Introduction
Granulomatous inflammation defines a pattern of reaction to a wide range of etiologic agents, organic and inorganic with certain morphologic correlates. Granuloma is “a focal chronic inflammatory response to tissue injury evoked by a poorly soluble substance characterized by the accumulation and proliferation of leukocytes, principally of the mononuclear type”.1
Granulomatous reaction is a type IV hypersensitivity reaction evoked by poorly soluble reactive substances. Six types of granulomatous skin lesions are identified according to cellular constituents and associated changes: 1) tuberculoid, 2) sarcoidal, 3) necrobiotic, 4) suppurative 5) foreign body and 6) histoid type granuloma. Incidence and prevalence of different types of granulomatous dermatitis depend on geographic location. Granulomatous skin lesions are common in eastern India. Many granulomatous skin lesions have identical histomorphology and conversely a single pathology can produce varied histological features. 2
Some rare suppurative chronic granulomatous skin diseases include Botryomycosis, Actinomycosis, Rhinosporoidosis, Nocardiosis, Cutaneous Tuberculosis, Actinomycetoma. Cutaneous botryomycosis is a rare and chronic suppurative bacterial infection with commonest causative organism being S. aureus. The diagnosis of botryomycosis is usually confirmed by demonstration of specific bacteria in discharge, tissue culture and characteristic histopathology findings. 3 Cervicofacial actinomycosis, also called lumpy jaw, is a chronic, suppurative and granulomatous bacterial infection caused mostly by Actinomyces species and rarely by Propionicusbacterium species. It classically presents as an indurated and suppurative nodule which subsequently results in draining sinuses and tissue fibrosis. 4 Lupus vulgaris (LV) is the most common form of cutaneous TB, accounting for 75% of the cases. LV is a chronic, progressive, post-primary, paucibacillary form of cutaneous tuberculosis occurring in persons with a moderate or high degree of immunity. It can develop as a result of direct inoculation, extension from an underlying organ, lymphatic spread, or rarely, hematogenous spread from an infective focus. Due to its varied clinical presentation, LV can mimic many dermatological conditions. 5 Madura foot, also known as mycetoma, is a chronic granulomatous infection affecting deep subcutaneous tissue. It is characterized by the formation of granules containing aggregates of the causative organisms, which can fistulate to the skin through multiple draining sinuses. The condition is caused by aerobic bacteria (actinomycetoma) or fungi (eumycetoma). 6 Leprosy and tuberculosis have been prevalent worldwide for over a century. They constitute a global health issue despite advancement of medical research and the success of MDT by the WHO. Coinfection with Mycobacterium leprae and Mycobacterium tuberculosis is rarely reported and varies from 2.5 to 7.7% in India. Coinfection of leprosy and tuberculosis are not uncommon, though infrequently reported. 7
Case Description
Botryomycosis
A 33-year-old male came with a chief complaint of painful red raised mass over left arm since 10 years, which increased in size since 1 year, associated with dragging type of pain and purulent discharge. For which he underwent excision 2 years back and it reappeared again.
On cutaneous examination
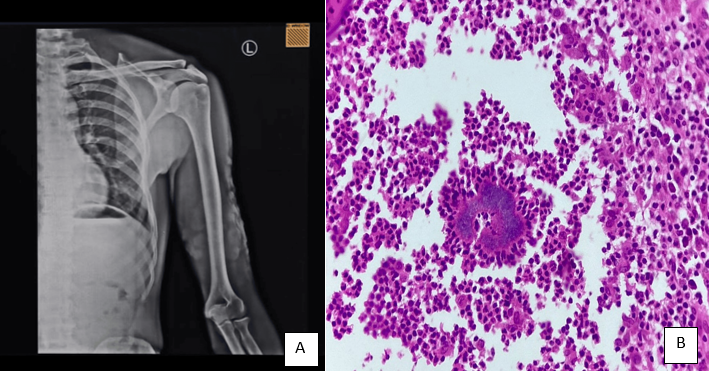
Single, well defined indurated erythematous plaque which is firm in consistency, with pustules, nodules and crusts over the surface measuring 14*17cms over left arm.(Figure 1)
Investigations
Gram stain: Gram positive cocci, non-filamentous bacteria.
Fungal culture in Sabouraud dextrose agar - Negative
Acid fast stain: No acid-fast bacilli was seen
Mycobacterial culture: Negative
Bacterial culture & sensitivity: Staphylococcus aureus isolated.(Figure 2)
Treatment
Treated with Inj.CLINDAMYCIN 600mg twice per day given for 7 days, followed by Capsule Amoxicillin + Clavulanic acid 625 mg thrice daily and Oral Clindamycin 300 mg thrice daily (as per sensitivity).
Ointment Mupirocin L/A over lesion twice daily. Antibiotic therapy is continued till clinical and radiological resolution.(Figure 4)
Actinomycosis
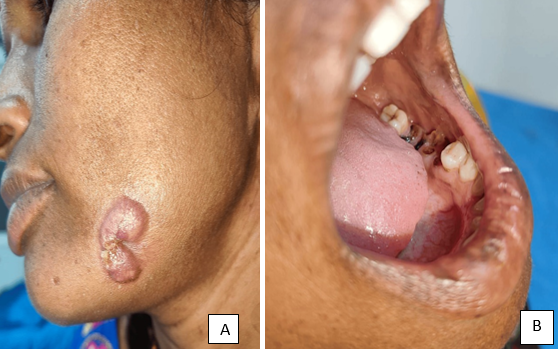
A 35-year-old female came with a chief complaint of itchy painful red raised lesions over left cheek since 5 years aggravated since 1 year. History of dental carries since 6 years.(Figure 5B)
On cutaneous examination
A single well defined indurated, firm, erythematous plaque of size 4*3cms present over the skin overlying left mandible with raised edge at one end and atrophic scarring on other end.(Figure 5A)
Figure 5
A: Erythematous indurated plaque with discharging sinus over skin overlying left mandible and B: showing route of infection with dental caries
Pus culture and sensitivity: Staphylococcus aureus and sensitive for amoxicillin and clavulanic acid
Mantoux test: positive with 20mm induration
On Chocolate agar: it produces molar tooth colonies
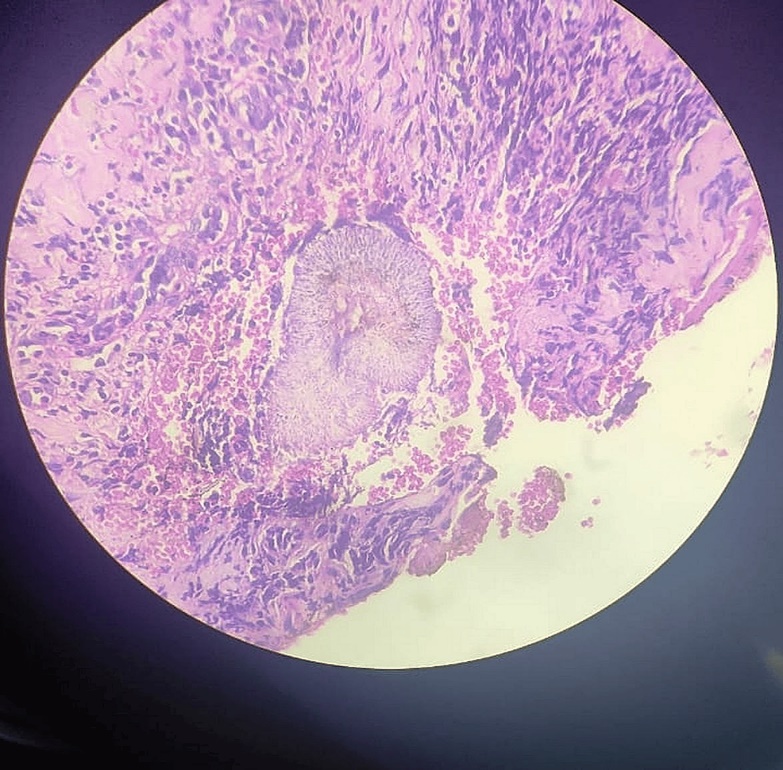
Histopathology - Shows nodular tuberculoid granulomatous infiltrate with areas of suppuration. The granuloma is composed of lymphocytes, plasma cells, histiocytes and epithelial cells with occasional Langhan’s giant cells - suggestive of ACTINOMYCOSIS.
Treatment
Treated with Capsule Amoxicillin and clavulanic acid 625 mg thrice daily given for 60 days.
Ointment Mupirocin L/A over lesion twice daily.(Figure 6)
Lupus vulgaris with scrofuloderma
A 15-year-old male came with a chief complaint of multiple painful raised skin-coloured lesions over neck, trunk, foot since 7 years. History of pulmonary tuberculosis in elder brother.
Examination
On General examination: Bilateral cervical, left axillary and inguinal lymphadenopathy. On Cutaneous examination: multiple ill-defined to well-defined erythematous plaque with crusting with smallest measuring 2*2 cms and largest measuring 8*8cms present over nape of neck, trunk, right axilla, dorsal of right foot, progressing on one end and the other end they are healing with depigmentation and atrophic scarring.(Figure 7A) A single erythematous crusted plaque with draining sinus present over left side of nape of neck.(Figure 7B)
Investigations
Mantoux test: positive with 20mm induration.(Figure 8)
FNAC: from cervical lymph node showed granulomatous lymphadenitis- suggestive of Koch’s etiology.
Histopathology - Shows dense tuberculoid granulomatous infiltrate made up of lymphocytes, plasma cells, neutrophils, histiocytes, epithelioid cells and few Langhans giant cells - suggestive of Lupus vulgaris.
Treatment
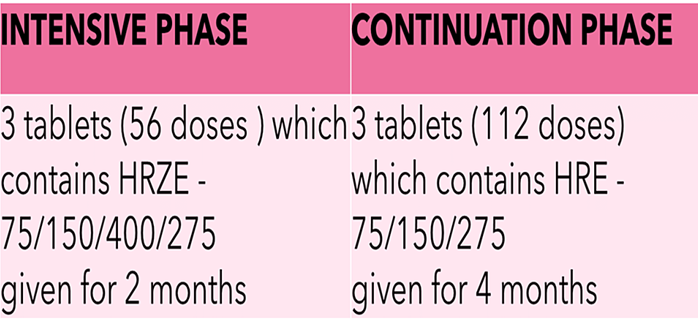
Since the patient weight is 40kgs so according to the revised national tuberculosis control programme, the treatment schedule is (Figure 9)-
H-Isoniazid r-rifampicin z-pyrazinamide e-ethambutol.
Borderline tuberculoid leprosy with type 1 reaction and pulmonary tuberculosis coinfection
A 76-year-old male came with the complaints of patient came with the complaint of multiple red raised lesions over trunk, both upper limbs and lower limbs since 20 days. Also, C/o fever (intermittent) since 30 days.
Patient is a known case of Pulmonary Tuberculosis on Antitubercular therapy since 2 months on irregular medication.
On cutaneous examination
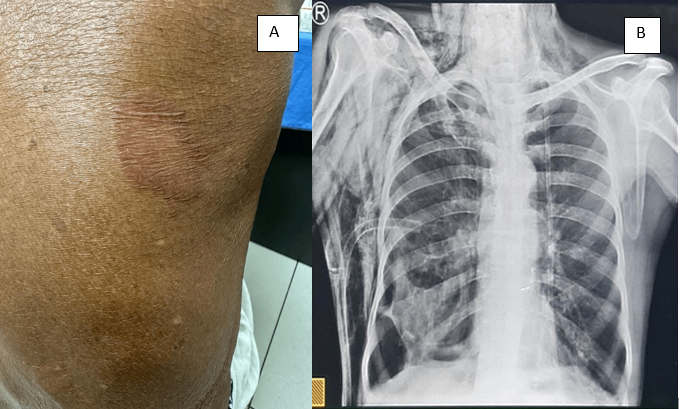
Multiple well defined oedematous and erythematous annular plaques distributed over bilateral flexor aspect of arms, forearms, anterior aspect of abdomen, lateral abdomen, extensor aspect of thigh, knees, lower legs, posterior aspect of trunk.(Figure 11A)
Sensory examination: Cold temperature and fine touch lost over the lesions. Crude touch: intact.
Nerve examination: Bilateral Ulnar nerve thickened, non-tender. Right posterior tibial nerve-thickened, non-tender.
Investigations
Cbnaat - positive, Chest X Ray showing Tuberculosis findings - B/L Hyperinflated lungs with right lower zone emphysematous bullae.(Figure 11B)
Viral markers - Nonreactive
CBC, LFT, RFT, RBS - within normal range
Slit skin smear - Acid fast bacilli+
Bacteriological index 2+, MI-30%
Histopathology
Biopsy shows small nodular tuberculoid granulomatous inflammation situated around neurovascular bundles of appendages and superficial and deep plexuses. Granuloma consists of lymphocytes and epithelioid cells and involves nerve twigs. Additionally, sparse superficial and deep perivascular lymphocytic infiltration is present. The dermo epidermal junction is focally infiltrated by lymphocytes and epidermal rete ridges are flattened.
Multiple furunculosis mimicking sporotrichosis
A 53-year-old female patient came with the complaints of multiple dark coloured raised lesions with diffuse swelling of left lower leg since 5 months. H/O of trauma present.
On cutaneous examination
Multiple well-defined erythematous nodules with surrounding hyperpigmentation in a linear distribution present over left lower leg and dorsum of left foot.(Figure 12) Few lesions became pustular with draining fluid. Mild tenderness+
Investigations
Pus for culture & sensitivity - Staphylococcus aures was isolated.
Fungal culture & sensitivity - no fungal elements noted.
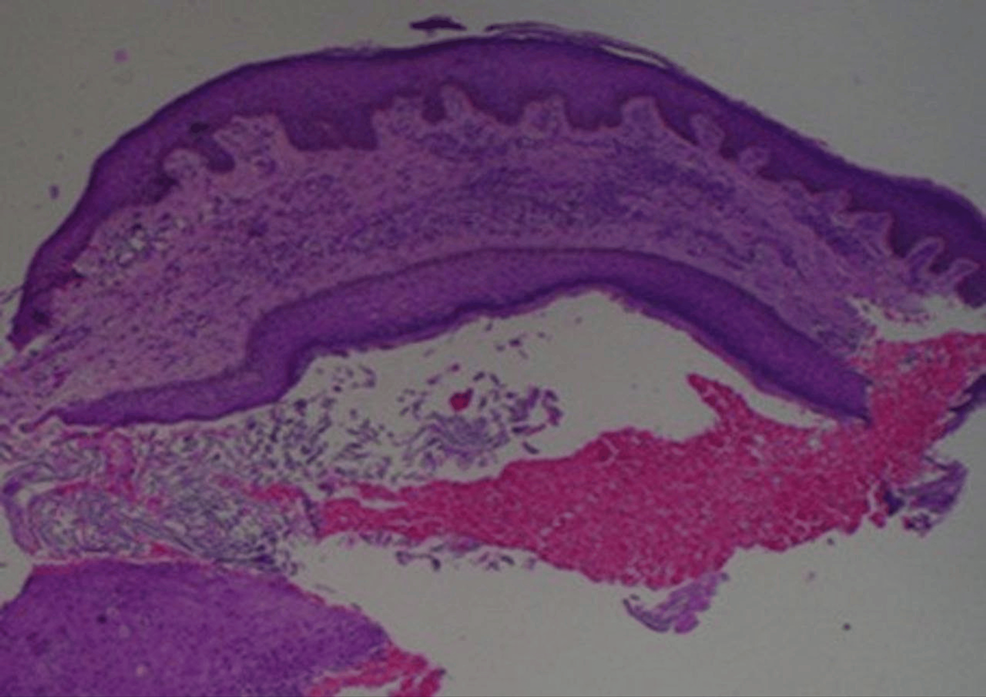
Histopathology: Granulomatous suppurative and fibrosing inflammation. Suggestive of infective granuloma-shows patchy granulomatous inflammation with foci of neutrophilic aggregation. Granuloma consists of lymphocytes, eosinophils, plasma cells, histiocytes and epithelioid cells. Overlying epidermis shows moderate spongiotic psoriasiform changes and at places infiltration by neutrophils. The deep dermis shows abundant haphazard fibroplasia there are no organisms seen.(Figure 13)
Eumycotic mycetoma
A 21-year old male came with the complaints of painless swelling over right foot since 3 months. No history of trauma present.
On cutaneous examination
Single well defined hyperpigmented subcutaneous swelling with multiple discharging sinuses and mild scaling present over right dorsum of foot.(Figure 14)
Histopathology
Biopsy shows a diffuse dense suppurative granulomatous infiltrate on a background of granulation tissue. The granuloma consists of histiocytes, lymphocytes, epithelioid cells and several foreign body and Langhan’s giant cells with a central focus of suppuration. Within the suppurative centre are seen numerous variously shaped and sized grayish coloured grains that are surrounded by Splendore Hoeppli material. The dermis shows edema, mucin, numerous thick walled capillaries and fibroplasia. Overlying epidermis shows moderate irregular hyperplasia with focal spongiosis.(Figure 15)
Discussion
A total of six patients were involved in the study, of whom four were males and two were females. The male to female ratio was 2:1, with a slight male majority. The most common age group was 31-40 years for both males and females. Painful raised lesion for long duration was the predominant complaint among those patients. Out of these six rare chronic granulomatous diseases, bacterial infections were common than fungal infection. According to type of Granuloma, suppurative were most frequent (N=4; 66.66%) followed by Tuberculoid granuloma (N=2; 33.33%) which does not correlate with Queirós CS, Uva L et al. study. 2 which included all types of granulomatous diseases where necrobiotic granulomas were the most frequent (N = 111; 27.0%), followed by sarcoidal (N = 72; 17.5%), tuberculoid (N = 51; 12.4%), suppurative (N = 45; 10.9%), foreign body (N = 40; 9.7%), and xanthogranulomas (N = 26; 6.3%).
BOTRYOMYCOSIS is a chronic granulomatous and suppurative infection caused by STAPHYLOCOCCUS AUREUS and also by pseudomonas, E. coli, proteus, etc. developed subcutaneous swelling, followed by papule and nodule over the swelling which either developed, erosion, ulceration or sinus giving seropurulent discharge. The diagnosis of botryomycosis is usually confirmed by demonstration of specific bacteria in discharge, tissue culture and characteristic histopathology findings. The case in this study showed effective treatment response with sensitive antibiotics without the need of surgical intervention, which correlates with Sirka CS, Dash G et al. study. 3
Cervicofacial actinomycosis clinically manifests in three stages, initially presenting as soft swelling of the peri-mandibular area (stage 1), followed by woody hard induration and development of multiple sinus tracts and fistulas discharging purulent materials and sulfur granules (stage 2). Most patients with cervicofacial actinomycosis present in first or second stage. Later on, if left untreated, it can directly invade the cranium, or be disseminated hematogenously to involve the brain, lungs and abdominal cavity (stage 3). The case in our study presented in stage 2, which correlates with Dash, Behera et al. study. 4 where they mentioned most patients presented either in stage 1 and 2.The patient in our study showed complete resolution with Cap. Amoxicillin with clavulanic acid after 2 months of treatment which does not correlate with Dash, Behera et al. study. 4 where in their study it took 5 months for complete resolution with combination of Cap amoxicillin and Cap Doxycycline.
Cutaneous involvement in TB cases worldwide is observed in approximately 1-2% of all affected individuals and is commonly encountered, particularly in developing and tropical regions. The overall prevalence of cutaneous TB in various Indian studies is 0.25-0.6%.LV is a post-primary paucibacillary cutaneous TB that occurs in previously sensitized individuals with a moderate degree of immunity. It is usually a re-infection of TB of the skin and this is acquired either exogenously by direct inoculation of the bacilli or endogenously by hematogenous or lymphatic spread from an underlying infected focus. 5 In our study, we had a padiatric patient with multifocal lupus vulgaris along with Scrofuloderma, with two lupus vulgaris lesions over trunk, one over foot and scrofuloderma over neck, which does not correlate with Pugalia N, Madke B et al. study. 8 where they mentioned buttocks and extremities are commonly involved in the Indian subcontinent and can be explained by the risk of traumatic inoculation during outdoor work in the Indian subcontinent. The lesions showed significant resolution after 8 weeks of starting ATT, healing with hypopigmentation and atrophy which does not correlate with Maloney ME, Cohen B et al. study. 9 where in their study, they noted lesions to be healing as hyperpigmented plaques.
Both Tuberculosis and Leprosy are chronic granulomatous infections caused by intracellular Gram-positive aerobic acid-fast bacilli that multiply slowly and have long incubation periods. Patients with leprosy and TB co-infection, an association that is rarely reported at present, even in areas where both diseases are endemic. One possible explanation for the decrease in the reports of co-infected cases is BCG vaccination, which has shown to provide at least some partial protection against both diseases . 8 Treatment includes MBMDT, as appropriate for leprosy, should be given except rifampicin (which should continue as recommended for tuberculosis).Dermatologists should be aware of the importance of screening leprosy patients for latent or active tuberculosis, especially when they present immunosuppressive factors, such as long-term corticosteroid therapy or HIV, to prevent morbidity and mortality due to coinfection and to reduce the risk of acquired resistance to rifampicin, which is the greatest risk factor for this association. 10
Furuncle or boil is an infection of hair follicles with perifollicular inflammation with staphylococcus aureus. It presents as painful red nodule with pus discharge, commonly seen in axilla and buttocks treated with antibiotics. Sporotrichosis is a sub-cutaneous fungal infection caused by Sporothrix schenckii, characterized by ulcerated nodules along the lines of lymphatics. It can also cause systemic infection affecting lungs and can be disseminated, but lymphocutaneous form is the most common presentation. 11
Mycetoma is a localized chronic, suppurative, and deforming granulomatous infection seen in tropical and subtropical areas. It is a disorder of subcutaneous tissue, skin and bones, mainly of feet, characterized by a triad of localized swelling, underlying sinus tracts, and production of grains or granules. Etiological classification divides it into eumycetoma caused by fungus, and actinomycetoma caused by bacteria. Since the treatment of these two etiologies is entirely different, a definite diagnosis after histopathological and microbiological examination is mandatory, though difficult. The disease is very difficult to treat. In our study, the patient started showing response with just systemic triazole antifungal ( Itraconazole) which does not correlate with Relhan V, Mahajan K et al. study. 12 where they did complete surgical excision of the lesion followed by long courses of antifungals.
Conclusions
Most of the patients had a chronic history with improper treatment. Histopathology is a fundamental tool in the diagnosis of granulomatous skin diseases, allowing for the categorization of various types of granulomas and often guiding further investigation of these patients. So, it is imperative that the clinical diagnosis has to be confirmed with histopathology for the definitive diagnosis and appropriate treatment of these rare chronic infective granulomatous diseases. All these rare cases showed excellent progress after starting the right treatment.