non bullous skin disorders.
Materials and Methods
A descriptive, ambispective study conducted over a period of 3 years in the department of pathology, Father Muller Medical College, Mangalore. Skin biopsies of clinically non-bullous lesions received from dermatology were included in this study and evaluated for routine histopathology and DIF. Autoimmune vesiculo-bullous lesions, bullous lichen planus and already diagnosed and treated cases were excluded.
For histopathological analysis, 3-4 micron thick sections from the formalin fixed paraffin embedded sections were stained with hematoxylin and eosin stain and evaluated.
For DIF of non-bullous skin lesions, lesional skin biopsy (according to conditions) was performed and samples were placed in an in house prepared Michel's medium (transport medium) and transported to our laboratory. If the specimen could not be processed immediately, the biopsy sample could be stored in this medium upto 14 days. Before the process, the sample is washed in a phosphate buffer solution three times for ten minutes. Subsequently, the biopsy was snap-frozen using Lecia CM1100 cryostat at -20°C and the tissue was prepared for cryo-sectioning. A minimum of 5 slides of 4-6 μm thick sections were cut for each case for staining with IgG, IgA, IgM, C3 and fibrinogen antibodies. Working mixture was prepared using 1μl of antibody (FITC conjugate, Dako) with 40μl of phosphate buffer, in dilution of 1:40 for IgA, IgM, C3, fibrinogen and 1:60 for IgG. Subsequently, the slides were washed in PBS; air dried and mounted using buffered glycerol. Each of these sections were then examined under Lecia fluorescent microscope at wavelengths of 340-400 nm and type, pattern of immune reactant was noted and interpreted.
The collected data was evaluated and analyzed and the clinical, histopathological and DIF diagnosis were compared across each other.
Results
Our cohort consisted of 61 clinically suspected cases of non-bullous lesions. During the course of this study a total of 141 skin biopsies were received for DIF analysis of which non-bullous lesions constitute for 43.26% of the total cases.
Age of our patients ranged from 4 to 64 years. Youngest patient was a 4 yr old boy diagnosed as HSP, while the oldest patient was 68 years old with lichenoid eruptions. Lichen planus cases were predominantly seen in >50 year age groups, while vasculitis cases were scattered across all age groups with 60 % cases occurring <30 years of age. Majority of patients were above 50 years of age and male to female ratio was 1.1:1.
Pattern of distribution
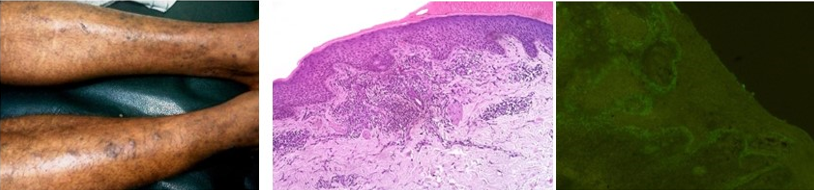
Most cases showed generalized involvement with limbs constituting the major site, lower limb more frequently than the upper limbs. Majority of the vasculitis cases (25 / 27) showed limb involvement, predominantly lower limb. Oral mucosal involvement was noted in 4 cases, all of them were cases of lichen planus. The lesions in vasculitis were generalized pruritic rashes and palpable purpura (55%) followed by erythematous papules (22%) (figure2). Similarly, lichen planus also showed generalized involvement, with lower extremities being frequently involved. The most common pattern of lesions were plaques and papules (13/18 cases), of which 8 were hypertrophic, 5 were regular and 2 violaceous in nature.(Figure 3)
Laboratory investigations showed an elevated ESR in 13 of the 21 cases and Antinuclear antibody (ANA) positivity in all 4 cases of LE and 3 cases of vasculitis. Laboratory investigations were not significant in cases of lichen planus.
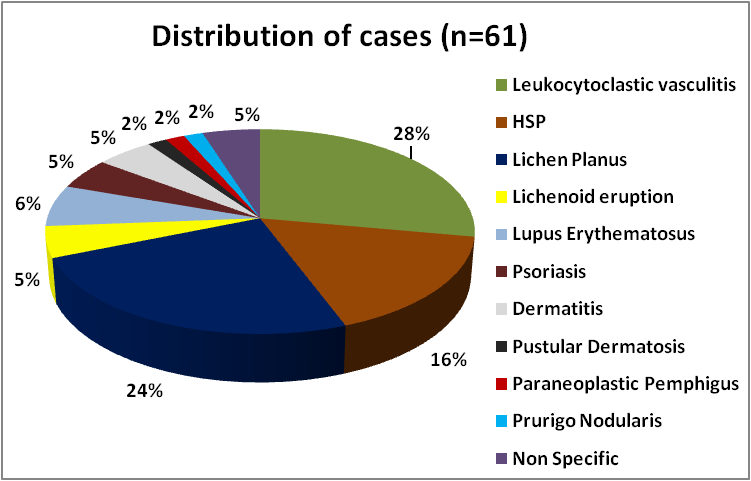
Considering the clinical, histomorphological and DIF findings a final diagnosis was considered in each of these 61 cases. Accordingly, vasculitis constituted the most number of cases, (27, 44.4%) followed closely by Lichen planus. (Figure 1)
Histopathologically, the findings were broadly categorized into epidermal and dermal. The epidermal changes were predominantly seen in cases of lichen planus, LE and psoriasis. The most characteristic epidermal changes in lichen planus was vacuolar degeneration of basal cells (12/15) followed by hyperkeratosis (11/15), acanthosis (9/15) and hypergranulosis (7/15). (Figure 3). These changes were also characteristically seen in cases of lichenoid eruption, LE, and few cases of vasculitis.
The dermal changes include both vessel wall changes and interstitial changes. The vessel wall changes constituted endothelial swelling, fibrinoid necrosis, red cell extravasation and leukocytoclasis, which were all significantly seen in vasculitis and absent in other conditions. (Figure 2). Interstitial mucin was noted in one of the 4 cases of LE and was demonstrated with alcian blue stain. The inflammatory cell component was noted in almost all the cases, at least in mild form. Of the 27 cases of vasculitis majority of them, (85.2%) showed neutrophilic type of inflammatory cells. Whereas, all the cases of lichen planus showed band-like lymphocytic infiltrates.
DIF study was available in all 61 cases, 42 (68.85%) of which showed positive findings. Majority of the cases of vasculitis (92.6%) showed positive DIF findings for at least one antibody. 10 of these cases were diagnosed as HSP with IgA positivity on DIF. (Figure 2). Among the cases of lichen planus, 11 of the 15 (73.3%) cases showed positive findings on DIF, with the majority of them showing fibrinogen positivity along with IgM and C3. (Figure 3). (Table 1)
Table 1
Positive DIF findings in various skin disorders: (n=42)
There was a good overall clinic-histological concordance (87%) with discordance in 8 cases (13%). 3 of these cases reported as lichenoid eruption on histopathology were clinically diagnosed as Dermatitis herpetiformis (DH), polymorphous light eruption (PMLE) and prurigo nodularis. The cases where no specific histopathological findings noted were clinically diagnosed as erythema multiforme, para-psoriasis and prurigo nodularis.
Discordant cases on histopathology and IF
Where DIF was helpful
10 cases of vasculitis were reported as LCV on histopathology; however DIF showed IgA positivity and finally were reclassified as HSP. Another case of lichen planus, histopathologically, showed non-specific findings, but DIF showed shaggy fibrinogen deposits in BMZ. One case which was clinically suspected to be Erythema multiforme, on HPE showed no specific findings. However, the DIF showed IgA, IgM, IgG, C3 and fibrinogen positivity and was reported as SLE. There were 2 clinically suspected cases of prurigo nodularis with a differential of DH, and negative DIF findings ruled out the diagnosis of DH.
Where Histopathology was helpful
Histopathology was diagnostic in the majority of our cases, in appropriate clinical context. Three cases of clinically suspected lichen planus were diagnosed as lichenoid eruptions based on histopathology alone. Among other cases which were negative for DIF, histopathology was helpful to arrive at a final diagnosis with clinical correlation.
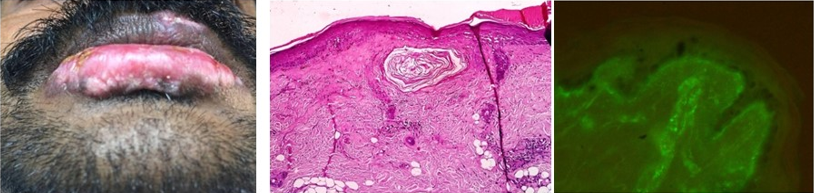
Figure 2
Multiple palpable pruritic rashes over lower extremities. H&E: 10X: Dermal changes in case of vasculitis. DIF: 40X: Case of HSP showing IgA granular vessel wall deposits.
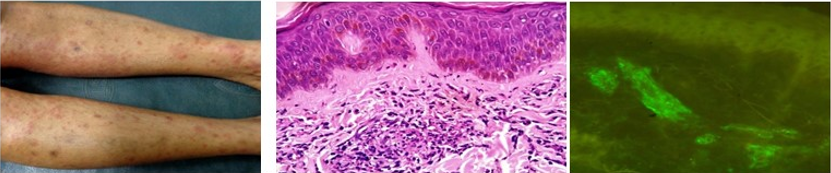
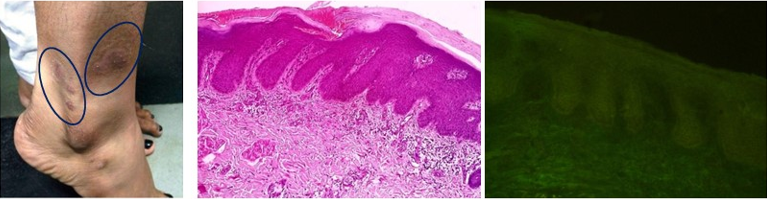
Figure 3
Multiplehyperpigmented plaque like lesions-lower extremities. H&E, 10X: Hypergranulosis, acanthosis and band like lymphocytic infiltrates. DIF: 10X: Shaggy fibrinogen deposits in the upper dermis.
Discussion
Vasculitis
The median age for cases of vasculitis in our study was 34 years and the age of the patients ranged from 4 to 64 years, which was similar to studies by Khetan P et al.4 There was a slight female preponderance for vasculitis, which is similar to studies by Nandeesh B et al and Chintagunta S et al.5, 6
Clinically pruritic rash and palpable purpura were the most common type of lesions (55%) followed by erythematous papules (22%), which was slightly lower as compared to studies by Swamy SM et al and Khetan P et al. 7, 4 Most common site of involvement was lower limb and duration of lesions ranged from one to twenty weeks. Systemic involvement was seen in 38% of cases with arthralgia being the most common systemic manifestation. The results were similar to studies by Chintagunta S et al, Swamy SM et al and Gupta S et al. 7, 6, 8
Among the lab parameters, ESR was elevated in 61.9% of patients of vasculitis and the result was similar to a study by Khetan P et al. 4 ANA profile was positive in 11.1% of our patients which was much higher as compared to the studies by Swamy SM et al and Chintagunta S et al. 7, 6
Histologically, leukocytoclasis is a prominent and characteristic findings in cases of vasculitis, was the most common dermal changes (96.3%), followed by neutrophilic infiltrates, red cell extravasation, fibrinoid necrosis and endothelial swelling of vessel wall. These findings were similar to a study by Khetan P et al. 4 Even though dermal changes were more prominent in cases of vasculitis, epidermal changes in the form of hyperkeratosis were noted in 37% of the cases in our study.
Out of the 27 patients of vasculitis who underwent DIF testing, positive results were noted in 92.6% of cases, for at least for one antibody. This result was superior as compared to studies by Guptha S et al. (Table 2) Of the 27 cases, 10 cases showed positivity for IgA and were diagnosed with HSP, with or without other antibodies staining. The most common antibody positive was C3, which was seen in 88.8% of cases. This result is higher as compared to studies shown in the table. This finding needs to be verified by studies with large sample sizes. In our study none of the cases of vasculitis showed IgG immunoreactivity. This finding is similar to study by Nandeesh B et al, where IgG is the least common immune reactant (10%). The percentage positivity varies according to the time of biopsy taken. Maximum positivity is seen when biopsy is taken within 48 hours after the onset of lesions. 5
Table 2
DIF findings in Vasculitis in comparison with other studies
|
|
Present study |
Swamy SM et al7 |
Khetan P et al4 |
Nandeesh B et al5 |
Gupta S et al8 |
|
DIF Positivity |
92.6% |
76.47% |
83.3% |
39% |
73.9% |
|
IgA |
37.04% |
69.23% |
27.5% |
23% |
43.5% |
|
IgM |
25.92% |
- |
25% |
- |
- |
|
C3 |
88.8% |
61.53% |
47.5% |
26% |
|
|
IgG |
- |
- |
30% |
10% |
27.1% |
|
Fibrinogen |
51.85% |
- |
- |
- |
- |
|
IgM + C3 |
25.9% |
- |
- |
- |
52.2% |
|
C3 + Fib |
51.85% |
- |
- |
- |
- |
According to our study, the sensitivity and specificity of HPE and DIF of vasculitis is 100% and 95.8%, respectively. Studies have shown that DIF is 100% sensitive for diagnosis of HSP, as compared to 90% sensitivity of HPE for the diagnosis of HSP. 9
Lichen planus
Lichen planus cases constituted for 24.6% of the total cases (15 out of 61). The median age of occurrence was 39 years and the age ranged from 10-68 years. These findings were similar in studies by Bhushan R et al and Parihar A et al.10, 11 Most of our patients of Lichen planus were >50 years of age. There was a slight male preponderance among cases of Lichen planus, which was not correlating with other studies which showed almost equal incidence. 10, 11
Clinically plaques and papules were the most common lesions (72%), of which, the majority were hyper-pigmented followed by regular and violaceous in nature. The most common site of involvement was lower extremities (30%). The patients presented with varied duration of lesions ranging from months to years. Oral involvement was seen in 26.6% of the cases, which was much higher as compared to study by Parihar A et al and Arora SK et al. All the other clinical findings were similar to other studies.
The salient histological epidermal changes observed in our study were vacuolar degeneration of basal cells (80%), orthokeratosis 73%), pigment incontinence (73.3%), acanthosis (60%). These results were similar to a study by Arora SK et al, except for pigment incontinence which was seen in 73.3% of our cases as compared to 39% in their study. (Table 3) Also, the percentage of cases showing acanthosis and hypergranulosis were slightly lower as compared to their study. Over all the epidermal changes in our study correlated well with other studies as shown in Table 3. The dermal band-like inflammatory infiltrates were noted in all the cases of lichen planus in our study.
Table 3
Epidermal changes in Lichen planus in comparison with other studies
|
|
Present study |
Bhushan R et al10 |
Parihar A et al11 |
Arora SK et al12 |
Goyal G et al13 |
|
Orthokeratosis |
73% |
- |
100% |
92% |
82.5% |
|
Acanthosis |
60% |
- |
94% |
- |
- |
|
Hypergranulosis |
46% |
- |
96.5% |
82% |
- |
|
Vacuolar degeneration |
80% |
- |
- |
100% |
- |
|
Civette bodies |
26% |
- |
82% |
29% |
87.5% |
|
Pigment incontinence |
73.3% |
- |
99% |
39% |
72.5% |
|
Band like infiltrates |
100% |
- |
94% |
- |
47.5% |
DIF was positive in 11 of the 15 (73.3%) cases of Lichen planus and these cases were positive for at least one antibody. 73.3% of the cases showed staining in the DEJ and these results are similar to those in published literature.(Table 4) 10 However, civatte bodies staining was noted in only 6.6% of our cases as compared to 54.5% by a study by Bhushan et al. Nine cases showed shaggy BMZ deposits while the rest showed granular deposits. Shaggy deposits of fibrinogen at BMZ were noted in 53.3% of cases. Following fibrinogen, IgM (26.6%) and C3 (20%) were also seen staining BMZ and dermal vessel walls in either shaggy and or granular pattern. These findings were noted in a slightly lower number of cases as compared to studies by Kulthanan K et al. (Table 4)
Table 4
DIF findings in Lichen planus in comparison with other studies
|
|
Fibrinogen |
IgM |
IgG |
IgA |
C3 |
|
Present study |
53.3% |
|
- |
6.6% |
20% |
|
Bhushan R et al 10 |
72.7% |
- |
- |
- |
- |
|
Arora SK et al 12 |
91% |
- |
- |
- |
- |
|
Kulthanan K et al 14 |
100% |
29% |
29% |
16% |
47% |
The sensitivity of HPE and DIF for cases of Lichen planus in our study was 93.3% and 73.3% which is similar to a study by Bhushan R et al, which showed 100% and 74.5% for HPE and DIF respectively. 10
Overall our study showed good immune histologic correlation (73.3%) among cases of lichen planus, which was similar to a study by Kulthanan K et al. 14
Lupus erythematosus
The cases of cutaneous forms of lupus erythematosus were commonly seen in the middle age, (range of 21-50 years) with female preponderance, M:Fof 1: 3. These results were similar to study by KP Karumbaiah et al. 15
Histologically, the case of DLE showed basement membrane thickening, basal vacuolar degeneration, interstitial mucin and dermal lymphocytic infiltrates which are all typical features of DLE. Histology was not contributory in cases of cutaneous LE and SLE, which were diagnosed on DIF and ANA profile. Of the two cases of SLE one showed features of scarring alopecia on HPE, however, DIF was negative. Studies have shown that scarring alopecia as a known complication of LE especially SLE. 16 On DIF, one case of SLE and LE each showed characteristic granular BMZ deposits of IgG, IgM, IgA, C3 and Fibrinogen. This case was clinically and histologically negative for any of the specific findings; hence DIF was diagnostic in the case. 17
Approximately, 90-95% of the patients with systemic or discoid lupus erythematosus have positive LBT in involved skin. 18 In a study by Mysorekar VV et al showed 100% sensitivity of DIF for cases of LE. 9 However, in our study the sensitivity was 50%. This finding may not be significant due to limited sample size.
Discordant results analysis - Clinical & histopathological
The clinical diagnosis of skin conditions are usually possible with careful observation, however in some cases it may be just possible to provide differential diagnosis 19 In our study 13.1% of clinical diagnoses were discordant with final diagnosis. This kind of clinic-pathological discordance can be due to non representative sampling, unknown previous therapy or could be due to secondary changes or complications, which alters the morphology of the lesions. Selection of biopsy sites also can be another critical factor for offering an appropriate diagnosis. Three clinically suspected cases of lichen planus turned out to be lichenoid eruptions which were negative for DIF. One of the cases of SLE, histologically showed features of scarring alopecia which is a known complication of LE, especially SLE. 16
Discordant results analysis - Histopathology & DIF
Where DIF was helpful
Of the 27 cases of vasculitis, 10 were diagnosed as HSP on DIF with IgA positivity. Two of the cases lacking any specific histological features were diagnosed as LE and SLE based on DIF positivity. Also a case of lichen planus which was histopathologically non-specific showed shaggy fibrinogen deposits and thus DIF was diagnostic. In two of the cases negative DIF results were helpful in ruling out clinical diagnosis of DH.
Where histopathology was helpful
Histopathology was diagnostic in the majority of the cases of lichen planus even though few of them were negative for DIF. 3 cases were diagnosed as lichenoid eruptions based on histopathology. Of the other cases which were negative for DIF, histopathology was helpful to arrive at a final diagnosis with clinical correlation. Selection of biopsy site, time of biopsy, treatment status and technical errors can lead to false negativity of DIF. In such cases we can arrive at or point towards a diagnosis based on histopathological findings with clinical correlation.
Thus in diagnostic dermatology, clinic pathological correlation is more important than relying on clinical findings alone, for a definitive diagnosis and timely initiation of treatment.
Conclusion
Clinical examination is the initial step in diagnosing non-bullous lesions just like any other skin disorders. However, many of these conditions have overlapping and diverse presentations making clinical diagnosis challenging, where histopathology and DIF are essential in arriving at a definitive diagnosis.
DIF could be crucial in the diagnosis of non-bullous disorders where, clinically, no diagnosis has been made due to the atypical appearance and nonspecific characteristics. In such cases, DIF is a rapid, efficient and convenient method to arrive at a diagnosis. However, DIF requires specialized equipment which requires high capital investment. In developing countries like India, due to financial constraints, affordability could be a problem. Technical and analytical expertise of DIF also plays an important factor. Although, DIF is diagnostic in certain non-bullous skin lesions and it may be non-contributory in few cases; in such cases, histopathology in a proper clinical context remains the cornerstone for diagnosis.
Thus, clinical, histopathological and DIF findings are always to be considered together and correlated to arrive at final diagnosis, as these methods independently may not be diagnostic in all the cases. Even though our study showed positive DIF findings in most cases and highlighted the diagnostic utility in certain cases, ours was a study with heterogeneous cases presenting clinically as non-bullous lesions. A larger, multicentre study could confirm our findings and certainly add to the existing literature.