- Visibility 57 Views
- Downloads 11 Downloads
- DOI 10.18231/j.ijced.2024.082
-
CrossMark
- Citation
A retrospective clinico epidemiological study of pattern of dermatosis involving trigeminal distribution in a tertiary care center
Introduction
Trigeminal nerve is the principal sensory nerve of face, and it has three distinct branches ocular (V1), maxillary (V2), and mandibular (V3) nerves.[1] Upper division, innervates forehead, upper eyelid, cornea, conjunctiva, and dorsum of the nose. Maxillary branch Supplies upper lip, lateral and posterior portions of nose, upper cheek, anterior temple, mucosa of nose, upper jaw, upper teeth, and roof of mouth Mandibular division Supplies lower lip, chin, posterior cheek, temple, external ear, mucosa of lower part of mouth, anterior two-thirds of the tongue. [2]
Many dermatoses involving the trigeminal nerve have underlying neurological implications. For instance, conditions like herpes zoster affecting the ophthalmic division of the trigeminal nerve may indicate reactivation of the varicella-zoster virus and raise concerns about potential complications such as postherpetic neuralgia and ophthalmic involvement. [3]
Dermatoses involving the trigeminal nerve can significantly impact the quality of life of affected individuals. Pain, disfigurement, and functional impairment associated with these conditions can have profound physical, psychological, and social consequences. Therefore, early recognition, accurate diagnosis, and prompt intervention are essential to alleviate symptoms and improve the overall well-being of patients. [4]
Studies focusing on the pattern of dermatoses involving the trigeminal nerve contribute to the advancement of medical knowledge and facilitate the development of novel diagnostic techniques and therapeutic modalities. By elucidating the underlying pathophysiological mechanisms and identifying potential risk factors, research in this field can lead to the development of more effective treatment strategies tailored to the specific needs of patients. [5]
Materials and Methods
A total of thirty two patients of all age groups and both the sexes, with skin lesions along trigeminal nerve distribution presenting to skin department, at tertiary care centre were included. It is a retrospective observational hospital record based study conducted from January 2023 to January 2024. They were assessed by available detailed demographic history, and clinical examination. The findings are recorded in a pre-designed pro forma. Relevant investigations, wherever required, were done. Ethical clearance is obtained before commencing the study. Microsoft Excel sheets are used to enter data. The study is recorded and its results analyzed. Simple percentages and proportions are used to compare various variables, including age and sex. The final outcome is shown as the percentage of skin diseases along the course of the trigeminal nerve.
Results
Age
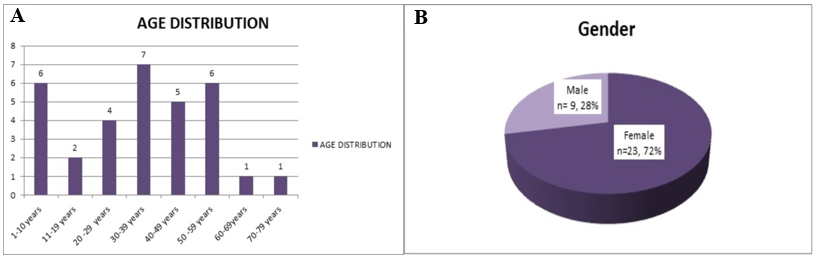
In the current study, it was found that the majority of the patients belonged to the age group of 30–39 years (21.87 %), followed by 1 -10 years (18.75 %) and 50-59 years (18.75 %), 40-49years(15.62 %), Least incidence was in the age group of 11-19 years (6.25%) followed by the age group 60-69 years ( 3.125 %) and 70-79 ( 3.125 %). [[Figure 1]A]
Gender
In the present study, it is found that there is an increased female preponderance (n=23, 71.87%) compared to males (n=9, 28.12%). [[Figure 1]B]
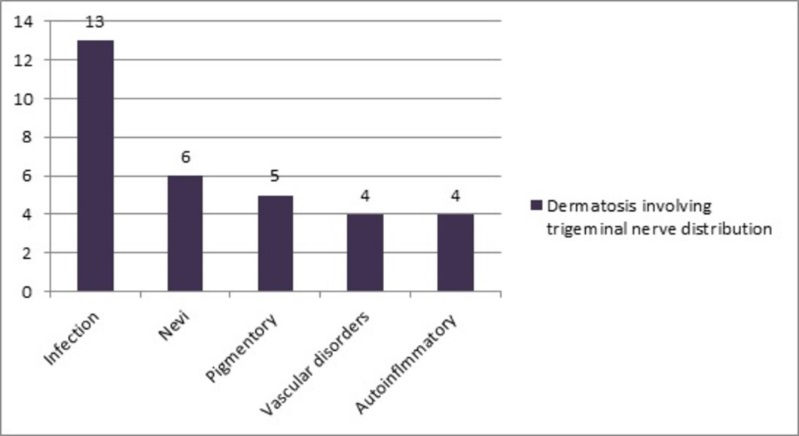
Group of dermatoses involving trigeminal nerve distribution
Of the 32 patients included in this study thirteen (40.62%) patients had infection followed by nevi (n=6, 18.75%), pigmentary disorders (n=5, 15.62%), vascular disorder (n=4, 12.5%) and auto inflammatory disorder (n=4, 12.5%) were seen. [[Figure 2]]
Types of dermatoses involving the trigeminal nerve distribution
Only herpes zoster (n=13, 40.62%) was the cause observed among the infections. Of the nevi, 5 cases (15.62%) had ota nevus, and 1 case (3.125%) was congenital melanocytic nevus. In pigmentary condition, there were five cases (15.62%) of segmental vitiligo. Of the patients with vascular disorders, four (12.5%) patients had port wine stain. Among the inflammatory disorder morphea was seen in 3(9.37%) patients and linear DLE in one patient (3.125%). [[Figure 3] A]
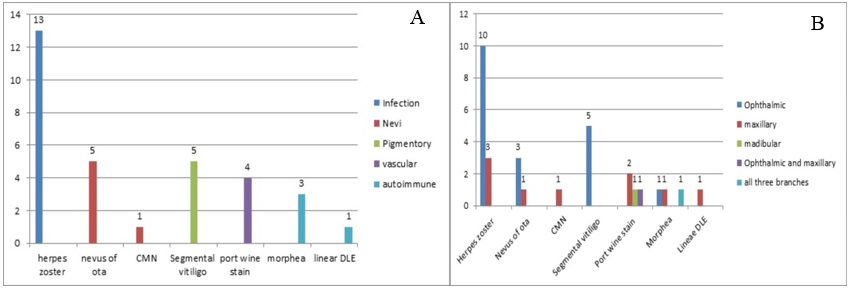



Distribution of dermatoses in relation to trigeminal nerve branches
Only herpes zoster (n=13, 40.62%) was the cause observed among the infections. The most frequent branches of the trigeminal nerve affected were the ophthalmic (n=10, 31.25%) and maxillary (n=3, 9.37%). Of the nevi, 5 cases (15.62%) had ota nevus, of which 3 cases (9.37%) involved the ophthalmic branch, 2 cases (6.25%) involved the maxillary branch, and 1 case (3.125%) was congenital melanocytic nevus which involved the ophthalmic branch of trigeminal nerve. In pigmentary condition, there were five cases (15.62%) of segmental vitiligo, involving the ophthalmic branch of the trigeminal nerve.
Of the patients with vascular disorders, four (12.5%) patients had port wine stain, 2 cases (6.25%) only had maxillary division, and 1 case (3.125%) had both the maxillary and ophthalmic, and in one case, the mandibular division.. Three individuals (9.37%) with morphea, an inflammatory disorder, were identified. Of these, one case covered the entire trigeminal nerve division, one was ophthalmic (9.37%), one involved the maxillary division (9.37%), and one was a linear DLE involving the maxillary division (3.15%). [[Figure 3]B]
Discussion
The trigeminal nerve, with its extensive sensory distribution across the face, plays a pivotal role in mediating various dermatological conditions. Disorders such as trigeminal neuralgia, trigeminal trophic syndrome, segmental neurofibromatosis, herpes zoster and other related ailments manifest distinctively due to trigeminal nerve involvement. Exploring the intricate relationship between the trigeminal nerve and facial dermatoses sheds light on diagnostic challenges, treatment modalities, and patient outcomes. Comprehensive understanding of these conditions is imperative for effective management and improving the quality of life for affected individuals.
In the current study, it was found that the majority of the patients belonged to the age group of 30–39 years (21.87 %) with female preponderance (n=23, 71.87%). Of the 32 patients included in this study thirteen (40.62%) patients had infection followed by nevi (n=6, 18.75%), pigmentary disorders (n=5, 15.62%), vascular disorder (n=4, 12.5%) and auto inflammatory disorder (n=4, 12.5%) were seen.
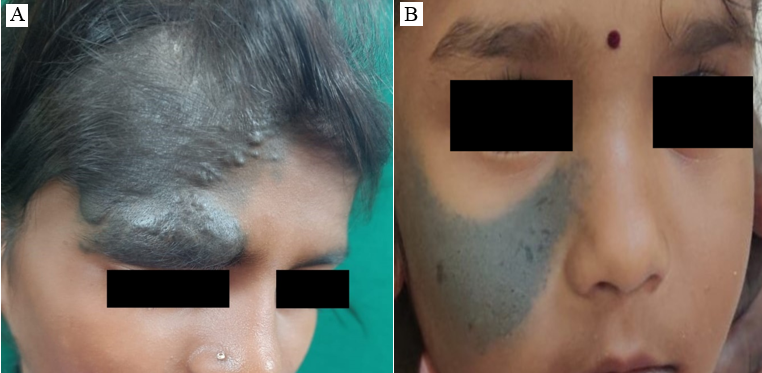
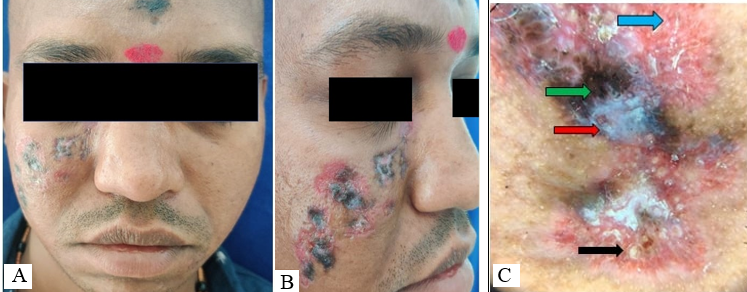
Only herpes zoster ophthalmicus (HZO) (n=13, 40.62%) was observed among the infections. The most frequent branches of the trigeminal nerve affected with HZO are the ophthalmic (n=10, 31.25%) followed by maxillary (n=3, 9.37%) nerve branch. Herpes zoster ophthalmicus (HZO) is described as Varicella Zoster Virus (VZV) involvement of the trigeminal nerve (V) ophthalmic division (V1). [6] It results from the reactivation of a latent VZV infection in the trigeminal ganglion that contains the ophthalmic branch of the trigeminal nerve; thereby causing patients typically have unilateral V1 dermatome prodromal pain, which is followed by an erythematous vesicular or pustular rash in the same region. Patients report the neuropathic pain as "burning," perhaps accompanied by paresthesias. Ocular symptoms such as conjunctivitis, uveitis, episcleritis, keratitis, or retinitis affect between 50 and 85 %of HZO cases. [7] HZO is an emergency ophthalmological condition as there's a chance of losing vision. Age over 50 and immunosuppression are the primary risk factors for HZO. [8] Furthermore, constitutional symptoms including fever, weariness, malaise, and headache may appear before the herpes rash. Acyclovir 800 mg (5 times daily for seven days) is prescribed to control the active viral phase. [9] Even in younger patients, those with HZO have a 1.3- to 4-fold higher risk of cerebrovascular events after the disease. [10]
Of the nevi, five cases (15.62%) had ota nevus, of which 3 cases (9.37%) involved the ophthalmic branch, 2 cases (6.25%) involved the maxillary branch, and 1 case (3.125%) involved congenital melanocytic nevus which involved ophthalmic branch of trigeminal nerve. Nevus of Ota Oculodermal melanocytosis and nevus fuscoceruleus ophthalmomaxillaris are other names for nevus of Ota. The first or second branches of the trigeminal nerve exhibit bluish hyperpigmentation, which is indicative of a dermal melanocytic hamartoma. [11], [12] Nevus of Ota affects Asians at an average rate of 0.014% to 0.034%. [13] The pathophysiology of this condition is unknown, but some theories have been proposed: the epidermal melanocytes may disappear, migrate from hair bulbs, or reactivate previously latent dermal melanocytes due to hormonal changes during pregnancy, dermal inflammation, or UV light exposure. [14]
There have been reports of extracutaneous involvement, with ocular involvement accounting for 60% of cases. The tympanic membrane is the mucosal membrane with the highest incidence of pigmentation in the head and neck. Rarely, the pharynx, tongue, iris, uveal tract, fundus, palate, buccal mucosa, and nasal mucosa are also affected. [15] Nevus of Ota has been associated with to various conditions, including Sturge–Weber syndrome, Klippel–Trenaunay syndrome, neurofibromatosis, multiple haemangiomas, spinocerebellar degeneration, ipsilateral deafness, and cataract. [12]
Congenital melanocytic nevi are uncommon, affecting less than 3% of newborns. [16], [17] They can affect any area of the skin and manifest as a single, large lesion or multiple smaller lesions. Their distribution patterns vary and can be linear, quadrant, multiple, or discrete.[18] They are most common on the head, neck, trunk, and extremities. On the other hand, a dermatomal distribution that nearly mimics the area of nerve supply of ophthalmic branches of the trigeminal nerve is rare. Kopf et al.[19] proposed an arbitrary classification of CMN according to their largest diameter in adulthood, dividing them into: small (<1.5 cm); medium (from 1.5cm to 19.9 cm); and large (or giant: ≥20 cm).The present case measured 7 cm x 8 cm, so classifies as medium congenital melanocytic nevus. When there is a sudden increased growth, pain, bleeding, ulceration, noticeable pigmentary changes, or pruritus, malignancy should be suspected.
Five cases of segmental vitiligo, a pigmentary condition involving the ophthalmic branch of the trigeminal nerve (15.62%), were observed. Segmental vitiligo a widespread idiopathic skin condition, vitiligo affects 1-2% of people across the population. Numerous ideas and hypotheses have been put up in an attempt to explain the precise pathophysiology of vitiligo, including those pertaining to autoimmunity, neuronal, melanocyte self-destruction or faulty adhesion, degenerative, composite, and convergence Not all pathophysiology can be explained by one theory, but in order to completely comprehend the pathogenesis of vitiligo, it is now thought that some of these hypotheses overlap or are related to one another. [20]
Lerner initially presented the neuronal hypothesis in 1959. He proposed the neural idea as a pathophysiological explanation for vitiligo. According to his theory, the skin's nerve endings may emit a cytotoxic chemical that destroys melanocytes. [21] According to Lerner; vitiligo was most likely caused by an increased production of a chemical that lightens melanocytes at the peripheral nerve ends. This is also the theory of Panja, who proposed that malfunction or injury to autonomic nerve components results in melanocytes losing their ability to function. He thought of vitiligo as an adreno-autonomic system-affecting "trophoneurosis." The clinical observation supporting the neuronal theory has gained additional strength and significance due to the correlation between vitiligo and emotional trauma and stress. [22]
Of the patients with vascular disorders, four patients (12.5%) had port wine stain, 2 cases (6.25%) only had maxillary division, and 1 case (3.125%) had both. included the maxillary, ophthalmic, and in one case, the mandibular divisions. Sturge–Weber syndrome (SWS) is a part of phakomatoses which consists of congenital hamartomatous malformations that may affect the eye, skin, and central nervous system (CNS) at different times, characterized by the combination of venous angiomas of leptomeninges, face, jaws and oral soft tissues. The cutaneous angiomas are called port wine stains, which usually occur unilaterally along dermatomes supplied by the ophthalmic and maxillary division of trigeminal nerve. It may be bilateral. It may extend to neck, limbs and other parts of the body, or it could be totally absent. Involvement of the area supplied by ophthalmic division is pathognomonic. [23]
Ocular involvement can result in glaucoma, choroidal hemangioma, buphthalmos or hemianopia. Differential diagnoses include Osler-Weber-Rendu syndrome, angio-osteodystrophy syndrome, Maffuci’s syndrome, Von Hippel Lindau disease, and Klippel Trenaumy-Weber syndrome. Presence of port wine stain can cause deep psychological trauma to patient and development of personality is affected in almost all patients. Treatment and prognosis depend on the nature and severity of clinical features. [24], [25]
Three individuals (9.37%) with morphea, an inflammatory disorder, were identified. Of these, one case covered the entire trigeminal nerve division, one was ophthalmic (9.37%), one involved the maxillary division (9.37%), and one was a linear DLE involving the maxillary division (3.15%). Parry Romberg syndrome also known as progressive hemifacial atrophy is a rare condition that clinically presents with unilateral atrophy of face. Females are more commonly affected. The disease usually begins during first two decades, with a progressive phase lasting 2–20 years, and then a stable phase sets in, usually culminating in resolution. The changes involve the dermatome at one or more branches of the trigeminal nerve. Ocular changes include enophthalmos due to loss of periorbital fat, and rarely uveitis and retinal vasculitis.[26]
The etiopathogenesis of PRS has been explained by various proposed theories involving vascular, genetic, autoimmune, neurogenic, and external factors. Trophoneurosis is the first theory proposed to explain the genesis of PRS. In addition to bone shrinkage on the ipsilateral side, ocular symptoms such as hemifacial atrophy and enophthalmos are caused by malfunction of the trophic fibers of the peripheral and trigeminal neurons. Dysregulation of the migration of neural crest cells is another potential cause. It exhibits hamartomas, ocular neuromas and odontogenic fibromas, in addition to cerebral aneurysms.[27], [28]
Linear discoid lupus erythematosus along maxillary division of trigeminal nerve, the most prevalent type of chronic cutaneous lupus erythematosus is thought to be discoid lupus erythematosus (DLE). The final stage of this inflammatory condition that affects the scalp is called cicatricial alopecia. When DLE of the scalp manifests clinically, the skin usually atrophy and pigmentary alterations are accompanied by erythematous papules or plaques and keratotic follicular clogging. It is dominated by women, particularly in the fourth and fifth generations.[29] In 80% of instances, discoid lupus erythematosus is limited to the head and neck and typically affects sun-exposed regions. Disseminated DLE is the term used when lesions spread beyond of the head and neck region.[30] rarely cases of DLE with dermatomal involvement have been documented in the literature. So far there have been only three cases recorded. Each of these individuals previously had Systemic lupus erythematosus, and they developed DLE lesions within a specific dermatome at the location of healed herpes zoster. We present this distinct DLE condition because it is a de novo dermatomal presentation with no history of pre‑existing dermatoses, described as an isomorphic or isotopic response
Limitations
Small sample size.
Rare cases have included in the study.
Conclusion
Trigeminal nerve-associated dermatoses underscore the intricate interplay between neurology and dermatology. Its recognition and management are crucial for alleviating patient discomfort and preventing potential complications. Understanding the significance of trigeminal nerve involvement in dermatological conditions is vital for tailored treatment strategies and improved patient outcomes. Enhanced interdisciplinary collaboration and on-going research efforts are key to advancing our understanding and therapeutic approaches. By addressing these complexities, healthcare professionals can better serve individuals afflicted with trigeminal nerve-associated dermatoses, ultimately enhancing their quality of life.
Source of Funding
None.
Conflict of Interest
None.
References
- T Huff, LJ Weisbrod, DT Daly. . Neuroanatomy, Cranial Nerve 5 (Trigeminal) 2024. [Google Scholar]
- HK Walker. Cranial Nerve V: The Trigeminal Nerve. Clinical Methods: The History, Physical, and Laboratory Examinations 1990. [Google Scholar]
- A Patil, M Goldust, U Wollina. Herpes zoster: A Review of Clinical Manifestations and Management. Viruses 2022. [Google Scholar] [Crossref]
- Y Ozcan, M A Sungur, B Y Ozcan, Y Eyup, E Ozlu. The Psychosocial Impact of Chronic Facial Dermatoses in Adults. Dermatol Pract Concept 2023. [Google Scholar] [Crossref]
- D Bove, A Lupoli, S Caccavale, V Piccolo, E Ruocco. Dermatological and immunological conditions due to nerve lesions. Funct Neurol 2013. [Google Scholar]
- A Patil, M Goldust, U Wollina. Herpes zoster: A Review of Clinical Manifestations and Management. Viruses 2022. [Google Scholar] [Crossref]
- EJ Cohen, BH Jeng. Herpes Zoster: A Brief Definitive Review. Cornea 2021. [Google Scholar]
- TJ Liesegang. Herpes zoster Ophthalmicus: Natural History, Risk Factors, Clinical Presentation, and Morbidity. Ophthalmology 2008. [Google Scholar]
- H Mappamasing, DM Indramaya, T Setyaningrum, Rahmadewi. Herpes Zoster: a case series with different manifestations. Bali Med J 2023. [Google Scholar]
- JL Bennett. Optic Neuritis. Continuum (Minneap Minn) 2019. [Google Scholar]
- F Murakami, T Baba, M Mizoguchi. Ultraviolet-induced generalized acquired dermal melanocytosis with numerous melanophages. Br J Dermatol 2000. [Google Scholar]
- DG Stanford, KE Georgouras. Dermal melanocytosis: a clinical spectrum. Aust J Dermatol 1996. [Google Scholar]
- A Hidano, H Kajima, S Ikeda. Natural history of nevus of Ota. Arch Dermatol 1967. [Google Scholar]
- Y Hori, O Takayama. Circumscribed dermal malanoses: classification and histologic features. Dermatol Clin 1988. [Google Scholar]
- X Xu, AY Chu, TL Pasha, DE Elder, PJ Zhang. Immunoprofile of MITF, tyrosinase, melan-A, and MAGE-1 in HMB45-negative melanomas. Am J Surg Pathol 2002. [Google Scholar]
- K Osburn, RH Schosser, MA Everett. Congenital pigmented and vascular lesions in newborn infants. J Am Acad 1987. [Google Scholar]
- YT Lin, RJ Teng, HC Chiu, KI Yau, MH Chang, YZ Shan. An unusual presentation of multiple congenitalmelanocytic nevi with a limb distribution. Dermatology 1997. [Google Scholar]
- I Effendy, R Happle. Linear arrangement of multiple congenital melanocytic nevi. J Am Acad Dermatol 1992. [Google Scholar]
- A Kopf, R Bart, P Hennessey. Congenital nevocytic nevi and malignant melanomas. J Am Acad Dermatol 1979. [Google Scholar]
- MS Al'Abadie, HJ Senior, SS Bleehen, DJ Gawkrodger. Neuropeptides and Neuronal Marker Studies in Vitiligo. Br J Dermatol 1994. [Google Scholar]
- A B Lerner. . Vitiligo. Progressin Dermatology 1972. [Google Scholar]
- R K Panja. Etiology of vitiligo-a problem. Ind J Dermatol Vener Lepr 1977. [Google Scholar]
- R Rajendran, R Rajendran, B Sivapathasundharam. Shafer’s Textbook of Oral Pathology. Benign and malignant tumors of oral cavity 2009. [Google Scholar]
- B Suprabha, S Baliga. Total oral rehabilitation in a patient with port wine stains. J Indian Soc Pedod Prev Dent 2005. [Google Scholar]
- S Mukhopadhyay. Sturge -Weber syndrome: A Case report. J Indian Soc Pedod Prev Dent 2008. [Google Scholar]
- J El-Kehdy, O Abbas, N Rubeiz. A review of Parry-Romberg syndrome. J Am Acad Dermatol 2012. [Google Scholar]
- UA Qureshi, NA Wani, U Altaf. Parry-Romberg syndrome associated with unusual intracranial vascular malformations and Phthisis bulbi. J Neurol Sci 2010. [Google Scholar]
- J Miao, R Liu, H Lin, C Su, H Li, G Lei. Severe Bilateral Pyramidal Tract Involvement in a Patient With Parry–Romberg Syndrome. Am J Med Sci 2009. [Google Scholar]
- P Fabbri, C Cardinali, B Giomi, M Caproni. Cutaneous lupus erythematosus: Diagnosis and management. Am J Clin 2003. [Google Scholar]
- M Hassan, KA Watters, E Netchiporouk. Linear discoid lupus erythematosus mimicking en coup de sabre morphea: A case report. SAGE Open Med Case Rep 2019. [Google Scholar] [Crossref]
- Introduction
- Materials and Methods
- Results
- Age
- Gender
- Group of dermatoses involving trigeminal nerve distribution
- Types of dermatoses involving the trigeminal nerve distribution
- Distribution of dermatoses in relation to trigeminal nerve branches
- Discussion
- Limitations
- Conclusion
- Source of Funding
- Conflict of Interest
