- Received November 30, -0001
- Accepted November 30, -0001
- Publication October 03, 2020
- Visibility 10 Views
- Downloads 1 Downloads
- DOI 10.18231/j.ijced.2020.053
-
CrossMark
- Citation
Dermoscopy in viral infections: An observational study
- Author Details:
-
K M. Sudhakar Rao
-
Sakshi S. Gaikwad *
Introduction
Various virus infections can be easily diagnosed and treated. Some cases can be atypical in presentation, making it difficult to proceed to diagnosis. Many of the infections when present in immunocompromised state can be difficult to diagnose because of its atypical presentation. Sometimes they can present with other dermatological condition, overlapping each-others clinical features. Thus, clinical diagnosis can be challenging. There can be delay in the diagnosis and treatment. Even the skin type (dark skin type) can contribute for such delay.
Histopathology is the gold standard for the diagnosis, but it is an invasive cumbersome and time consuming process. Whereas, dermoscopy is accurate non-invasive, easier, technique which can be used for diagnosis within a short period.[1] Dermoscopy is very useful auxiliary tool. It helps in diagnosing different dermatological condition by magnifying both surface and sub-surface features, which are not appreciated by unaided eye. [2] In this report, we sought to provide various dermoscopic features in various viral infection which may assist in clinical diagnosis.
Objective
To evaluate dermoscopic patterns in viral infections.
Materials and Methods
The ethical clearance for the study was obtained by the Institutional Ethical Committee. Written informed consent was taken from the patients.
This study was carried out on 106 patients, out of which 85 were men and 21 were female attending the department of dermatology in a tertiary care hospital. Ages of the patients were between 6 years to 80 years. It was an observational study and patients were selected randomly. Handheld contact dermoscope, Derm Lite 4 was employed in the study. A smart phone was attached to the dermoscope to save images.
Results
The study enrolled 106 patients, out of which 85 (80.20%) were men and 21(19.80%) were female. Ages ranged from 6 to 80 years. 48(45.28%) out of them had viral warts, 9(8.49%) had Molluscum contagiosum (MC) and 15(14.15%) had Pityriasis rosea (PR), 10(9.43%) had herpes labialis, 10(9.43%) had herpes zoster, 8(7.54%) had varicella, 5(4.71%) had hand foot mouth disease and 1 (0.94%) had Orf nodule.
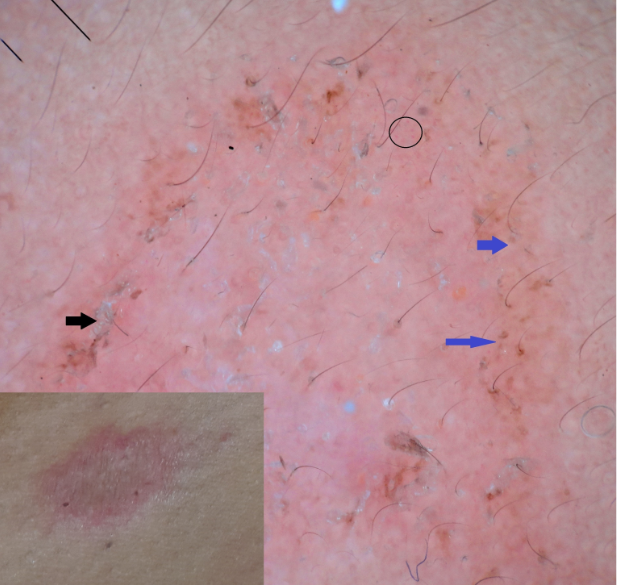
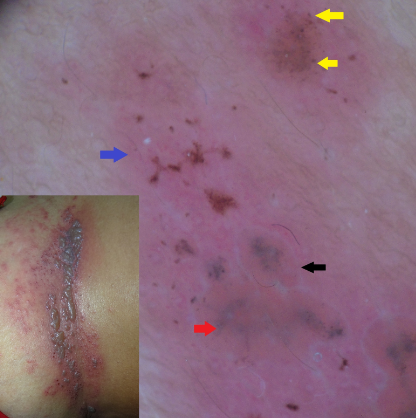
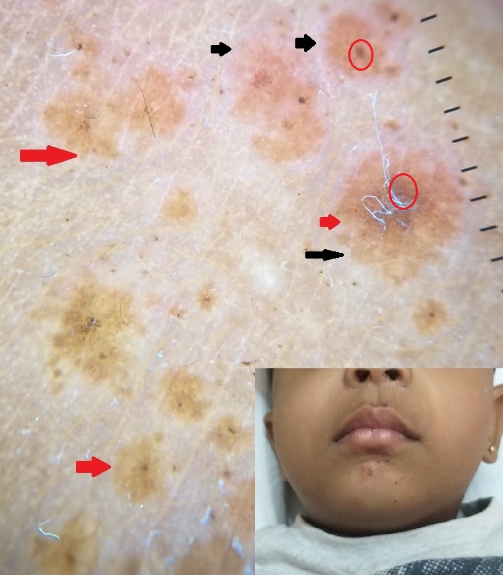
PR on dermoscopy had brown dots and red dots. All (100%) the cases had peripheral scaling, 3(20%) had brownish yellowish background and 12(80%) had light pink background. ([Figure 1])
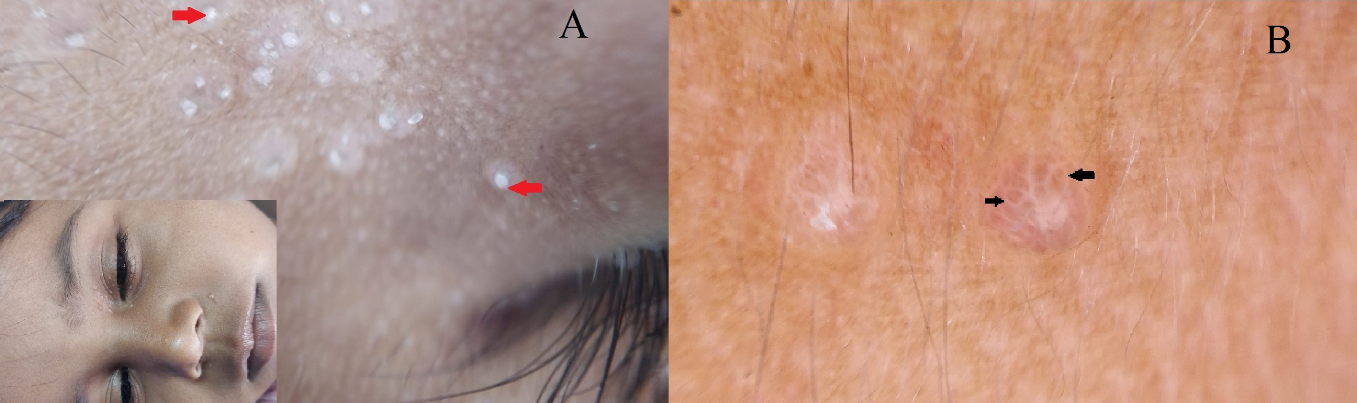
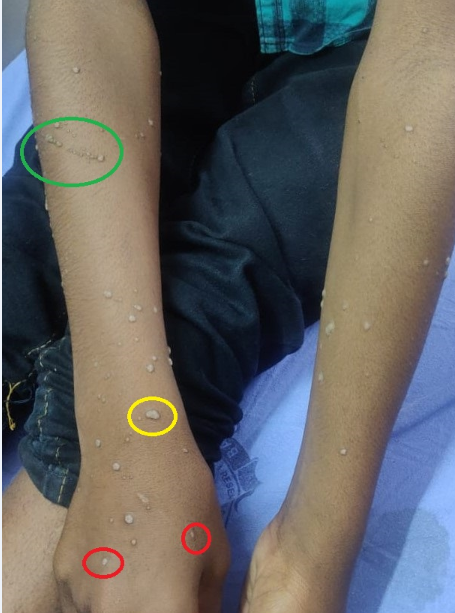
9 patients presented with MC. On dermoscopy all (100%) showed white amorphous structure. 4(44.45%) of them had erosion, 1(11.12%) of them had central umbilication, 4(44.45%) of them showed poly-lobulated structure and 1(11.12%) patient had 4-leaf -clover – like appearance. ([Figure 2])
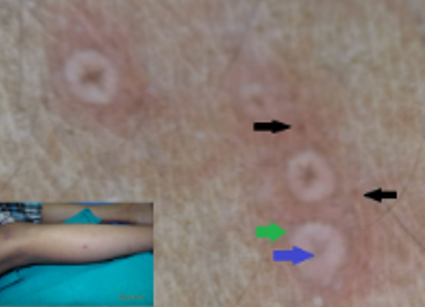
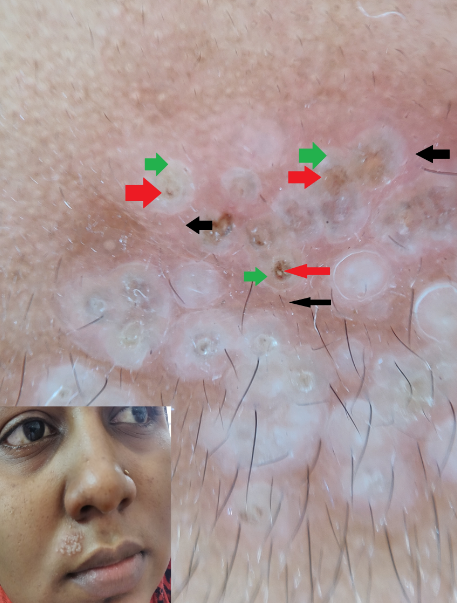
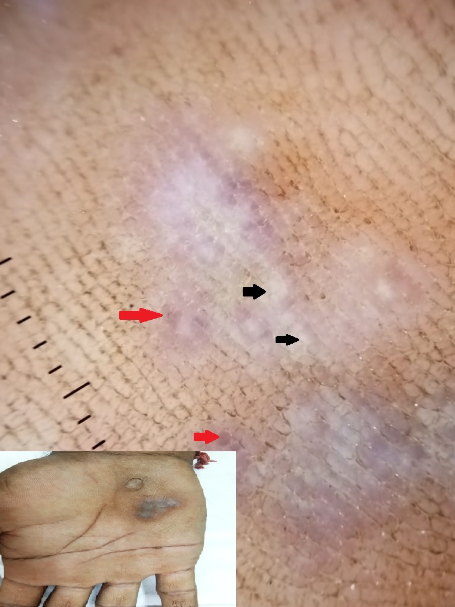
On dermoscopy all chicken pox cases (100%) showed erythematous background and brown dots. Two (25%) had erosions and 2 (25%) showed central umbilication. ([Figure 3])
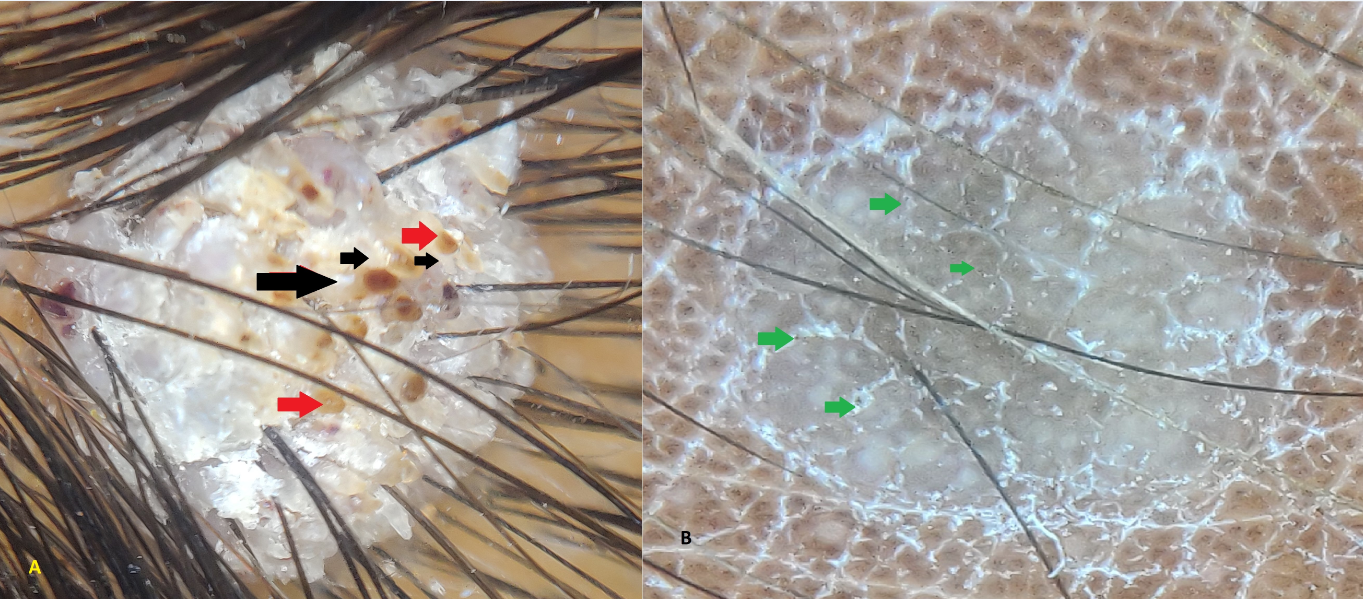
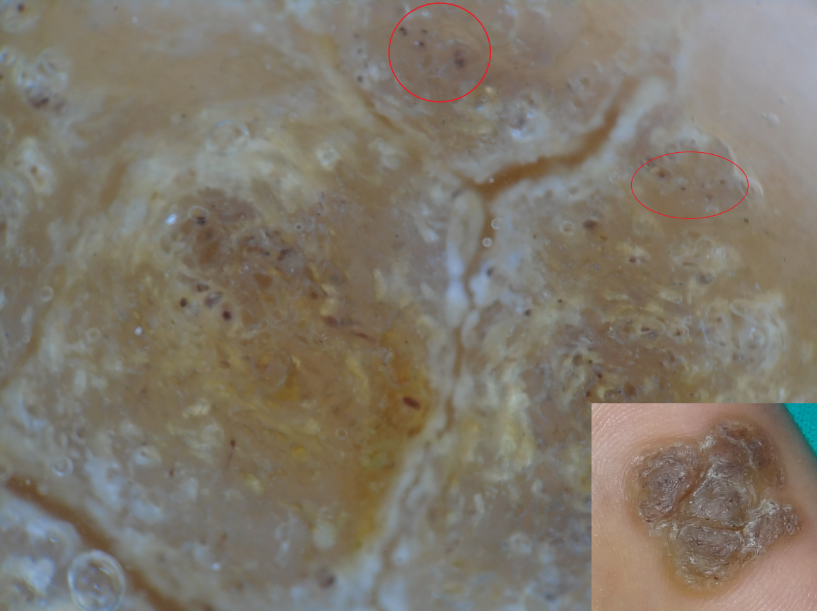
Among 48 patients with warts, 5(10.41%) had plane wart, 29 (60.41%) had common wart, 3(6.25%) had periungual wart, 8 (16.67%) had plantar wart, 2 (4.16%) had filiform wart and 1 (2.08%) patient had genital wart. All of them on dermoscopy showed red to blackish red. In addition, common wart had tadpole like structure. Filiform wart had finger-like projections, hairpin vessel and white halo. Genital wart showed knob like structure, hair pin like vessels and mosaic pattern (figure 4,5,6,7,8[Figure 4], [Figure 5], [Figure 6], [Figure 7], [Figure 8] )
Dermoscopic features of herpes labialis had 3 zones, central brown pigmentation, surrounded by white colour and peripheral Erythema in 8 (80%) patients. In 2 (20%) patients we noticed erythematous background, erosions and brown dots. (figure 9)
Dermoscopically all the cases of herpes zoster had erythematous background (100%), 8 (80%) had poly-globular white structure, brown dots were present in 3 (30%) patients, 2 (20%) had erosions and centrally placed grey dots in 3(30%) patients. ([Figure 10])
Dermoscopy of hand foot mouth disease lesion showed yellowish/brown background, brown dots, brown globules and whitish hue in 3(60%) patients. 2 (40%) showed crusting and yellowish/brown pigmentation. ([Figure 11])
Orf nodule on dermoscopy showed bluish area and central whitish areas. ([Figure 12])
Tzanck smear from herpes patients showed multinucleated giant cell and acantholytic cell. Orf nodule showed acantholytic cell.(Figure 13 )



| Type of infection | N | Dermoscopic findings |
| Plane wart | 05 | Brown to Blackish red dots |
| Common wart | 29 | Grouped red dots with white halo |
| Periungual wart | 03 | presence of black dots |
| Plantar wart | 08 | presence of black dots |
| Filiform wart | 01 | Finger like projection |
| Filiform wart | 02 | Finger like projection, hairpin vessel with white |
| Genital wart | 01 | Knob like structure, hairpin vessel, mosaic pattern |
| Molluscumcontagiosum (9) | 4 | Erosion, whitish structure |
| 1 | Central umbilication, whitish structure, 4-leaf-clover-like appearance | |
| 4 | Whitish structure, polylobular structure | |
| Pityriasisrosea (15) | 3 | Brown dots, red dots, peripheral scaling and light pink background |
| 1 | Brown dots, red dots, diffuse white scaling, and yellowish background | |
| 1 | Brown dots, red dots, peripheral scaling, and yellowish background | |
| 1 | Brown dots, red dots and yellowish background | |
| 2 | Brown dots, red dots and light pink background | |
| 7 | Brown dots, red dots, diffuse white scaling, and light pink background | |
| Chicken pox(8) | 4 | Erythematous background, brown dots, |
| 2 | Erythematous background, brown dots, erosion | |
| 2 | Erythematous background, brown dots, umbilication | |
| Herpes zoster(10) | 3 | Polylobular white structure. erythematous background, brown dots, grey to black centrally placed dots |
| 2 | Erosion, erythematous background | |
| 5 | Erythematous background, brown dots, polylobular white structure | |
| Herpes labialis(10) | 8 | 3 zones, central brown pigmentation, surrounding white colour and peripheral erythema |
| 2 | Erythematous background, erosions, brown dots | |
| Hand foot mouth disease(5) | 3 | Yellowish /brown background, brown dots, globules and whitish hue. |
| 2 | Crusting, erythematous background | |
| Orf nodule | 1 | bluish globules, whitish area |



Discussion
Pityriasis rosea (PR)
In our study most common background was light pink (80%), as compared to study (65%) which was yellow. [3] The reason can be due to darker skin type in our study. In a study,[3] 50% of the background was dull red in colour as compared to our study which was light pink (80%). Similarly, in another study[4] 40 % background colour was dull red as compared to our study which was light pink (80%) colour. The reason can be due to darker skin type in our study. We observed brown dots, globules and red dots in 100% patients, similar to other studies.[4], [5] Peripheral white scaling present in 12 (80%) patients. Lallas et al described peripheral scaling in 80%of patients. Scaling represent hyperkeratosis while the red dots represent vascular pattern histologically.[4], [5] Pityriasis rosea is very common dermatological condition caused by HHV6 and HHV 7.[6]
Molluscum contagiosum
In our study all the patients had whitish structure. (44.45%)patients had erosion and poly lobulated structure (44.45%). Central umbilication was seen in only 11.12 % patients. Polylobulated structure was seen in all cases in the study,[7] while in our study it was 40% of patients. Polylobular structure is due to lobular hyperplasia. As mentioned in the literature,[8] vascular structure like crown (72.34), radial (54.25), dotted vessels (20.21%) and flower pattern (19.68) were not noticed in our study, due to skin typeIV. Our study also showed 4-leaf-clover-like appearance similar to Piccolo V.[9] According to him young lesions showed 4-leaf -clover – like appearance. Similar structure was seen in the study,[10] due to optical effect by horny material. Ianhez M et al described yellowish material at the centre of lesion.[8] but our study showed whitish structure.
Chicken pox
Dermoscopically there was presence of erythematous background (100%), brown dots (100%), central erosion (25%) and vesicles presented with well-defined to ill-defined border. Similar findings were seen in the study. [7] With erythematous background and brown dots in 100% of the patients. In addition, we were also able to appreciate central umbilication (25%). Brown dots represent multinucleated giant cell. [7] But due to lack of literature on dermoscopy of chicken pox, we could not compare our study.
Wart
On dermoscopy all types of common warts show brown to blackish dots, which represent vascular pattern. We appreciated grouped red dots with white halo. These were mentioned as tadpole like structures in the study. [7] There was presence of black dots in plantar and periungual wart. We also observed finger like projection in filiform wart similar to described in the study. [7] These finger like projections were described as more pronounced papillae than that one seen in common wart in the literature.[9] In our patient with filiform wart we observed hairpin vessel with white halo. Knob like structure and hairpin like vessels were seen in genital wart.[11], [12] As compared to the study,[13] mosaic pattern (grouped dotted vessels in centre surrounded by whitish network) was similar to our study. There was presence of tiny small brown to blackish red dots in plane warts in our study. Similarly, red dots in light brown background were described by Papakonstantinou E.[14]
Herpes labialis
It is caused by herpes simplex virus-1.[15] In a study,[7] dermoscopy showed erythematous background and brown dots in all the patients. We noticed 3 zones, central brown pigmentation, surrounded by white colour representing ballooning degeneration and peripheral erythema in 80% patients. 20% patients showed erythematous background, erosions and brown dots. Due to lack of literature on dermoscopy of Herpes labialis, we could not compare with other studies.
Herpes zoster
According to the literature,[7] herpes zoster showed multiple confluent round cloudy white polyglobular structures. Similarly, we were able to appreciate it in 80% of our patients. Central brown dots (53%) as present in their study,[7] were also seen in our study (80%). We were also able to appreciate erythematous background in 100 % of our patients. There was also presence of grey to black centrally placed dots (30%) in our study which was not described in the study.[7]
In a study,[16] dermoscopy showed erythematous area and dilated vessels. These patterns were not similar to our study, due to early presentation of herpes zoster.
Our findings of herpes and the ones mentioned in literature were similar. But, again due to inadequate dermoscopic studies on herpes infection, we were unable to compare our findings.
Hand foot mouth disease
Hand foot mouth disease, very common in children, caused by Coxsackievirus. [17] Dermoscopy shows yellowish/brown pigmentation in all the patients. Brown dots, globules present in 60%, crusting in 40 % and whitish hue. Due to lack of literature, we could not compare with other studies.
Orf nodule
According to the study, [18] dermoscopy of orf nodule showed yellow white ring, crust, greyish white streak and yellow white area. Vascular structures like erythema, dot vessels, glomerular vessels, and milky red globule were noticed. Similarly, our study shows bluish globules and whitish area. No vascular structures were appreciated in our study. As we had only one case, various dermoscopic features of Orf nodule was unable to study. Due to paucity of article we could not compare our study with other article.
Conclusion
Clinically similar conditions can be distinguished with the help of dermoscopy. It can help to proceed to diagnosis within short time, in case of atypical presentation. It is gaining wide spread importance in realm of dermatology.
Source of Funding
None.
Conflict of Interest
None.
References
- H Kittler, H Pehamberger, K Wolff, M Binder. Diagnostic accuracy of dermoscopy. Lancet Oncol 2002. [Google Scholar]
- E Errichetti, G Stinco. Dermoscopy in General Dermatology: A Practical Overview. Dermatol Ther 2016. [Google Scholar]
- M Nwako-Mohamadi, J Masenga, D Mavura, O Jahanpour, E Mbwilo, A Blum. Dermoscopic features of psoriasis, lichen planus, and pityriasis rosea in patients with skin type IV and darker attending the Regional Dermatology Training Centre in Northern Tanzania. Dermatol Pract Concept 2019. [Google Scholar]
- A. Lallas, A. Kyrgidis, T.G. Tzellos, Z. Apalla, E. Karakyriou, A. Karatolias. Accuracy of dermoscopic criteria for the diagnosis of psoriasis, dermatitis, lichen planus and pityriasis rosea. Br J Dermatol 2012. [Google Scholar]
- Ö F Elmas, A Kilitçi, E M Acar. Dermoscopic profile of pityriasis rosea. Dermatol Sin 2019. [Google Scholar]
- V Relhan, K Mahajan, A K Relhan, V K Garg. Pityriasis rosea: An update on etiopathogenesis and management of difficult aspects. Indian J Dermatol 2016. [Google Scholar]
- H H Mehta, S S Nayak, P C Gajjar, V N Nimbark. Dermoscopy of general dermatological conditions in Indian population: A descriptive study. Clin Dermatol Rev 2017. [Google Scholar]
- M Ianhez, S C Cestari, M Y Enokihara. Seize MB Dermoscopic patterns of molluscum contagiosum: a study of 211 lesions confirmed by histopathology. An Bras Dermatol 2011. [Google Scholar]
- V Piccola. Updates on dermoscopy and infectious skin diseases. Dermatol Pract Concept 2020. [Google Scholar]
- G Badavanis, E Pasmatzi, A Monastirli, S Georgiou, D Tsambaos. Topical Imiquimod is an Effective and safe Drug for molluscum contagiosum in Children. Acta Dermatol Venerol Croat 2017. [Google Scholar]
- M Ianhez, C Cestarisda, M Y Enokihara, M B Seize. Dermoscopic patterns of molluscum contagiosum: a study of 211 lesions confirmed by histopathology. An Bras Deramtol . [Google Scholar]
- R Meza-Romero, C Navarrete-Dechent, C Downey. Molluscum contagiosum: an update and review of new perspective in etiology, diagnosis, and treatment. Clin, Cosmetic Investig Dermatol 2019. [Google Scholar]
- P Tschandl, G Argenziano, R Bakos, G Jean-Yves, R Hofmann-Wellenhof, H Kittler. Dermoscopy and entomology (entomodermoscopy). J der Deutschen Dermatologischen Gesellschaft 2009. [Google Scholar]
- E Papakonstantinou, U Raap. Alternative uses of dermoscopy in general dermatology. J Surg Dermatol 2017. [Google Scholar]
- G W Raborn, Mga Grace. Recurrent Herpes Simplex Labialis: Selected Therapeutic Options. J Can Assoc 2003. [Google Scholar]
- F Lacarrubba, A E Verzì, M L Musumeci, G Micali. Early diagnosis of herpes zoster by handheld reflectance confocal microscopy. J Am Acad Dermatol 2015. [Google Scholar]
- K B Kumar, A G Kiran, B U Kumar. Hand foot and mouth disease in children: A clinic epidemiological study. Indian J Paediatr Dematol 2016. [Google Scholar]
- E Ayhan, H Aktas. Dermoscopic features and types of Orf and milkrs nodule. Postepy Dermatol Alergol 2017. [Google Scholar]
