Introduction
Topical corticosteroids are the commonest agents used in the treatment of dermatological diseases. Numerous steroids of varied strengths are available as over the counter medication at local drugstores. These steroid creams are abused for the treatment of pigmentary problems, acne, fairness etc. These corticosteroids are applied mainly over the face, causing an entity called, ‘topical steroid dependent face’(TSDF).1 Topical steroid dependent face is defined as a long-term damage to the facial skin which is either semi- permanent or permanent due to the unreasonable, uncontrolled, continuous, random application of topical corticosteroids leading to a variety of cutaneous manifestations.2 In this condition, there is appearance of rebound erythema, burning and scaling on the face after stoppage of usage of topical steroids for a long time.3 It also causes psychological addiction to the topical corticosteroids.1
Dermoscopy involves studying the surface and subsurface skin structures through an instrument called as dermoscope.4 It is a diagnostic technique which helps in examining the epidermis, papillary dermis and structures up to reticular dermis.5 The advantage of dermoscopy is that it helps to visualise structures that are not visible to the naked eye or by routine diagnostic methods like magnifying lens examination. Also, dermoscopic features reflect the histopathological changes in the skin. 6 Hence, dermoscopy non-invasively aids in rapid detection of TSDF even before it is clinically evident.
The prevalence of TSDF in India varies from 15% in a study done by Saraswat et al3 to 36.23% in a study done by Pal D et al.7 The topical steroids give rapid relief in most of the inflammatory and infective conditions on using for a short term while prolonged use can cause increased redness, itching, burning, increased hair growth, acne on face which is hard to treat and annoying for the patients.
The abuse of topical corticosteroids is prevalent worldwide.8, 9, 10 The abuse is more common in our society as fair skin is an obsession.11 There are many studies done on topical steroid dependent face in the recent past.12, 13, 14 A lot of such studies are done on the epidemiology of topical steroid dependent face.13, 14 There are only a small number of studies where dermoscopy of these clinical signs are done.15 Hence our study aimed at studying the dermoscopic features of topical steroid dependent face and also comparing the damage to the skin based on the potency of steroid usage.
Materials and Methods
This was a cross- sectional study conducted at the Department of Dermatology of a tertiary care hospital from South India between 1st August 2022 to 31st December 2022. A total of 398 patients aged 18 years and above presenting with facial dermatoses suggestive of topical steroid dependent face like redness, itching, burning, increased hair growth, acne and with a history of topical steroid application over the face for more than one month were enrolled in our study. Prior informed consent was taken and Institutional Ethics committee clearance was also taken before the start of the study. The exclusion criteria included patients with the history of thyroid disorders, pregnancy, polycystic ovarian syndrome, treatment with oral corticosteroids and rosacea. The details on the demographics of the patient like gender, age, education, source of recommendation of topical steroid, cause of application, clinical features, strength and duration of steroid use were recorded using a structured questionnaire. The details of the type of steroid application were recorded. The patients were divided into two groups based on the potency of the topical steroid applied as: one applying class I/II and the other applying class III and above potency topical steroid. The dermoscopy of all cases was performed by two observers independently and blinded for bias. In case of any discrepancy in the findings, a third experienced observer confirmed the diagnosis and final reporting was done. Clinical and dermoscopic images of the patient were taken after obtaining an informed consent. Both polarized and non-polarized modes were used for dermoscopic study. Dermoscopic images were taken from Dermlite DL 3 (3 Gen, Inc., San Juan Capistrano, California).
Statistical analysis was done using Statistical Package for Social Sciences version 20. The dermoscopic features were correlated with the clinical features and potency of application of steroids using Chi- square test. The ‘p’ value less than 0.05 was considered statistically significant. The descriptive data was presented as frequency and percentage.
Results
A total of 398 cases were included in the study. The female to male ratio was 3.06:1, with 300 female patients and 98 male patients. Females formed majority in our study. The larger part of the cases were in the age group of 18-30 years (57.78%). The mean age of the patients was 30.22 ± 5.7 years. Table 1 shows the gender and age distribution in the study.
Three hundred and eighteen patients (79.89%) were literate and eighty (20.10%) of them were illiterate. The source of recommendation for the topical steroid creams was pharmacist in 38.94%, practitioners from alternative system of medicine in 26.63%, friends/ relatives in 19.59%, general physician in 10.80%, social media in 2.01% and dermatologist in 1.75% of the patients (Table 2). The duration of topical corticosteroid application was 1-3 months in 30.15% (120) patients, 4-6 months in 32.66% (130) patients and more than 2 years in 9.04% (36) patients (Table 2). Melasma and other hyperpigmentary causes was the most common cause of steroid usage in 32.16% (128) patients, followed by acne in 30.15% (120) patients (Table 2).
158 patients (39.69%) were applying class I/II steroids and 240 patients (60.30%) were applying class III and above creams. The most prevalent steroid used was 0.1% Betamethasone valerate followed by 0.05% Clobetasol propionate (Table 2). Majority of the patients presented with itching (70.35%) and redness (69.84%); burning sensation (60.30%), pigmentation (55.27%), acne (40.20%) and increased hair growth (24.62%) were the other symptoms as depicted in Table 3. The most common clinical observation was erythema (82.91%) and hyperpigmentation (74.87%) as shown in Table 4.
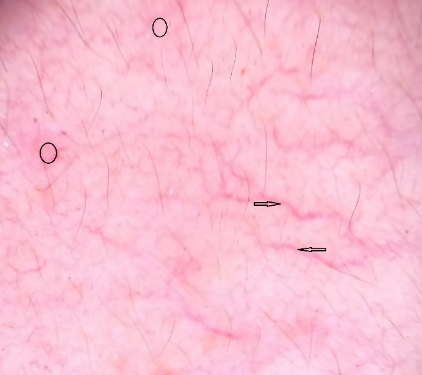
Figure 1
Branched vessels (black arrow), Y shaped vessels (blue arrow), serpentine vessels (green arrow), white structureless areas (black circle) on dermoscopy.
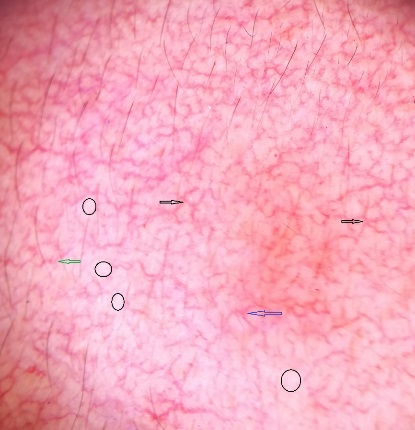
Figure 4
Brown globules (black circles) with an exaggerated pigment network, white hair (black arrow), hypertrichosis (red arrow) on dermoscopy.

Table 1
Gender and Age distribution of TSDF cases
|
|
Number (n= 398) |
Percentage (%) |
|
Gender |
|
|
|
Female |
300 |
75.37% |
|
Male |
98 |
24.62% |
|
Age |
|
|
|
18-30 years |
230 |
57.78% |
|
31- 40 years |
119 |
29.89% |
|
41-50 years |
40 |
10.05% |
|
>50 years |
9 |
2.26% |
Table 2
Other demographic characteristics of the study patients
Table 3
Clinical features of TSDF
|
Symptoms |
Number |
Percentage (%) |
|
Redness |
278 |
69.84% |
|
Acne |
160 |
40.20% |
|
Itching |
280 |
70.35% |
|
Burning sensation |
240 |
60.30% |
|
Increased hair growth |
98 |
24.62% |
|
Pigmentation |
220 |
55.27% |
Table 4
Correlation of clinical and dermoscopic features in topical steroid dependent patients
Table 5
Vascular structures on dermoscopy
|
Vascular structures |
Number (%) |
|
Serpentine |
278 (69.84%) |
|
Branched |
238 (59.79%) |
|
Linear |
178 (44.72%) |
|
Y shaped |
114 (28.64%) |
|
Polygonal |
96 (24.12%) |
|
Fine |
12 (3.01%) |
Table 6
Dermoscopic comparison based on potency of steroid application
The dermoscopic features included mainly diffuse red areas (93.96%), terminal hair (75.87%), telangiectasias (74.87%) and brown globules (73.86%). White hair, focal white areas, exaggerated pigment network, starburst pattern with central plug and pustules, desquamation, pink structureless areas were the other features seen on dermoscopy (Table 4). In this study, the comparison of dermoscopic features like terminal hair (p value 0.03), telangiectasias (p value 0.03), focal white areas (p value 0.02), white hair (p value 0.01) with their concurrent clinical features were statistically significant (p value less than 0.05). These dermoscopic findings on correlation with their concurrent clinical manifestations were seen in statistically higher proportion of the cases dermoscopically. The other dermoscopic features like diffuse red areas, brown globules, desquamation, pink structureless areas on comparison with their concurrent clinical features were not statistically significant (p value more than 0.05) (Table 4).
In this study, the comparison of dermoscopic features like terminal hair, telangiectasias, focal white areas, white hair with their concurrent clinical features were statistically significant (p value less than 0.05). The most common vascular structures under dermoscopy were serpentine (69.84%) followed by branched (59.79%) and linear vessels (44.72%) (Table 5).
Majority of the dermoscopic findings were appreciated more with class III and above steroids but did not show any statistical significance. (Table 6).
Discussion
The misuse of topical corticosteroids by patients is due to widespread availability and fast relief of symptoms.7 The adverse events associated with the abuse or overuse of these creams collectively called as, “topical steroid damaged face”, which was suggested by Lahiri and Condoo. 2
Initially, on application of these topical corticosteroids, due to the anti-inflammatory and vasoconstrictive effects, there is resolution of primary skin condition. But with a continuous use, epidermal atrophy, degeneration of the structures in dermis, and weakening of the collagen occurs.16 This is due to the inhibition of collagen and hyaluronic acid synthesis by topical corticosteroids.17 Also, inhibition of keratinocyte proliferation occurs due to topical corticosteroid usage which leads to skin atrophy and focal white areas on dermoscopy.18 The sudden stoppage of topical corticosteroids gives rise to rebound effect of withdrawal of steroids.2 The withdrawal of topical corticosteroids causes endothelial nitric oxide release which in turn leads to vasodilatation, formation of erythema and telangiectasias.19 There is a chronic immunosuppression caused by topical steroid application which lead to increased growth of micro-organisms, resulting in acneiform eruptions.15 Erythema, burning sensation, itching, dyspigmentation, papulopustular lesions are the various clinical features of TSDF that are described in literature.20
In our study, female preponderance was noted with females 75.37% and males 24.62% in the gender distribution. This finding is similar to the studies done by Chauhan et al.21 in which 68% of 75 patients were females and Skandashree B S et al.22 in which 79.5% of 200 patients were females. This could be because of greater aesthetic interest observed in women than men. In addition to this, skin lightening is one of the main cause for application of these creams. Hence, this may be the reason for application in female population. Many studies across the globe show similar evidence.23, 24
Most of the cases in our study was in the age group 18 to 30 years with 57.78% of patients followed by 31 to 40 years with 29.89% of patients in this age group. These findings were similar to the studies done by Skandashree B S et al.22 where most (56%) of the patients were in the age group of 16 to 30 years, followed by 27.5% of the patients in the age group 31 to 40 years and Nyati et al.25 where 48.20% patients were in the age group 21 to 30, followed by 25.22% of the patients in the age group 31 to 40 years. This is because this age group is more conscious about their looks.
In most of the Indian studies on TSDF, majority of the patients were literate.12, 21 This signifies the ignorance of even the educated patients in the usage of topical steroid creams. In our study, pharmacists (38.94%) were the main source of recommendation for the topical steroid creams. This finding is similar to the study done by Chauhan et al21 in which pharmacists constituted 40% of the source of recommendation. This indicates the widespread over the counter sale of topical corticosteroid creams.
The duration of topical corticosteroid use in our study was up to 6 months in 62.71% patients (1-3 months in 30.15% and 4-6 months in 32.66% of patients). These findings were similar to the study done by Skandashree et al. where 63% of the patients used the steroid for less than six months22 and Ambika et al. where 55% of the patients used topical steroids for less than six months.26 The reason for stoppage of these creams after six months could be the increase in the symptoms of TSDF later on.
Melasma and other hyperpigmentary conditions was the most common indication which accounted for 32.16%, followed by acne in 30.15% and skin brightening creams in 27.13% of patients. These findings were similar to study done by Saraswat et al. where 29% of patients used the topical steroids for fairness, followed by 28.5% for melasma and other hyperpigmentary conditions and 24% for acne.1
The most common topical steroid applied was 0.1% Betamethasone valerate (45.22%), followed by 0.05% Clobetasol propionate (20.10%) and 0.1% Mometasone furoate (15.07%). These findings were similar to a study done by Lahiri and Condoo et al. where Betamethasone valerate was used by 50%, followed by mometasone furoate in 17.8% and clobetasol propionate in 12% of the patients. 2 But in the study by Skandashree et al.,22 Mometasone 0.1% was the commonest topical steroid applied and in the study done by Chauhan et al.,21 0.25% Beclomethasone dipropionate was the commonest topical steroid applied. These differences are due to the variability of the commonly available topical steroid creams in that locality.
The most common symptoms on application of topical corticosteroids were itching (70.35%) and redness (69.84%), followed by burning seen in 60.30% of the patients. Meanwhile, Chauhan et al.21 observed redness (62.66%), followed by burning (52%) and itching (44%).
In our study we found that erythema (82.9%) was the commonest clinical finding in patients with TSDF, followed by hyperpigmentation (74.87%). Similar findings were seen in the study done by Chauhan et al.21 in which erythema in 76% and hyperpigmentation in 74.66% patients was noted.
Dermoscopy is a valuable tool which helps in the diagnosis of TSDF. In our study, the dermoscopic features of TSDF observed were diffuse red areas, brown globules, exaggerated pigment network, terminal hair, telangiectasias, desquamation, focal white area, white hair and pink structureless areas. Dermoscopic study of the clinical features in the present study showed diffuse red areas (93.96%) as the most common finding, followed by hypertrichosis (75.87%), telangiectasias (74.87%) and brown globules (73.86%). These features were comparable to the dermoscopic features of the study by Sethi et al. 12 where 92.4 % showed red diffuse areas, followed by telangiectasias (87.1%) and hypertrichosis (80.3%). In our study, more number of cases showed terminal hair (P= 0.03), telangiectasias (P= 0.03), focal white areas (0.02), white hair (P= 0.01) dermoscopically when correlated with the clinical features. These findings are similar to the study by Sethi et al., 12 where telangiectasias, hypertrichosis, white structureless areas, white hair and desquamation were observed in statistically higher proportion of cases on dermoscopy. The vascular structures that were observed on dermoscopy in our study were serpentine, branched, linear, Y shaped, polygonal and fine vessels. In our study, serpentine vessels were the most common vessels seen (69.84%). This finding is similar to the study by Sethi et al. 12 in which serpentine vessels accounted for 73.5% of the cases.
There was no statistically significant variation of the clinical features with changes in potency of the topical corticosteroids. However, the proportion of the dermoscopic features showed significant increase with higher potency of topical steroid creams. Sethi et al.12 noted similar finding with respect to the alteration of potency and dermoscopic findings.
Dermoscopy also helps us to distinguish TSDF from other causes of facial redness such as tinea faciei, erythemato- telangiectatic rosacea, lupus erythematosus. In superficial dermatophytosis (tinea faciei), there are follicular micropustules, diffuse intense erythema, and brown spots with white- yellowish halo.20 Rosacea presents with polygonal vessels as seen in TSDF, but the presence of focal white area, terminal hairs and white hairs is suggestive of TSDF.4 In lupus erythematosus there is inverse strawberry pattern with salmon-coloured follicular dots surrounded by white halos. 27
The treatment of TSDF focuses on complete stoppage of steroid use, progressively less potent steroids can be used over few weeks. Bland emollients, topical calcineurin inhibitors, non-steroidal anti-inflammatory drugs, antihistamines are the agents used in the management of unpleasant symptoms like burning, itching and stinging sensation. Targeted and suitable treatment can be planned based on the dermoscopic features like erythema and telangiectasias treated by vasoconstrictors like brimonidine, sunscreens; acneiform eruptions treated by anti-inflammatory agents and antibiotics like doxycycline, topical metronidazole, isotretinoin etc.
Hence, dermoscopy can be a valuable tool to identify the early and delayed findings of TSDF. Dermoscopy is non-invasive and can also be used to educate the patients regarding the harmful effects of topical steroids.
Conclusion
Topical steroid induced damage of the face is rampant due to the easy availability of steroid creams. A combination of clinical characteristics and dermoscopy of the topical steroid induced damage aids in the proper and early diagnosis, thus helping to control the further damage. It also helps in predicting the disease severity and enhances adherence to the treatment. Thus, dermoscopy helps in the diagnosis and treatment of TSDF.