- Visibility 371 Views
- Downloads 36 Downloads
- Permissions
- DOI 10.18231/j.ijced.2025.010
-
CrossMark
- Citation
Clinico observational dermatoscopic study of facial melanosis in a semiurban tertiary hospital in central Bihar
Abstract
Introduction: Disorders of hyperpigmentation especially with facial involvement can result in tremendous psycho-social impact and are associated with poor quality of life. Mostly diagnosis is based clinically; the role of histopathology is limited by its invasive nature and reluctance on part of patient to undergo facial biopsy as well. Dermatoscopy is a non-invasive, handy tool, which is increasingly being used in diagnosis and prognostication of pigmentary dermatoses.
Materials and Methods: A clinico-observational dermatoscopic study of various facial hyperpigmentary disorders was carried out and their clinical profile were compared. 105 patients attending our Outpatient department were enrolled between Jan 2020 to March 2021 with their informed written consent. Dermlite Dl4w in polarised mode was used. Clinical history was elicited and noted.
Results: Female patients outnumbered male overall. Melasma was highest followed by post inflammatory hyperpigmentation among all cases. In our study, we found reticuloglobular followed by annular pattern to be most common dermatoscopic findings.
Conclusion: Dermatoscopy is important tool for differentiating various facial melanosis.It can be helpful in differentiating benign from malignant condition and melanocytic from non-melanocytic lesions. Prognosis can be explained and adverse effects of therapy can be easily monitored and prevented. Best available therapy can be planned accordingly.
Introduction
Disorders of hyperpigmentation are very common. These can be melanocytic and non-melanocytic. Pigmentary disorders involving face can really take toll on patients pscho-social well-being often leading to lower quality of life. Some of the causes of Facial melanoses include Melasma, Lichen Planus Pigmentosus, Post inflammatory hyperpigmentation, Riehl’s melanosis(pigmented contact dermatitis), Erythema dyschromicum perstans (EDP), Erythrosis, Pigmentary demarcation lines and Poikiloderma of Civatte. But there is considerable overlap in features amongst the clinical entities.[1]
These are primarily diagnosed through clinical evaluation, as the role of histopathology is limited by its invasive nature and patients' reluctance to undergo facial biopsies. Dermatoscopy has gained prominence due to its noninvasive nature. Dermatoscopy offers several advantages, as clinicians can conduct examinations over the entire affected area, perform repeated assessments throughout the course of the disease, and modify or confirm diagnoses as needed. Very few published literature is available where dermatoscope has been employed to study facial melanoses. [1]
Approximately 10.8% of adult patients attending dermatology outpatient departments (OPD) in Western India present with disorders of pigmentation. [2]
This study aims to find the utility of dermatoscopy in the routine diagnosis of FM of patients attending our OPD.
Materials and Methods
A cross sectional study was done at Department of Dermatology in Semi-urban tertiary hospital in central Bihar after approval from Ethical Committee. It was done from Jan 2020 to March 2021. One hundred and five patients were included after taking informed written consent. This is a urban tertiary care hospital that caters both urban and rural population of Bihar.
Inclusion criteria
Patients >18yrs or above of age in both sexes.
Patients who were willing to participate in study were enrolled.
Exclusion criteria
Patients who had taken treatment in the last 1 month.
Pregnant and lactating women.
Patients with active infection on face.
Overlapping two or more facial melanosis.
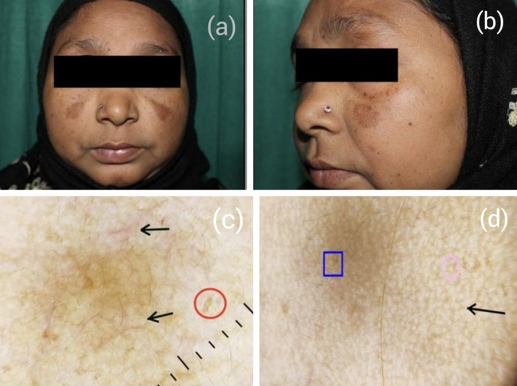
A detailed history including use of prescription drugs, significant medical history was elicited. Clinical examination of each patient was done. Dermoscopic examination of the lesion was done using Dermlite DL4w. Photographs were taken using One Plus 8T smartphone (dermoscopic) and clinical picture (DSLR Canon 1300D)([Figure 1]).
Results
Total eighteen thousand six hundred and twenty six patients attended our OPD during our study period (Jan 2020 to march 2021). Among them nine hundred sixty patients were found who had Facial Melanosis. We chose first hundred and five patients who fulfilled our selection criteria.
In this study female outnumbered male. Out of 105 patients, 70 (66%) were females and 35 (34%) were male. They were further divided into three age groups -18-20 yrs, 21-40 yrs & 41-60 yrs. 21-40 years age group consisted maximum 78 patients among them 28(35.8%) were male & 50(64.2%) were female. Among these, 12 patients who belonged to 18-20yr age group, 3(25%) were male & 9(75%) were female. 41-60 years age group consisted of 15 patients; 5(33.3%) were male and 10(63.7%) were female patients.
Maximum patients 65 (62%) were affected in the Malar area. 35 (33%) patients were affected with Centrofacial area. Centro facial with Mandibular area affected in 4 patient and Mandibular area was affected in 1 patient.
|
Duration of disease |
No of patients (n=105) |
Percentage |
|
<1yr |
27 |
25.7 |
|
1-<5yr |
63 |
60 |
|
5-10yr |
10 |
9.5 |
|
>10yr |
05 |
4.8 |
In our study, maximum patients had duration of melanoses for 1yr-<5yr i.e 63(60%) followed by less than a year 27(25.7%).([Table 1])
|
Facial melanoses |
No of patients (n=105) |
Percentage |
|
Melasma |
73 |
69.5 |
|
Nevus of ota |
05 |
4.8 |
|
Lichen planus pigmentosus |
04 |
3.8 |
|
Exogenous ochronosis |
01 |
0.9 |
|
Freckles and ephelides |
5 |
4.8 |
|
Postinflammatory hyperpigmentation |
12 |
11.4 |
|
Pigmented contact dermatitis |
05 |
4.8 |
Melasma was most common facial melanoses (69.5%) followed by post inflammatory hyperpigmentation (11.4%). Nevus of Ota, LPP, PCD all being at 4.8% while exogenous ochronosis being least common (0.9%).([Table 2])
|
Condition |
Type |
Dermoscopic findings |
Number of patients (%) |
|
Melasma |
1.Epidermal (n=23) |
a. Reticuloglobular pattern (RGP) |
23(100%) |
|
|
|
b. Granular pattern(GP) |
14(60.7%) |
|
|
|
c. Annular pattern(AP) |
9(39.1%) |
|
|
|
d. Arcuate pattern(AC) |
5(21.7%) |
|
|
|
e. Perifollicular dark brown globules & granules(PFDBGG) |
15(65.2%) |
|
|
2. Dermal (n=21) |
a. Reticuloglobular pattern(RGP) |
12(57.1%) |
|
|
|
b. Annular pattern(AP) |
10(47.6%) |
|
|
|
c. Arcuate pattern(AC) |
9(42.9%) |
|
|
|
d. Perifollicular dark brown globules & granules(PFDBGG) |
16(76.2%) |
|
|
|
e. Pseudoreticular honeycomb pattern(PRHP) |
6(28.6%) |
|
|
3.Mixed (n=29) |
a. Reticuloglobular pattern(RGP) |
26(89.7%) |
|
|
|
b. Granular pattern(GP) |
1(3.4%) |
|
|
|
c. Annular pattern(AP) |
24(82.8%) |
|
|
|
d. Arcuate pattern(AC) |
16(55.2%) |
|
|
|
e. Perifollicular dark brown globules & granules(PFDBGG) |
27(93.1%) |
|
|
|
e. Psuedoreticular honeycomb pattern(PRHP) |
4(13.8%) |
In our study out of 73 melasma patients, mixed pattern was most common i.e 29 (39.7%) followed by epidermal i.e 23 (31.5% ) followed by dermal 21(28.8%).([Table 3])
Dermatoscopic findings in total 23 patients of Epidermal Melasma ([Figure 2]), 100% (23) were RGP pattern which was highest followed by PFDBGG pattern 65.2% (15). Dermatoscopic pattern of 29 patients of mixed melasma ([Figure 3]) PFDGG 27 (93.1%) pattern was highest, second highest RPG pattern 26 (89.7%). Dermatoscopic pattern of 21 patients of dermal melasma, PFDBGG 16 (76.2%) pattern was highest followed by RPG pattern 12(57.1%).
|
Disease |
Dermoscopic findings |
Number of patients (%) |
|
Post inflammatory hyperpigmentation (PIH) n=12 |
A. Granular Pattern(GP)/brown dots and granules |
7(58.3%) |
|
|
B. Pseudoreticular Honeycomb Pattern(PRHP) |
12(100%) |
|
|
C. Brown black structureless areas |
2(16.6%) |
|
Pigmented contact dermatitis (n=5) |
A. Pseudonetwork with non-pigmented follicular openings |
5(100%) |
|
|
B. Fine Pigment Granules with perifollicular whitish halo |
3(60%) |
|
Nevus of Ota (n=5) |
A. Bluish Black Blotches And Structreless Areas |
5(100%)5 |
|
|
B. Reticuloglobular Pattern |
5(100%) |
|
Lichen planus pigmentosus (n=4) |
A. Perifollicular Dark Brown Globules And Granules(PFDBGG) |
1(25%) |
|
|
B. Bluish Black Granules |
2(50%) |
|
|
C. Hem Like Pattern |
2(50%) |
|
|
D. Reticuloglobular Pattern |
4(100%) |
|
|
E. Exaggerated Pseudoreticular Network |
3(75%) |
|
Facial exogenous oochronosis (n=1) |
A. Irregular Grey Brown, Globular, Annular And Arciform Structures |
1(100%) |
|
|
B. Diffuse Brown Background With White Dots |
1(100%) |
|
|
C. Curvilinear And Worm Like Structures |
1(100%) |
|
Freckles and Lentigines (n=5) |
A. Uniform Pigmentation With Moth Eaten Edge |
5(100%) |
|
|
B. Uniform Dark Brown Pigmentation |
5(100%) |
Second most common melanoses was Post Inflammatory Hyperpigmentation 12(11.4%). On dermoscopy ([Figure 4]), PRHP pattern was seen highest 12 (100%) followed by GP Pattern 7 (58.33%).([Table 4])
A total of 5 cases of Nevus Of Ota ([Figure 5]), Pigmented Contact Dermatitis ([Figure 6]) & Freckles And Lentigines ([Figure 7]) were studied. The most common dermatoscopic patterns were bluish black blotches and structureless areas, reticular pattern, and uniform pigmentation with moth eaten edges respectively in these cases.
Other hypermelanotic conditions seen in the minority include Lichen planus pigmentosus ([Figure 8]) and Facial exogenous oochronosis ([Figure 9]).

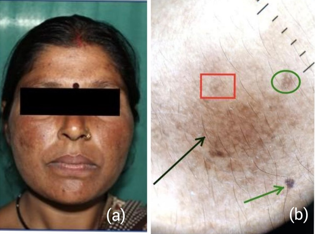
Green arrow: Jelly sign (denser distribution of granules around follicles); Red box: Dots and globules, sparing follicular and adnexal opening; Green box: Epidermal pigment.






Discussion
Our face plays a critical role in physical attractiveness. Unlike most internal illnesses, skin diseases especially those on face are often immediately visible to others and, therefore, may lead to significant psychosocial consequences and consequent dermatological consultations, thus explaining the growing importance of these disorders. [3]
Facial melanoses (FM) are a common presentation in Indian patients, causing cosmetic disfigurement with considerable psychological impact. These disorders are mainly diagnosed by thorough clinical examination since facial biopsy can be invasive, and many patients are unwilling to go for it. It is crucial to differentiate between benign and malignant conditions to give prompt and accurate treatment. [4]
Dermatoscopy, a relatively recent advancement in diagnostic technology, has gained prominence due to its non-invasive characteristics and the ability to conduct repeated examinations over period of time.
While dermoscopy cannot replace a clinical history and examination or histopathological analysis, it offers significant advantages in the diagnosis of various hyperpigmentation disorders.[5]
Additionally, individuals with darker skin are particularly vulnerable to pigmentary disorders, largely due to the contrast created by the absence of pigment and their predisposition to developing post-inflammatory hyperpigmentation.[6]
Female predominance seen in our study 66% which was comparable with study by Patel et al[7] (63.3%) and Hassan et al[8] (65.8%).
This was seen probably due to hormonal influence and females being more conscious about their appearance in comparison to males.
In our study the most common site of disease was malar 63(63%) followed by centro facial 35(35%).
In our study, the most common age group affected was 21 to 40 years in 74% cases, which was higher to Hassan et al.[8] and Patel et al[7] study in which the most common age group was 21 to 40 years (56.73%) and 19-40years (55%) respectively.
The most common dermatoscopic pattern seen in our study was reticuloglobular 65% (69) followed by annular pattern 40.9%(43). The reticuloglobular pattern was identified as the most common dermoscopic pattern in studies by Nanjundaswamy et al[9] 35%(7), Kaur et al[10] 81%(9) and Yalamanchili et al [11] 95%(10).
Melasma was reported as the most common cause of melanosis consisting of 69.5% cases. This is much higher than that reported by Hassan et al [8] with 35% and Patel et al [7] with 39%.
Melasma is particularly common among individuals of Asian and Hispanic descent, as well as those with Fitzpatrick skin types 4 to 6.[9] This condition often affects people who are frequently exposed to intense ultraviolet light.[12]
In our study of 73 melasma patients, the mixed pattern was the most prevalent, observed in 29 patients (39.7%). This was followed by the epidermal pattern, seen in 23 patients (31.5%), and the dermal pattern, which was present in 21 patients (28.8%). Melasma usually presents as a reticular pigment network, often with perifollicular sparing. The pigmentation can range from light to dark brown.[13]
Second most common melanoses was Post Inflammatory Hyperpigmentation 12(11.4%) similar to Patel et al[7] with 10% and Hassan et al [8] with 16.34% cases.
Most common etiology was secondary to acne vulgaris. This was similar to a study by Hassan et al and Taylor et al. [14] On dermoscopy, PRHP pattern was seen highest 12 (100%) followed by GP Pattern 7 (58.33%).
Lichen planus pigmentosus, a rare variant of lichen planus, constituted 3.8% of patients in our study.Females outnumbered males by 80% of the cases which was similar to Vega et al., who also reported female preponderance [15] Bhutani et al. observed no difference in sex distribution in their patients. [16] Pigmentation in different patients varied from slate gray to brownish-black but was diffuse in the majority.
In patients with freckles and lentigines, the exclusive dermoscopic findings were uniform pigmentation with a moth-eaten edge, along with a dark brown, uniform network.
Limitation
Histopathological correlation was not done.
Conclusion
In our study of 105 patients, melasma was most common facial melanoses. Most common dermatoscopic finding was reticuloglobular pattern. Our study offers valuable insights into the dermatoscopic findings of various hyperpigmented lesions, enhancing clinical practice. It helps bridge the gap between confirmatory biopsy results and clinical observations. Routine use of a dermatoscope can improve accuracy in assessing hyperpigmented skin lesions, potentially reducing the need for invasive biopsies.
Source of Funding
None.
Conflict of Interest
None.
References
- Kanna N, Rasool S. Facial melanoses:Indian perspective. Indian J DermatolVenereol Leprol. 2011;77(5):552-63. [Google Scholar]
- Sayal S, Das A, Gupta C. Pattern of skin diseases among civil population and armed forces personnel at Pune. Indian J Dermatol Venereol Leprol. 1997;63(1):29-32. [Google Scholar]
- Hassan I, Bhat Y, Aleem S, Anwar P. AClinico-epidemological study of facial melanosis. Pigment. 2015;2(1). [Google Scholar] [Crossref]
- Kaliyadan F. The scope of the dermoscope. Indian Dermatol Online J. 2016;7(5):359-63. [Google Scholar]
- Oza R, Agrwal S, Tank J, Sutaria A, Parmar K, Shah B. Role of dermoscopy in hyperpigmented skin disorders: A tertiary care centre experience. IP Indian J Clin Exp Dermatol. 2023;9(4):184-93. [Google Scholar]
- Sandhu S, Shekhar N, Radhakrishnan S. Dermoscopy of disorders of hyperpigmentation. Pigment Int. 2021;8(1):14-24. [Google Scholar]
- Patel D, Tandel J, Rutoo P, Ganjiwale J, Nair P. Clinico-dermatoscopic study of facial melanosis at a tertiary care hospital. Pigment Int. 2022;9(2):115-21. [Google Scholar]
- Iffat H, Samia A, Bhat Y, Parvaiz A. A clinico-epidemiological study of facial melanosis. Pigment Int. 2015;2(1):34-40. [Google Scholar]
- Nanjundaswamy B, Joseph J, Raghavendra K. A clinico dermoscopic study of melasma in a tertiary care center. Pigment Int. 2017;4(2):98-103. [Google Scholar]
- Kaur S, Kaur J, Sharma S, Sharma M, Mahajan A, Singh A. A clinico-dermatoscopic study of 100 cases of melasma in a tertiary care hospital. Int J Res Dermatol. 2018;4(1):41-5. [Google Scholar]
- RY, Shastry V, JB. Clinico-epidemiological Study and Quality of Life Assessment in Melasma. Indian J Dermatol. 2015;60(5). [Google Scholar] [Crossref]
- Wu I, Lambert C, Lotti T, Hercogová J, Sintim-Damoa A, Schwartz R. Melasma. G Ital Dermatol Venereol. 2012;147(4):413-8. [Google Scholar]
- Gupta T, Sarkar R. Dermoscopy in Melasma − Is it Useful?. Pigment Int. 2017;4(2). [Google Scholar] [Crossref]
- Taylor S, Grimes P, Lim J, Im S, Lui H. Postinflammatory hyperpigmentation. J Cutan Med Surg. 2009;13(4):183-91. [Google Scholar]
- Vega ME, Waxtein L, Arenas R, Hojyo T, Dominguez-Soto L. Ashy dermatosis and lichen planus pigmentosus: a clinicopathologic study of 31 cases. Int J Dermatol. 1992;31(2):90-4. [Google Scholar]
- Bhutani L, Bedi T, Pandhi R, Nayak N. Lichen planus pigmentosus. Dermatologica. 1974;149(1):43-50. [Google Scholar]
How to Cite This Article
Vancouver
Hassan A, Singh A, Anjula , Singh R, Kumar S, Shankar V. Clinico observational dermatoscopic study of facial melanosis in a semiurban tertiary hospital in central Bihar [Internet]. IP Indian J Clin Exp Dermatol. 2025 [cited 2025 Sep 29];11(1):67-72. Available from: https://doi.org/10.18231/j.ijced.2025.010
APA
Hassan, A., Singh, A., Anjula, , Singh, R., Kumar, S., Shankar, V. (2025). Clinico observational dermatoscopic study of facial melanosis in a semiurban tertiary hospital in central Bihar. IP Indian J Clin Exp Dermatol, 11(1), 67-72. https://doi.org/10.18231/j.ijced.2025.010
MLA
Hassan, Asna, Singh, Abhilasha, Anjula, , Singh, Ramawatar, Kumar, Subodh, Shankar, Vikas. "Clinico observational dermatoscopic study of facial melanosis in a semiurban tertiary hospital in central Bihar." IP Indian J Clin Exp Dermatol, vol. 11, no. 1, 2025, pp. 67-72. https://doi.org/10.18231/j.ijced.2025.010
Chicago
Hassan, A., Singh, A., Anjula, , Singh, R., Kumar, S., Shankar, V.. "Clinico observational dermatoscopic study of facial melanosis in a semiurban tertiary hospital in central Bihar." IP Indian J Clin Exp Dermatol 11, no. 1 (2025): 67-72. https://doi.org/10.18231/j.ijced.2025.010
