- Visibility 238 Views
- Downloads 33 Downloads
- DOI 10.18231/j.ijced.2025.016
-
CrossMark
- Citation
Prospective hospital based study of non-venereal dermatoses of external genitalia at tertiary care institute
- Author Details:
-
Rachana Shekar
-
Pavithra Gundappa *
-
Ranjitha M L
Introduction
‘Nonvenereal disease’ is defined as the group of disorders involving the genitalia, which are not transmitted sexually.[1] It includes, two groups of disorders.[1] Firstly, disorders which affect only the external genitalia and the second group includes disorders that affect the genitalia and other parts of the body.[1] Nonvenereal diseases which are peculiar to external genitalia are plasma cell balanitis, Peyronie’s disease, lichen planus of genitalia, lichen sclerosus et atrophicus, fournier’s gangrene, Behcet’s disease, angiokeratoma of Fordyce, nonvenereal sclerosing lymphangitis, phimosis and paraphimosis.[2]
Various physiological, developmental, infective and inflammatory, traumatic, tumorous and miscellaneous conditions affect genitalia. Physiological variants in males includes pearly penile papules, achrochordons, sebaceous prominence, angiomas and angiokeratomas.[3] Physiological variants in females include angiokeratoma, sebaceous gland hyperplasia, vestibular papillomatosis and varicosities of the labial veins.[3]
Based on etiopathogenesis, nonvenereal genital dermatoses are classified in to: inflammatory disorders (genital psoriasis, lichen planus, lichen sclerosus, seborrheic dermatitis), infections and infestations (dermatophytosis and scabies), exogenous causes (irritant contact dermatitis, topical corticosteroid abuse, adverse drug reactions : fixed drug eruption, SJS/TEN), pigmentary disorders (vitiligo), multisystem disorders (Behcet’s disease, Reiter syndrome, inflammatory bowel diseases), benign conditions(achrochordons, scrotal calcinosis, angiokeratoma, sebaceous cyst), premalignant (erythroplasia of Queyrat) and malignant (squamous cell carcinoma).[4], [5]
Since non venereal dermatoses includes wide variety of disorders, it is essential to differentiate between venereal and nonvenereal genital dermatoses, as these disorders create apprehension among patients.
Aims and Objectives
To evaluate the frequency of non-venereal diseases of external genitalia.
To determine the clinical and demographic pattern of non-venereal diseases of external genitalia.
Materials and Methods
This study was conducted from February 2016 to February 2017 at a tertiary care institute, after obtaining approval from the institution ethics committee. The study population included all patients with nonvenereal diseases who attended the Dermatology outpatient department in the study period. Consecutive 100 patients with nonvenereal dermatoses were included in the study. Informed written consent was taken. Detailed history including age, sex, chief complaints, onset and duration of the disease, site of affection, associated medical disorders, cutaneous condition and history of exposure were taken in a pre-structured proforma. Thorough general and physical examination of genitalia and other body parts was done to look for associated lesions. Relevant investigations such as complete blood count, blood sugar, KOH smear, Tzanck smear, Gram stain, HIV and VDRL tests and biopsy were done as and when required.
Results
Total of 100 cases with nonvenereal diseases of genitalia were recorded for a period of one year. Of which 10 were children. Male: female = 2.2: 1. Age ranged from 4 years to 81 years with mean age of 38 (among males) & 37.33 (among females). 72 patients (72%) were married.
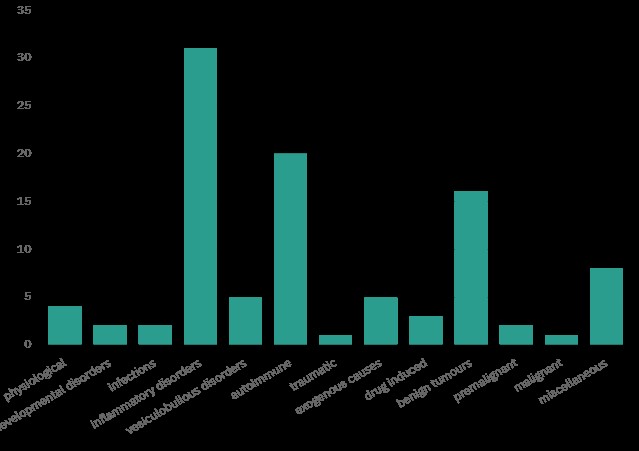
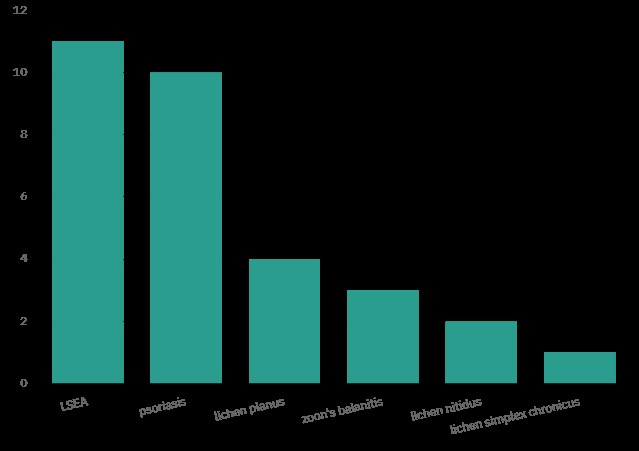







In our study total of 34 different types of nonvenereal genital dermatoses were noted. Frequency of non-venereal genital dermatoses and frequency of inflammatory causes depicted in bar [Figure 1], [Figure 2] respectively. The most common presentation in this study was depigmented patch on the genitalia, followed by itching, raised lesions and erosions.
Most common were Steatocystoma multiplex (10) followed by psoriasis (9), vitiligo (7) in males. Most common was genital vitiligo (13) followed by LSEA (7) among females. Nonvenereal dermatoses affecting other sites were noted in 25 patients, most commonly in vitiligo followed by psoriasis. Associated sexually transmitted infection was noted in a single case.
Discussion
In our study majority of the patients were aged > 40 years (45%). This is in contrast to other studies where most of the patients aged between 21-30 years.
In our study, among 20 vitiligo patients [[Figure 3]], isolated genital vitiligo was found in 17 patients & 3 patients had associated extra-genital vitiligo. In this study vitiligo was observed in all groups similar to studies done by Garg et al, Hogade et al.[4], [5], [6] Females were affected more commonly. Youngest patient with genital vitiligo was 6 year old girl.
Lichen sclerosus, a chronic condition affecting skin and mucosa. It commonly affects the female genital skin. It may affect other non-genital areas. It is common in prepubertal girls and post-menopausal women.[7] Anogenital lichen sclerosus are six to ten times more common in females than males.[3] 11 patients had lichen sclerosus et atrophicus [[Figure 4], [Figure 5]] which predominantly affected females (7), which also included a thirteen year old female child. Lichen sclerosus presented as well defined depigmented patch with atrophy and telengiectasia. There was associated hypopigmented atrophic macules on the legs in a female patient. Three male patients developed complications of lichen sclerosus in the form of difficulty in retracting prepuce.
Genital psoriasis [[Figure 6]] was noted in 10 patients in this study. 9 were males presented with well-defined erythematous scaly plaques. Glans penis was the common site to be affected. 5 patients had psoriasis affecting only external genitalia.
Steatocystoma [[Figure 7]] presented as multiple discrete yellowish papules and nodules on the scrotum in 10 patients. It affected young patients more commonly similar to studies done by Karthikeyan et al, Garg et al.[1], [4]
Angiokeratoma [[Figure 8]] was seen in 3 patients presenting as skin colored to dark discrete papules on the scrotum. Angiokeratoma of Fordyce is common in late adulthood or in elderly patients.[8] Common site to be affected is scrotum. Lesions may be seen on shaft or glans penis, thighs, abdomen, and buttocks.[9] In our study it was seen in young and middle aged patients involving scrotum and shaft of the penis.
Lichen planus presented as well defined violaceous to hyperpigmented flat topped papules and plaques involving scrotum, glans and shaft of the penis. 2 patients had associated oral lichen planus in this study. In a study done by Schmidt H et al males were affected more than women. [10]
Zoon’s balanitis is an idiopathic, chronic, benign, inflammatory mucositis of genitalia that presents as solitary, shiny, well defined erythematous plaque on glans penis.[11] Zoon’s balanitis [[Figure 9]] was present in 3 patients which presented as erythematous velvety shiny plaques affecting coronal sulcus & glans penis.
Two middle aged patients had calcinosis cutis who manifested with multiple erythematous to dark colored nodules studded with white chalky deposits in the scrotum. However serum calcium was normal in both patients.
An elderly male patient presented with erosion on the external genitalia of 3 days duration associated with fever. Tzanck smear was negative. Ig M antibody for chikungunya was positive. In a study conducted in Central India, 16 male patients with chikungunya had ulcerations affecting scrotum and penis.[12]
Peyronie’s disease common in middle-aged and elderly men. It often presents as localized fibrotic disorder of tissue adjacent to the erectile tissues.[3] Our patient presented with pain in the penis of 5 year duration. On examination there was linear firm band on the dorsum of the penis. Penile Doppler study showed calcification in the mid shaft of the penis.
Pearly penile papules are physiological variants of male external genitalia which presents as multiple, tiny, flesh-colored papules on the coronal sulcus. It has to be differentiated from genital molluscum and warts.
Other non-venereal disorders noted in our study were irritant contact dermatitis, lichen nitidus, vesiculobullous disorders, cutaneous vasculitis, squamous cell carcinoma [[Figure 9]], fixed drug eruption, methotrexate induced genital ulcer, linear verrucous nevus, lymphangioma circumscriptum, Fournier’s gangrene, scrotal abscess, lichen simplex chronicus, etc.
This study reveals a wide variety of genital disorders with diverse etiology. Most of the studies done on non-venereal external genital diseases included only male patients in their studies. There are only few studies combining both males & females.
In studies conducted by Karthikeyan et al, Saraswat et al, Hogade et al, Sampath et al, vitiligo was most common genital dermatoses.[1], [4], [6], [13] Study done by Puri et al showed scrotal dermatitis and lichen sclerosus as the most common nonvenereal dermatoses affecting males and females respectively.[5] Study conducted by Nyati et al showed Tinea cruris as the most common condition. [14] Psoriasis was most common condition in a study by Geetha et al.[15] Study conducted by Nidhi et al reported lichen sclerosus as the most common genital disease. [16]
Conclusion
The disease affecting external genitalia are unique. There are variety of non- venereal conditions that can affect external genitalia, stressing the importance to identify the non –venereal causes in genital dermatoses. Since non-venereal diseases can clinically mimic sexually transmitted diseases, it is essential to differentiate the two, in order to reduce the patient’s anxiety. This study has helped in evaluating the frequency, various manifestations, and etiological factors of various nonvenereal genital dermatoses.
Source of Funding
None.
Conflict of Interest
None.
References
- K Karthikeyan, TJ Jaisankar, D Thappa. Non-venereal dermatoses in male genital region-Prevalence and pattern in a referral centre in South India. Indian J Dermatol 2001. [Google Scholar]
- B Khaitan, VK Sharma. Nonvenereal diseases of genitalia. Sexually Transmitted Diseases and AIDS 2003. [Google Scholar]
- CB Bunker, W Porter. Dermatoses of the male gentialia. Rook’s text book of Dermatology 2016. [Google Scholar]
- PK Saraswat, A Garg, D Mishra, S Garg. A study of pattern of nonvenereal genital dermatoses of male attending skin OPD at a tertiary care center. Indian J Sex Transm Dis AIDS 2014. [Google Scholar]
- N Puri, A Puri. A study of nonvenereal genital dermatoses in North India. Our Dermatol Online 2012. [Google Scholar]
- AS Hogade, S Mishra. A study of pattern of nonvenereal genital dermatoses of male attending skin OPD of tertiary centre in Kalaburagi. Int J Res Dermatol 2017. [Google Scholar]
- N Singh, DM Thappa, TJ Jaisankar, S Habeebullah. A clinical study of vulval lichen sclerosus at a tertiary care hospital in South India. Indian J Sex Transm Dis 2007. [Google Scholar]
- EM Farber, L Nall. Genital psoriasis. cutis 1992. [Google Scholar]
- M A Gonzalez - Lopez, G Consuegra, M Lacalle, M Gonzalez-Vela. Unilateral angiokeratoma of the scrotum (Fordyce’s type) associated with a contralateral varicocele. Indian J Dermatol Venereol Leprol 2017. [Google Scholar]
- H Schmidt. Frequency, duration and localization of lichen planus. A study based on 181 patients. Acta Derm Venereol 1961. [Google Scholar]
- N Kumar, V Paliwal, D Mathur. Prevalence of Non venereal genital dermatoses in male patients attending tertiary care centre in North India. Int J Med Res Health Sci 2022. [Google Scholar]
- K Mishra, V Rajawat. Chikungunya induced genital ulcers. Indian J Dermatol Venereal Leprol 2008. [Google Scholar]
- SPK Talamala, P Gummadi, G B Vatti. A Clinical Study of Patterns of Non Venereal Genital Dermatoses of Adult Males in a Tertiary Care Center. IOSR J Dent Med Sci 2016. [Google Scholar]
- A Nyati, P Agarwal. Pattern of non-venereal dermatoses of female external genitalia in Rajasthan. Asian Pac J Health Sci 2016. [Google Scholar]
- G Shinde, S Popere. A clinical study of non venereal genital dermatoses of adult in a tertiary care center. Int J Biomed Adv Res 2017. [Google Scholar]
- N Singh, DM Thappa, TJ Jaisankar, S Habeebullah. Pattern of non-venereal dermatoses of female external genitalia in South India. Dermatol Online J 2008. [Google Scholar]
How to Cite This Article
Vancouver
Shekar R, Gundappa P, L RM. Prospective hospital based study of non-venereal dermatoses of external genitalia at tertiary care institute [Internet]. IP Indian J Clin Exp Dermatol. 2025 [cited 2025 Sep 11];11(1):109-113. Available from: https://doi.org/10.18231/j.ijced.2025.016
APA
Shekar, R., Gundappa, P., L, R. M. (2025). Prospective hospital based study of non-venereal dermatoses of external genitalia at tertiary care institute. IP Indian J Clin Exp Dermatol, 11(1), 109-113. https://doi.org/10.18231/j.ijced.2025.016
MLA
Shekar, Rachana, Gundappa, Pavithra, L, Ranjitha M. "Prospective hospital based study of non-venereal dermatoses of external genitalia at tertiary care institute." IP Indian J Clin Exp Dermatol, vol. 11, no. 1, 2025, pp. 109-113. https://doi.org/10.18231/j.ijced.2025.016
Chicago
Shekar, R., Gundappa, P., L, R. M.. "Prospective hospital based study of non-venereal dermatoses of external genitalia at tertiary care institute." IP Indian J Clin Exp Dermatol 11, no. 1 (2025): 109-113. https://doi.org/10.18231/j.ijced.2025.016
