- Visibility 1.6k Views
- Downloads 246 Downloads
- Permissions
- DOI 10.18231/j.ijced.2025.001
-
CrossMark
- Citation
Utility of artificial intelligence in dermatology: Challenges and perspectives
Abstract
Introduction: Medicine is entering a transformative era with disruptive technologies such as virtual reality, genomic prediction, data analytics, personalized medicine, stem cell therapy, 3-D printing, and nanorobotics. Dermatology is significantly impacted by these advancements, particularly through artificial intelligence (AI). AI, defined as devices performing functions typically requiring human intelligence, plays an increasingly prominent role in healthcare. John McCarthy coined the term AI in 1956. In dermatology, AI aids in diagnosis, treatment planning, and understanding diseases across communities. Machine learning and deep learning, subsets of AI, require extensive datasets and robust analysis to improve accuracy and performance.
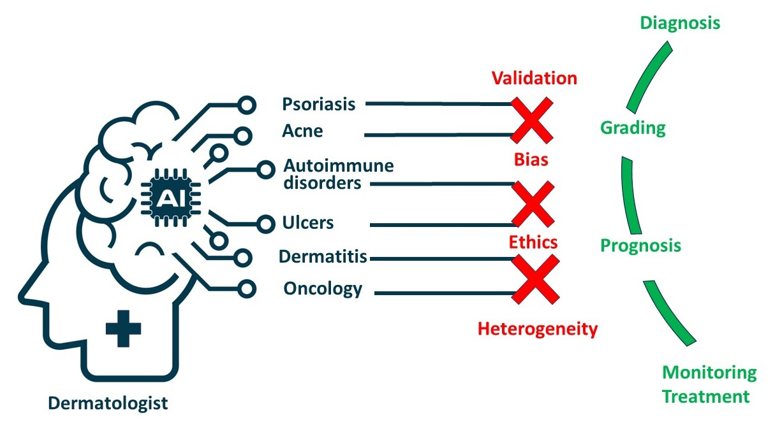
Discussion: AI's integration into dermatology is revolutionizing the field by enabling precision, reducing errors, and minimizing staffing needs. AI tools support dermatologists in diagnosing and treating various conditions, from psoriasis and acne to dermatitis and ulcers. Convolutional neural networks (CNNs) enhance the classification of skin lesions, while predictive models optimize treatment strategies based on patient data. AI's role extends to oncology, where it improves skin cancer detection through image analysis and histopathological assessment. Despite its potential, AI in dermatology faces challenges such as data quality, representativeness, algorithm transparency, and ethical considerations. Addressing biases, standardizing imaging protocols, and enhancing human-machine collaboration are crucial for maximizing AI's benefits.
Conclusion: AI holds immense promise in dermatology, offering innovative solutions to enhance patient care and diagnostic accuracy. The future of AI in dermatology includes advancements in vision-language models, federated learning, and precision medicine approaches. Overcoming challenges related to data privacy, regulatory standards, and model evaluation is essential for successful integration into clinical practice. Collaborative efforts among stakeholders are vital to drive progress and realize the full potential of AI, ultimately improving patient outcomes globally.
Introduction
Medicine stands at the precipice of a transformative era, ushered in by a multitude of potentially disruptive technologies. From virtual reality and genomic prediction of diseases to data analytics, personalized medicine, stem cell therapy, 3-D printing, and nanorobotics, the landscape of healthcare is rapidly evolving. [1], [2] Within this landscape, dermatology, the branch of medicine concerned with the diagnosis and treatment of skin conditions, is undergoing profound changes. Notably, computer algorithms have emerged as powerful tools, aiding dermatologists in diagnosis and the intersection of technology and medicine represents the burgeoning field of artificial intelligence (AI) in dermatology.[3]
AI is defined as “the ability of a device to perform functions normally associated with human intelligence, such as reasoning, learning, and self-development.” [4] It currently occupies a significant position in our lives and is getting progressively larger on an AI basis.[5] John McCarthy, a mathematician, coined the term AI in 1956.[6] As studies on AI continue to develop at an ever-increasing pace, there is no doubt that dentistry, along with many other disciplines, is set to change and advance.
AI execution has the potential to improve our knowledge of illnesses in different communities. By analyzing and extrapolating vast amounts of data, AI can provide a computerized analysis that could lead to a better understanding of various health conditions. It is appropriate to expect the use of terminologies like “digital transformations,” “digitalized workflows,” and “technical developments” owing to the technological advances in computer power, the accessibility of global information, along the widespread availability of large data that is currently ready for AI assessment. [7] Datasets for AI demand thorough analysis to improve their accuracy. The experts are required to invest time and effort to prepare the data to be used for successful learning. Machine learning is an algorithm that refers to the study of computer models that improve their performance by learning from experience without explicit instruction, therefore it requires sample data to make predictions or decisions. [8] On the other hand, deep learning and statistical learning are sub-branches of machine learning, which is a science under Computer Science or Computer Engineering. [9]
Dermatological practice and research are undergoing a rapid transformation owing to the advancements in AI. AI in dermatology is revolutionizing the discipline by enabling more precision, fewer errors, and a reduction in staffing needs. In dermatology clinics, AI is capable of performing an array of duties including appointment scheduling, clinical diagnosis support, and treatment planning.[10] General algorithms are a powerful tool for searching through large amounts of data efficiently they work by using the principle of survival of the fittest in natural selection, allowing them to find the best possible solutions to problems.
With the advancement of modern inventions and technology, the approach to the diagnosis and treatment of dermatological disorders has gone through substantial improvements. Dermatologists can now diagnose patients with skin disorders or even grade cancers more accurately as a result of AI algorithms.[11] An AI-powered method that assists in identifying and differentiating lesions is image analysis allows improved prognostication by dermatologists.[12] AI can assist the clinician in deciding the most suitable course of action based on patient data (age, sex, ethnicity), minimizing the likelihood of medical error and eventually maximizing patient outcomes. [13]
In the realm of dermatology, AI holds immense promise, primarily due to the discipline's rich repository of clinical, dermatoscopic, and dermatopathological image data. Understanding the fundamentals of AI is increasingly becoming essential for designing and interpreting medical studies in dermatology. The present manuscript aims to provide a comprehensive overview of the utility of AI in dermatology, examining both its current state and future prospects. By critically evaluating existing achievements and limitations, with a focus on their relevance in clinical practice, the review seeks to provide insights into the role of AI in shaping the future of dermatological care.
Discussion
The following text provides a comprehensive overview of the utility of AI in various aspects of dermatology:
Psoriasis
AI algorithms, particularly convolutional neural networks (CNNs), are being utilized to improve the classification of psoriasis through image recognition. [14] By analyzing digital images of skin lesions, these algorithms can accurately identify and classify psoriatic plaques, guttate psoriasis, inverse psoriasis, and other manifestations of the condition. [15] This aids dermatologists in making accurate diagnoses and tracking disease progression over time.
Researchers are exploring the use of AI models to predict the response of psoriasis patients to biologic therapies. By analyzing various parameters collected at the initial visit, such as disease severity, patient demographics, clinical history of psoriasis, and genetic markers, these models can forecast how individuals are likely to respond to specific biological treatments. [16] This predictive capability allows clinicians to tailor treatment strategies for each patient, optimizing outcomes and potentially reducing the need for trial-and-error approaches.
Machine learning models are also being developed to differentiate psoriasis from psoriatic arthritis using genetic markers. This is particularly valuable because psoriasis and psoriatic arthritis often coexist, and distinguishing between the two conditions can be challenging based solely on clinical presentation. [17], [18] By analyzing genetic data, AI algorithms can help clinicians accurately diagnose and manage both conditions, leading to more targeted and effective treatment approaches. [19]
Acne and other inflammatory dermal conditions
AI tools are revolutionizing the way dermatologists diagnose and manage this common skin condition.[20] By accurately delineating acne lesions and categorizing their severity, these AI systems assist dermatologists in tracking treatment progress and optimizing therapeutic interventions. Furthermore, AI has extended its application to the evaluation of rosacea lesions, demonstrating promising results in lesion counting and assessment, thus broadening its scope in inflammatory skin disease management. [21]
Beyond acne, AI is making significant strides in the identification and management of various other inflammatory skin conditions. Conditions such as lichen planus, pityriasis lichenoides, dermatomyositis, and seborrheic dermatitis are being targeted for AI-based solutions. [22] For example, machine learning techniques have been employed to classify different subtypes of myositis using ultrasound images, providing clinicians with valuable insights into disease presentation and progression. [23] Additionally, AI algorithms have been utilized to predict the sensitization potential in allergic contact dermatitis, offering a proactive approach to preventing adverse skin reactions. [24]
Studies have demonstrated that AI-based lesion-counting programs outperform manual counting performed by expert dermatologists, achieving high sensitivity and positive predictive values for various acne lesions such as papules, nodules, pustules, and whitehead comedones. [25] These advancements underscore the transformative potential of AI in dermatology, facilitating more accurate diagnosis, personalized treatment strategies, and improved patient outcomes across a spectrum of inflammatory skin diseases.
Dermatitis
Just as in psoriasis, AI algorithms are being employed to enhance the accuracy of diagnosing dermatitis from visual cues captured in images of skin lesions. [26], [27] These algorithms analyze various features and patterns in dermatitis lesions, enabling dermatologists to make more precise diagnoses and track disease progression more effectively.
Furthermore, AI models are being developed to predict the severity of atopic dermatitis, a common form of dermatitis characterized by inflamed, itchy skin. [27] By incorporating self-reported flare scores, patient demographics, and treatment history, these models can provide insights into the progression of the disease and help clinicians tailor treatment plans to individual patients' needs. This personalized approach to managing atopic dermatitis has the potential to improve patient outcomes and quality of life. [28]
In addition to diagnosis and severity prediction, AI is being utilized to prevent allergic contact dermatitis by predicting skin sensitization potential and the potency of substances. [29], [30] Traditionally, predictive screenings for sensitizing chemicals relied on animal models, such as the murine local lymph node assay. [31] However, there is a growing shift towards non-animal testing methods, such as the Genomic Allergen Rapid Detection assay, which measures transcriptional levels of genomic biomarkers. [32], [33] AI algorithms play a crucial role in analyzing the complex data generated by these assays, allowing researchers to identify patterns and signatures associated with skin sensitization and predict the potential allergenicity of various substances.
Ulcers
AI has proven to be a useful tool in the diagnosis and assessment of diabetic and pressure ulcers. [34], [35] These AI applications offer advanced capabilities for precise wound analysis, including the measurement of wound perimeter, surface area, depth, and composition. By accurately delineating wound boundaries and differentiating between various types of tissue involved, such as granulation, slough, and necrotic tissue, AI tools provide clinicians with objective and quantitative assessments of healing progression during treatment. [36]
One notable application described by Mukherjee et al. focuses on the classification of wound tissues, showcasing AI's ability to accurately identify and categorize different components of ulcerative lesions. [37] This capability not only aids in the diagnostic process but also facilitates treatment planning by providing clinicians with valuable insights into the nature and severity of the ulcer.
Moreover, AI-based risk prediction tools play a crucial role in pre-emptively identifying individuals at higher risk for developing pressure ulcers. By analyzing various clinical parameters and risk factors, these predictive models help clinicians anticipate and mitigate the likelihood of pressure injury occurrence, particularly among surgical critical care patients. [38] This proactive approach to ulcer management enables healthcare providers to implement preventive measures and interventions aimed at reducing the incidence and severity of pressure ulcers.
AI in dermatological oncology
The application of AI in skin cancer detection has garnered significant attention due to the rising incidence and financial burden associated with this disease. Conventional techniques for detecting skin cancer rely on visual and histopathological analysis, which may present limitations such as subjectivity and invasiveness. [39]
Several studies have demonstrated the effectiveness of AI, particularly deep learning algorithms, in classifying skin lesions and detecting melanoma. Nasr–Esfahani et al. and Stanford University conducted pioneering research in training neural networks for melanoma detection, achieving notable sensitivity and specificity. [40], [41] Subsequent studies by Fujisawa et al. and Han et al. further validated the utility of deep learning technology in skin cancer classification, showcasing high sensitivity and specificity comparable to dermatologists. [42], [43]
Furthermore, Brinker et al. showcased the superiority of automated dermoscopic melanoma image classification over dermatologists, highlighting the potential of AI to outperform human experts in lesion classification. [44] Despite these advancements, challenges such as external validity and the need for extensive training data persist.
In addition to clinical images, AI has ventured into histopathological analysis for skin cancer diagnosis. Hekler et al. demonstrated the ability of CNNs to outperform histopathologists in classifying histopathological melanoma images, underscoring the potential of AI as a complementary tool in histopathological assessment.[45] While AI in skin cancer diagnosis is still in its early stages, it shows considerable promise in revolutionizing dermatological practice. Smartphone applications leveraging AI algorithms for melanoma diagnosis have emerged, offering the potential for instant risk assessment. [46] However, concerns regarding false reassurance and missed diagnoses underscore the importance of continued research and validation.
Beyond skin cancer, AI holds promise in other dermatological domains such as atopic dermatitis and psoriasis. Gustafson et al. and De Guzman et al. demonstrated the utility of machine learning and artificial neural networks in phenotype identification and detection of atopic dermatitis from images, respectively.[47], [48] In psoriasis research, Guo et al. and Shrivastava et al. showcased the potential of AI in predicting psoriasis and risk assessment, offering opportunities for personalized treatment protocols. [49], [50]
Dermatopathology cancer diagnostics
The integration of artificial intelligence (AI) in dermatopathology, particularly with the advent of whole slide imaging (WSI), offers promising avenues for supporting dermatopathologists in various aspects, notably in skin cancer recognition. However, efforts to integrate patient data into CNN models have not shown significant improvement in performance.
Challenges remain in implementing AI in dermatopathology, including the potential for unreliable predictions when models encounter inputs that differ from their training datasets. [51] Conformal prediction has emerged as a potential solution to enhance the accuracy of predictions and flag unreliable results.
Studies focusing on diagnosing basal cell carcinoma (BCC) using whole-slide imaging have shown promising results. CNNs have achieved high sensitivity for detecting BCC, with some models demonstrating successful generalization to samples from different centers. [52], [53] Moreover, AI can help decrease pathologists' workload by automating the diagnosis of commonly encountered, low-risk entities like BCC.
AI has also shown promise in predicting sentinel lymph node status, visceral recurrence, and death based on the histology of primary melanoma tumors. [54], [55] Furthermore, AI could assist in identifying mitotic figures, delineating tumor margins, and interpreting immunohistochemistry stains, potentially recommending additional diagnostic tests. [56]
The clinical implementation of AI in dermatology faces several barriers that need to be addressed for successful integration into practice. Ensuring consistently high-quality images is essential for accurate AI predictions. Factors such as inadequate focus, lighting, resolution, and color representation can significantly impact prediction performance. [51] Clinics face challenges in obtaining high-quality images due to limited time, insufficient training, and inadequate equipment. [57] Guidelines for skin lesion imaging and patient education strategies can help improve image quality. Additionally, incorporating immediate feedback features for image quality in digital applications shows promise.
AI models can inadvertently perpetuate biases present in training data, leading to disparities in healthcare outcomes. Models trained on datasets consisting mainly of lighter skin tones may have lower performance for lesions on darker skin tones, exacerbating health inequities. [58], [59] Efforts to collect diverse datasets and transparency in dataset characteristics are crucial to address algorithmic bias and ensure equitable healthcare outcomes.
Thorough validation of AI models is essential before clinical implementation. Validation should involve computational stress testing using large external datasets to ensure efficacy in real-world clinical scenarios. [60] Publicly shared models and benchmarks, along with accessible databases, facilitate comprehensive validation. Rigorous testing for unintended biases and robustness to image variations is necessary to understand the model's limitations and reasons for errors.[61] While AI in dermatopathology is still evolving, it holds immense promise for enhancing diagnostic accuracy, reducing pathologists' workload, and improving patient outcomes. Continued research and validation are crucial for realizing the full potential of AI in dermatopathology and its integration into clinical practice.
Other applications
AI has found diverse applications across various dermatological conditions, expanding beyond the realm of skin cancer diagnosis. For instance, in acne management, smartphone applications have been developed to grade and classify acne lesions, providing patients and clinicians with a convenient tool for monitoring treatment progress. [20] Similarly, in the case of onychomycosis, diagnostic accuracy has been significantly enhanced using deep learning AI, leveraging a vast reference set of images to improve detection and classification. [62]
Moreover, AI technologies play a crucial role in predicting skin sensitization substances and analyzing the physiochemical properties of substances to determine their sensitizing potential. [29], [30], [31], [32] These applications aid in risk assessment and preventive measures, particularly in occupational settings where exposure to sensitizing agents is common.
Tele-dermatology represents another area where AI integration has revolutionized clinical practice, especially in regions with limited access to dermatologists. [63] Smartphone applications equipped with AI capabilities enable the capture of skin lesions and relevant clinical information, facilitating remote consultation and referral when necessary. This has become particularly relevant during the COVID-19 pandemic, where telemedicine has become a critical component of healthcare delivery. [64]
Furthermore, AI serves as an educational tool for dermatologists, researchers, students, and skin cancer specialists. [65] By providing access to visually similar images and case studies, AI platforms enhance learning and diagnostic skills, empowering medical professionals to make accurate diagnoses and treatment decisions. In face-to-face assessment, AI augments the diagnostic process by collaborating with human dermatologists, leveraging the expertise of both to achieve more accurate and comprehensive evaluations of skin conditions. This collaborative approach maximizes diagnostic accuracy and improves patient care outcomes.
Pitfalls and drawbacks
AI holds immense potential in revolutionizing dermatological practice, but it is not without limitations. One significant challenge lies in the quality and representativeness of the data used to train AI algorithms. Deep learning neural networks rely on vast amounts of data, which can be scarce for diseases with low prevalence or when data is not representative of diverse populations. Moreover, heterogeneity across medical datasets and the complexity of neural networks can lead to overfitting, where models perform well on training data but fail to generalize to new cases. [66] Additionally, the accuracy of AI applications is contingent upon the quality and accuracy of input data, emphasizing the importance of data accuracy and infrastructure for data sharing.
Despite technological advancements, acceptance of AI in dermatology remains a challenge. Clinical diagnosis in dermatology relies heavily on detailed history-taking, thorough clinical examination, and complementary investigations. [67] The human touch and holistic approach integral to patient care cannot be replaced by algorithms alone. Histopathology continues to serve as the gold standard for diagnosis, underscoring the enduring role of traditional diagnostic methods in dermatology practice.
Another limitation is the "black box" problem inherent in AI reasoning. Traditional clinical decision-making involves understanding the rationale behind each decision, which contrasts with the opaque nature of AI algorithms. [68] It can be challenging to interpret how specific features or calculations contribute to AI-generated outputs, posing challenges to trust and transparency in AI-driven diagnostics.
Legal liability and ethical considerations further complicate the integration of AI into dermatological practice. [69] Privacy concerns arise from the large datasets required for AI training, raising questions about patient consent and data protection. Additionally, in the event of adverse outcomes, accountability and liability remain ambiguous, necessitating the establishment of ethical guidelines and regulatory frameworks.
Bias is another critical issue in AI applications, where algorithms may inherit biases from training data or inadvertently learn biased patterns. Lack of diversity in training data can lead to underperformance on images from diverse populations, exacerbating existing healthcare inequities. [70] Moreover, there are concerns about the potential job displacement resulting from AI implementation, although some experts argue that AI can enhance diagnostic efficacy and patient care rather than replace human dermatologists. [71]
The generalizability of AI models is another limitation, with most studies based on data from Western populations and developed nations. The findings may not be applicable globally, highlighting the need for diverse and representative datasets from different regions and populations. Technical challenges such as image quality variability and standardization further hinder AI implementation in dermatology. [70] Standardizing image acquisition and establishing quality standards are crucial for ensuring consistent and accurate AI diagnostics. Moreover, the interpretability of AI outputs remains a challenge, as complex algorithms may generate decisions without human-understandable reasoning.
Addressing these limitations requires interdisciplinary collaboration and ongoing research to develop robust, transparent, and equitable AI algorithms. Moreover, ethical guidelines, regulatory frameworks, and standardized protocols are essential to ensure the responsible and effective integration of AI into dermatological practice. Despite these challenges, AI holds promise in transforming dermatological care, provided that its limitations are adequately addressed and mitigated.
Addressing the limitations
To address the limitations of AI in dermatology, several strategies can be employed to enhance the performance and applicability of existing algorithms. Firstly, expanding the training datasets for CNNs to reflect the diversity of the general population is crucial. With increasing immigration and globalization, clinicians are encountering patient populations with diverse ethnicities and skin types. Therefore, training algorithms on a broader range of images from different ethnicities can improve their performance across various populations. Currently, most algorithms are trained on datasets predominantly comprising Caucasian or Asian patients, but early screening of patients with skin of color could be more beneficial, given the higher incidence of advanced disease and lower survival rates in this population.
In addition to diversifying training datasets, the inclusion of metadata for patients under examination is essential. Metadata such as age, gender, skin type, and anatomical location can provide valuable contextual information for both clinicians and algorithms. Integrating clinical metadata into AI training can create a more realistic diagnostic environment, mirroring the diagnostic approach of clinicians who consider a patient's history in their assessments. Studies integrating clinical metadata have shown promising results, indicating improved classifier accuracy compared to CNNs alone. [72]
Clinical close-up images offer additional insights that may not be visible under dermoscopy alone. Combining clinical and dermoscopic image analysis through combined CNNs can improve algorithm performance. [73] These datasets of clinical images have the potential to train algorithms for smartphone applications, enhancing diagnostic capabilities outside clinical settings. Addressing confounding factors in images is another critical strategy to improve algorithm performance. Techniques such as image segmentation can separate lesions from background artifacts, enhancing algorithm accuracy. [74] Although segmentation may introduce new challenges, controlling segmentation quality can mitigate potential pitfalls.
Moreover, validating algorithms using out-of-distribution data from different sources can enhance their generalizability. Currently, most validation studies use holdout data exclusively, limiting the assessment of algorithm performance in diverse clinical settings. [75] Future research should consider incorporating these images to evaluate classifier performance under varying conditions.
Collaboration between human clinicians and AI systems is crucial for maximizing diagnostic accuracy. Studies have shown that combining the expertise of dermatologists with AI algorithms can improve diagnostic outcomes. [71] Instead of viewing AI as a replacement for human clinicians, integrating AI as a supportive tool in clinical decision-making can enhance overall diagnostic efficacy.
Standardizing imaging protocols through the use of Digital Imaging and Communications in Medicine (DICOM) standards is essential for ensuring data quality and interoperability. DICOM enables the attachment of supplementary metadata and lesion classification outputs to medical images, facilitating data exchange and external validation of AI algorithms. [76] Additionally, DICOM's de-identification profiles protect patient privacy in clinical trials, addressing ethical concerns associated with AI implementation.
The overall utility of AI in dermatology, and various hurdles in achieving the outcomes is depicted in [Figure 1]. By implementing these strategies, the dermatological community can overcome the limitations of AI and harness its full potential to improve patient care and diagnostic accuracy in dermatology.
Future prospects
The future of AI in dermatology holds tremendous promise, with several exciting directions and opportunities on the horizon. Language models, particularly Vision-Language Models (VLMs), are emerging as powerful tools in dermatology. [77] VLMs, capable of associating visual inputs like images with text data, offer vast potential in diagnosis, treatment planning, and patient data analysis. These models could evolve into generalist medical AI capable of providing approximate diagnoses, treatment options, and deeper insights by integrating various patient data types. As computing power increases and datasets expand, these models are poised to become more accurate and versatile, augmenting dermatological practice to provide more precise and holistic care.
Accessing medical data, including dermatological images, poses challenges due to privacy and legal concerns. Federated learning offers a solution by enabling distributed training of AI models across multiple institutions without sharing raw data. [78] This approach preserves data privacy while harnessing diverse datasets to improve model performance. Additionally, the concept of Federated Models introduces the potential for local models fine-tuned with institutional data, offering insights tailored to specific demographics and guidelines. [79] Despite challenges, these models hold promise in building more generalizable and contextually relevant dermatology AI models.
The integration of AI algorithms into clinical practice requires careful consideration of their utility and impact. Human-machine collaboration, aided by AI in time-consuming tasks such as lesion mapping and naevus count, shows promise for improving patient care. [71] Precision medicine approaches leveraging ML algorithms can enable personalized risk stratification and surveillance for melanoma patients. Teledermatology and smartphone apps, powered by CNN algorithms, have the potential to enhance screening, awareness, and accessibility to dermatological care, ultimately improving patient outcomes. [63], [64]
Conclusion
The burgeoning field of AI in dermatology represents a transformative opportunity to enhance patient care, diagnosis, and treatment. As AI technologies continue to evolve, they offer innovative solutions to longstanding challenges in dermatological practice, from improving diagnostic accuracy and treatment planning to expanding access to care through teledermatology and smartphone applications. However, realizing the full potential of AI in dermatology requires addressing key considerations such as data privacy, model evaluation, regulatory standards, and the integration of AI into clinical workflows. Collaborative efforts among dermatologists, researchers, policymakers, and industry stakeholders are essential to drive forward progress in this exciting and rapidly advancing field, ultimately improving outcomes for patients worldwide.
Source of Funding
None.
Conflict of Interest
None.
References
- Alzoubi L, Aljabali AA, Tambuwala MM. Empowering precision medicine: the impact of 3D printing on personalized therapeutic. AAPS Pharm Sci Tech. 2023;24(8). [Google Scholar] [Crossref]
- Hu M, Ge X, Chen X, Mao W, Qian X, Yuan WE. Micro/Nanorobot: A Promising Targeted Drug Delivery System. Pharmaceutics. 2020;12(7). [Google Scholar] [Crossref]
- Venkatesh K, Raza M, Nickel G, Wang S, Kvedar J. Deep learning models across the range of skin disease. NPJ Digit Med. 2024;7(1). [Google Scholar] [Crossref]
- Gavriushenko M, Kaikova O, Terziyan V. Bridging human and machine learning for the needs of collective intelligence development. Procedia Manufacturing. 2020;42:302-6. [Google Scholar] [Crossref]
- James G, Witten D, Hastie T, Tibshirani R. . An Introduction to Statistical Learning with Application in R. 2013. [Google Scholar]
- Rajaraman V. John McCarthy – Father of Artificial Intelligence. Resonance. 2014;19:198-207. [Google Scholar] [Crossref]
- Marques I, Ferreira J. Digital transformation in the area of health: systematic review of 45 years of evolution. Health Technol. 2020;10(3):575-86. [Google Scholar] [Crossref]
- Sarker I. Machine Learning: Algorithms, Real-World Applications and Research Directions. SN Comput Sci. 2021;2(3). [Google Scholar] [Crossref]
- Frank M, Drikakis D, Charissis V. Machine-Learning Methods for Computational Science and Engineering. Computation. 2020;8. [Google Scholar] [Crossref]
- Patel S, Wang J, Motaparthi K, Lee J. Artificial intelligence in dermatology for the clinician. Clin Dermatol. 2021;39(4):667-72. [Google Scholar]
- De A, Sarda A, Gupta S, Das S. Use of Artificial Intelligence in Dermatology. Indian J Dermatol. 2020;65(5):352-7. [Google Scholar]
- Li Z, Koban KC, Schenck TL, Giunta RE, Li Q, Sun Y. Artificial Intelligence in Dermatology Image Analysis: Current Developments and Future Trends. J Clin Med. 2022;11(22). [Google Scholar] [Crossref]
- Young A, Xiong M, Pfau J, Keiser M, Wei M. Artificial intelligence in dermatology: A primer. J Invest Dermatol. 2020;140(8):1504-12. [Google Scholar]
- Schaap M, Cardozo N, Patel A, Jong Ed, BG, MS. Image-based automated Psoriasis Area Severity Index scoring by Convolutional Neural Networks. J Eur Acad Dermatol Venereol. 2022;36(1):68-75. [Google Scholar]
- Rashid M, Gilanie G, Naveed S, Cheema S, Sajid M. . Signal Image Video Process. 2024;18:163-72. [Google Scholar] [Crossref]
- Bagel J, Wang Y, Montgomery IP, Abaya C, Andrade E, Boyce C. A Machine Learning-Based Test for Predicting Response to Psoriasis Biologics. SKIN J Cutan Med. 2021;5(6):621-38. [Google Scholar]
- Shapiro J, Getz B, Cohen S, Jenudi Y, Underberger D, Dreyfuss M. Evaluation of a machine learning tool for the early identification of patients with undiagnosed psoriatic arthritis-A retrospective population-based study. J Transl Autoimmun. 2023;7. [Google Scholar] [Crossref]
- Achararit P, Manaspon C, Jongwannasiri C, Phattarataratip E, Osathanon T, Sappayatosok K. Artificial intelligence-based diagnosis of oral lichen planus using deep convolutional neural networks. Eur J Dent. 2023;17(4):1275-82. [Google Scholar]
- Rosa JD, Kim J, Tian S, Tomalin L, Krueger J, Suárez-Fariñas M. Shrinking the psoriasis assessment gap: early gene-expression profiling accurately predicts response to long-term treatment. J Invest Dermatol. 2017;137(2):305-12. [Google Scholar]
- Seite S, Khammari A, Benzaquen M, Moyal D, Dréno B. Development and accuracy of an artificial intelligence algorithm for acne grading from smartphone photographs. Exp Dermatol. 2019;28(11):1252-7. [Google Scholar]
- Gerges F, Shih F, Azar D. Automated diagnosis of acne and rosacea using convolution neural networks. . 2021. [Google Scholar]
- Xu X, Chen B, Huang J, Yang J, Li M. Seborrheic dermatitis-distributed rash in dermatomyositis is associated with progressive interstitial lung disease. J Am Acad Dermatol. 2021;84(6):1694-6. [Google Scholar]
- Uçar E. Classification of myositis from muscle ultrasound images using deep learning. Biomed Signal Process Control. 2022;71( Part B). [Google Scholar] [Crossref]
- Fortino V, Wisgrill L, Werner P, Suomela S, Linder N, Jalonen E. Machine-learning-driven biomarker discovery for the discrimination between allergic and irritant contact dermatitis. Proc Natl Acad Sci U S A. 2020;117(52):33474-85. [Google Scholar]
- Kim D, Sun S, Cho S, Kong H, Lee J, Lee J. Automated Facial Acne Lesion Detecting and Counting Algorithm for Acne Severity Evaluation and Its Utility in Assisting Dermatologists. Am J Clin Dermatol .. 2023;24(4):649-59. [Google Scholar]
- Guimarães P, Batista A, Zieger M, Kaatz M, Koenig K. Artificial Intelligence in Multiphoton Tomography: Atopic Dermatitis Diagnosis. Sci Rep. 2020;10(1). [Google Scholar] [Crossref]
- Maulana A, Noviandy T, Suhendra R, Earlia N, Bulqiah M, Idroes G. Evaluation of atopic dermatitis severity using artificial intelligence. Narra J. 2023;3(3). [Google Scholar] [Crossref]
- Paul C, Griffiths C, Costanzo A, Herranz P, Grond S, Mert C. Factors predicting quality of life impairment in adult patients with atopic dermatitis: results from a patient survey and machine learning analysis. Dermatol Ther (Heidelb). 2023;13(4):981-95. [Google Scholar]
- Kalicińska J, Wiśniowska B, Polak S, Spiewak R. Artificial Intelligence That Predicts Sensitizing Potential of Cosmetic Ingredients with Accuracy Comparable to Animal and In Vitro Tests-How Does the Infotechnomics Compare to Other “Omics” in the Cosmetics Safety Assessment. Int J Mol Sci. 2023;24(7). [Google Scholar] [Crossref]
- Im JE, Lee J, Kim H, Kim H, Seo D, Kim K. Prediction of skin sensitization using machine learning. Toxicol Vitro. 2023;93. [Google Scholar] [Crossref]
- Ambe K, Suzuki M, Ashikaga T, Tohkin M. Development of quantitative model of a local lymph node assay for evaluating skin sensitization potency applying machine learning CatBoost. Regul Toxicol Pharmacol. 2021;125. [Google Scholar] [Crossref]
- Masinja W, Elliott C, Modi S, Enoch S, Cronin M, Mcinnes E. Comparison of the predictive nature of the Genomic Allergen Rapid Detection (GARD) assay with mammalian assays in determining the skin sensitisation potential of agrochemical active ingredients. Toxicol In Vitro. 2021;70. [Google Scholar] [Crossref]
- Ogulur I, Pat Y, Ardicli O, Barletta E, Cevhertas L, Fernandez-Santamaria R. Advances and highlights in biomarkers of allergic diseases. Allergy. 2021;76(12):3659-86. [Google Scholar]
- Pappachan J, Cassidy B, Fernandez C, Chandrabalan V, Yap M. The role of artificial intelligence technology in the care of diabetic foot ulcers: the past, the present, and the future. World J Diabetes. 2022;13(12):1131-9. [Google Scholar]
- Ribeiro F, Fidalgo F, Silva A, Metrôlho J, Santos O, Dionisio R. Literature review of machine-learning algorithms for pressure ulcer prevention: Challenges and opportunities. Informatics. 2021;8(4). [Google Scholar] [Crossref]
- Anisuzzaman D, Wang C, Rostami B, Gopalakrishnan S, Niezgoda J, Yu Z. Image-based artificial intelligence in wound assessment: A systematic review. Adv Wound Care (New Rochelle). 2022;11(12):687-709. [Google Scholar]
- Mukherjee R, Manohar D, Das D, Achar A, Mitra A, Chakraborty C. Automated tissue classification framework for reproducible chronic wound assessment. Biomed Res Int. 2014. [Google Scholar] [Crossref]
- Toffaha K, Simsekler M, Omar M. Leveraging artificial intelligence and decision support systems in hospital-acquired pressure injuries prediction: A comprehensive review. Artif Intell Med. 2023;141. [Google Scholar] [Crossref]
- Heibel H, Hooey L, Cockerell C. A review of noninvasive techniques for skin cancer detection in dermatology. Am J Clin Dermatol. 2020;21(4):513-24. [Google Scholar]
- Nasr-Esfahani E, Samavi S, Karimi N, Soroushmehr S, Jafari M, Ward K. Melanoma detection by analysis of clinical images using convolutional neural network. Annu Int Conf IEEE Eng Med Biol Soc. 2016. [Google Scholar] [Crossref]
- Esteva A, Kuprel B, Novoa R, Ko J, Swetter S, Blau H. Dermatologist-level classification of skin cancer with deep neural networks. Nature. 2017;542(7639):115-8. [Google Scholar]
- Fujisawa Y, Inoue S, Nakamura Y. The Possibility of Deep Learning-Based, Computer-Aided Skin Tumor Classifiers. Front Med (Lausanne). 2019;6. [Google Scholar] [Crossref]
- Han X, Wang L, Seo SH, He J, Jung T. Measuring Perceived Psychological Stress in Urban Built Environments Using Google Street View and Deep Learning. Front Public Health. 2022;10. [Google Scholar] [Crossref]
- Brinker TJ, Hekler A, Enk A, Berking C, Haferkamp S, Hauschild A. Deep neural networks are superior to dermatologists in melanoma image classification. Eur J Cancer. 2019;119:11-7. [Google Scholar] [Crossref]
- Hekler A, Utikal J, Enk A, Berking C, Klode J, Schadendorf D. Pathologist-level classification of histopathological melanoma images with deep neural networks. Eur J Cancer. 2019;115:79-83. [Google Scholar] [Crossref]
- Wei M, Tada M, So A, Torres R. Artificial intelligence and skin cancer. Front Med. 2024;11. [Google Scholar] [Crossref]
- Gustafson E, Pacheco J, Wehbe F, Silverberg J, Thompson W. A machine learning algorithm for identifying atopic dermatitis in adults from electronic health records. Proc (IEEE Int Conf Healthc Inform). 2017. [Google Scholar] [Crossref]
- Guzman LD, Maglaque R, Torres V, Zapido S, Cordel M. Design and Evaluation of a Multi-model, Multi-level Artificial Neural Network for Eczema Skin Lesion Detection. IEEE Int Conf Artif Intell Model Simul. 2015. [Google Scholar] [Crossref]
- Zhou J, Li Y, Guo X. Predicting psoriasis using routine laboratory tests with random forest. PLoS One. 2021;16(10). [Google Scholar] [Crossref]
- Dan D, Srivastava N. Psoriasis: Striving for Potential Biomarkers. Assay Drug Dev Technol. 2023;21(6):235-57. [Google Scholar]
- Grzybowski A, Jin K, Wu H. Challenges of artificial intelligence in medicine and dermatology. Clin Dermatol. 2024;42(3):210-5. [Google Scholar]
- Jiang Y, Xiong J, Li H, Yang X, Yu W, Gao M. Recognizing basal cell carcinoma on smartphone-captured digital histopathology images with a deep neural network. Br J Dermatol. 2020;182(3):754-62. [Google Scholar]
- Zon MV, Waa JVD, Veta M, Krekels G. Whole-slide margin control through deep learning in Mohs micrographic surgery for basal cell carcinoma. Exp Dermatol. 2021;30(5):733-8. [Google Scholar]
- Brinker T, Kiehl L, Schmitt M, Jutzi T, Krieghoff-Henning E, Krahl D. Deep learning approach to predict sentinel lymph node status directly from routine histology of primary melanoma tumours. Eur J Cancer. 2021;154:227-34. [Google Scholar] [Crossref]
- Kulkarni P, Robinson E, Pradhan JS, Gartrell-Corrado R, Rohr B, Trager M. Deep learning based on standard H&E images of primary melanoma tumors identifies patients at risk for visceral recurrence and death. Clin Cancer Res. 2020;26(5):1126-34. [Google Scholar]
- Garcia M, Antonio M. Automated Diagnosis of Seven Major Skin Tumors in Canines Using a Convolutional Neural Network (CNN) on H&E-Stained Whole Slide Images (WSI) [dissertation. Freie Universitaet Berlin (Germany). 2022. [Google Scholar]
- Gomolin A, Netchiporouk E, Gniadecki R, Litvinov I. Artificial Intelligence Applications in Dermatology: Where Do We Stand?. Front Med (Lausanne). 2020;7. [Google Scholar] [Crossref]
- Heldreth CM, Monk E, Clark A, Schumann C, Eyee X, Ricco S. Which Skin Tone Measures Are the Most Inclusive? An Investigation of Skin Tone Measures for Artificial Intelligence. ACM J Responsible Comput. 2024;1(1):1-21. [Google Scholar] [Crossref]
- Fliorent R, Fardman B, Podwojniak A, Javaid K, Tan I, Ghani H. Artificial intelligence in dermatology: advancements and challenges in skin of color. Int J Dermatol. 2024;63(4):455-61. [Google Scholar]
- Liopyris K, Gregoriou S, Dias J, Stratigos AJ. Artificial intelligence in dermatology: challenges and perspectives. Dermatol Ther. 2022;12(12):2637-51. [Google Scholar]
- Combalia M, Codella N, Rotemberg V, Carrera C, Dusza S, Gutman D. Validation of artificial intelligence prediction models for skin cancer diagnosis using dermoscopy images: the 2019 International Skin Imaging Collaboration Grand Challenge. Lancet Digit Health. 2022;4(5):330-9. [Google Scholar]
- Lim S, Ohn J, Mun J. Diagnosis of Onychomycosis: From Conventional Techniques and Dermoscopy to Artificial Intelligence. Front Med (Lausanne). 2021;8. [Google Scholar] [Crossref]
- Giansanti D. Advancing Dermatological Care: A Comprehensive Narrative Review of Tele-Dermatology and mHealth for Bridging Gaps and Expanding Opportunities beyond the COVID-19 Pandemic. Healthcare (Basel). 2023;11(13). [Google Scholar] [Crossref]
- Kanwal S, Tabassum S, Qadri P. Real-time tele dermatology in assessing clinical outcomes of skin diseases. Rawal Med J. 2022;47(4):1005-8. [Google Scholar]
- Wells A, Patel S, Lee JB, Motaparthi K. Artificial intelligence in dermatopathology: Diagnosis, education, and research. J Cutan Pathol. 2021;48(8):1061-8. [Google Scholar]
- Yu F, Moehring A, Banerjee O, Salz T, Agarwal N, Rajpurkar P. Heterogeneity and predictors of the effects of AI assistance on radiologists. Nat Med. 2024;30(3):837-49. [Google Scholar]
- Boch K, Schmidt E, Schmidt E. Medical History and Clinical Examination. Diseases of the Oral Mucosa: Study Guide and Review. 2021. [Google Scholar] [Crossref]
- Pierce R, Sterckx S, Biesen WV. A riddle, wrapped in a mystery, inside an enigma: How semantic black boxes and opaque artificial intelligence confuse medical decision-making. Bioethics. 2022;36(2):113-20. [Google Scholar]
- Naik N, Hameed B, Shetty D, Swain D, Shah M, Paul R. Legal and Ethical Consideration in Artificial Intelligence in Healthcare: Who Takes Responsibility?. Front Surg. 2022;9. [Google Scholar] [Crossref]
- Jacoba C, Celi L, Lorch A, Fickweiler W, Sobrin L, Gichoya J. Bias and Non-Diversity of Big Data in Artificial Intelligence: Focus on Retinal Diseases: “Massachusetts Eye and Ear Special Issue. Semin Ophthalmol. 2023;38(5):433-41. [Google Scholar]
- Tschandl P, Rinner C, Apalla Z, Argenziano G, Codella N, Halpern A. Human-computer collaboration for skin cancer recognition. Nat Med. 2020;26(8):1229-34. [Google Scholar]
- Ningrum D, Yuan S, Kung W, Wu C, Tzeng I, Huang C. Deep learning classifier with patient’s metadata of dermoscopic images in malignant melanoma detection. J Multidiscip Healthc. 2021;14:877-85. [Google Scholar] [Crossref]
- Olayah F, Senan EM, Ahmed IA, Awaji B. AI techniques of dermoscopy image analysis for the early detection of skin lesions based on combined CNN features. Diagnostics. 2023;13(7). [Google Scholar] [Crossref]
- Hung K, Yeung A, Tanaka R, Bornstein M. Current applications, opportunities, and limitations of AI for 3D imaging in dental research and practice. Int J Environ Res Public Health. 2020;17(12). [Google Scholar] [Crossref]
- Bradshaw T, Huemann Z, Hu J, Rahmim A. A guide to cross-validation for artificial intelligence in medical imaging. Radiol Artif Intell. 2023;5(4). [Google Scholar] [Crossref]
- Caffery L, Rotemberg V, Weber J, Soyer H, Malvehy J, Clunie D. The role of DICOM in artificial intelligence for skin disease. Front Med. 2021;7. [Google Scholar] [Crossref]
- Lin B, Xu Y, Bao X, Zhao Z, Zhang Z, Wang Z. SkinGEN: an Explainable Dermatology Diagnosis-to-Generation Framework with Interactive Vision-Language Models. arXiv. 2024. [Google Scholar] [Crossref]
- Xu G, Wu Y, Hu J, Shi Y. Achieving Fairness in Dermatological Disease Diagnosis through Automatic Weight Adjusting Federated Learning and Personalization. arXiv. 2022. [Google Scholar] [Crossref]
- Yaqoob M, Alsulami M, Khan M, Alsadie D, Saudagar A, Alkhathami M. Federated Machine Learning for Skin Lesion Diagnosis: An Asynchronous and Weighted Approach. Diagnostics (Basel). 2023;13(11). [Google Scholar] [Crossref]
- Abstract
- Introduction
- Discussion
- Psoriasis
- Acne and other inflammatory dermal conditions
- Dermatitis
- Ulcers
- AI in dermatological oncology
- Dermatopathology cancer diagnostics
- Other applications
- Pitfalls and drawbacks
- Addressing the limitations
- Future prospects
- Conclusion
- Source of Funding
- Conflict of Interest
- References
How to Cite This Article
Vancouver
Tafti F, Sachdev SS, Thorat R, Kshirsagar M, Pinge S, Savant S. Utility of artificial intelligence in dermatology: Challenges and perspectives [Internet]. IP Indian J Clin Exp Dermatol. 2025 [cited 2025 Oct 18];11(1):1-9. Available from: https://doi.org/10.18231/j.ijced.2025.001
APA
Tafti, F., Sachdev, S. S., Thorat, R., Kshirsagar, M., Pinge, S., Savant, S. (2025). Utility of artificial intelligence in dermatology: Challenges and perspectives. IP Indian J Clin Exp Dermatol, 11(1), 1-9. https://doi.org/10.18231/j.ijced.2025.001
MLA
Tafti, Farheen, Sachdev, Sanpreet Singh, Thorat, Rohit, Kshirsagar, Minal, Pinge, Sujata, Savant, Suyog. "Utility of artificial intelligence in dermatology: Challenges and perspectives." IP Indian J Clin Exp Dermatol, vol. 11, no. 1, 2025, pp. 1-9. https://doi.org/10.18231/j.ijced.2025.001
Chicago
Tafti, F., Sachdev, S. S., Thorat, R., Kshirsagar, M., Pinge, S., Savant, S.. "Utility of artificial intelligence in dermatology: Challenges and perspectives." IP Indian J Clin Exp Dermatol 11, no. 1 (2025): 1-9. https://doi.org/10.18231/j.ijced.2025.001
