- Visibility 160 Views
- Downloads 7 Downloads
- DOI 10.18231/2581-4729.2019.0010
-
CrossMark
- Citation
Immunotherapy with PPD in treatment of warts: An open labelled study from western Uttar Pradesh
- Author Details:
-
Amit Jaiswal
-
RP Sharma
-
Guneet Bedi
-
Kamna Gupta *
Abstract
Introduction: Warts are the viral infection of the skin caused by Human Papilloma Virus occurring in form of verrucous growth over the surface of the skin. Incomplete removal or local recurrence of the infection is the disadvantage with the currently available local tissue destructive therapies. Newer therapy i.e. intralesional immunotherapy with purified protein derivative offers the advantage of taking care of viral infection not only at treatment site but also at the remote site and also offers life long immunity.
Materials and Methods: The study was conducted on 51 patients of warts of all ages at LLRM Medical College, Meerut. After clinical examination, patients were given 0.1 ml of 5 TU of PPD intralesionally in the largest wart at an interval of one week for six weeks. Patient’s assessment in follow up visits was done with clinical photographs and by filling proforma for effects and side effects.
Results: Complete clearance was seen in 35(68.6%) patients, partial clearance in 6(11.7%) patients, and no clearance in 10(19.6%) patients. The variation in response in different morphologic type of warts was as follows: Periungual and palmar wart 100% clearance, plantar wart 78.5% clearance, verruca plana 60% clearance and verruca vulgaris showed 47% clearance.
Conclusion: PPD immunostimulation is worth in all types of warts. It can be used as a valuable first line treatment in difficult to treat sites like palmoplantar wart and periungual wart.
Keywords: Wart, PPD, Immunotherapy.
Introduction
Warts are the viral infection of the skin caused by Human Papilloma virus, which manifest in the form of verrucous growth over the surface of skin. HPV is a DNA virus that infects skin or mucosal cells. It infects the basal layer of epithelium, possibly the stem cells, but viral replication takes place only in fully differentiated keratinocytes i.e. cells of the stratum spinosum and stratum granulosum. All papilloma virus types have a tropism for stratified squamous epithelial cells, but they vary in their specificity for different anatomical sites like cervix, skin etc.[1]
There are certain predisposing factors for warts like usage of swimming pools or shower room in plantar warts, nail biting in common warts, shaving in beard area for verruca plana over the face, handling in occupational handlers for palmar warts and iatrogenic from instruments like colposcope, smoke fume in laser/electrocautery, cotton swabs in cryotherapy. Anogenital warts in both adults and children can be transmitted via both sexual and non-sexual route.[1] Once the warts have occurred, approximately 23% of them regress spontaneously within 2 months, 30% regress within 3 months and 65% to 78% within 2 years.[2] Although, most warts (65-78%) do resolve spontaneously but it is the tendency to spread the infection, cosmetic disfigurement and sometimes pain for which patients seek treatment.
There are various ways of treatment (medical and surgical) for warts but incomplete removal is quite common with these locally destructive therapies used such as electrocautery, cryotherapy, excision, curettage, keratolytics, laser therapy or topical immunotherapy in form of Dinitrochlorobenzene, Squaric acid dibutyl ester, imiquimod, or tuberculin jelly.[3],[4]
So, this kind of treatment is a reason for frustration in patients as well as the treating physician. Another problem is of local recurrence or pseudo kobner phenomenon. In male, local trauma due to shaving carries the risk of transmitting the infection to the other site in the beard region. So, local tissue destructive therapies at these sites is a failure at times.
Currently, a newer form of therapy is in trend which is known as immunotherapy. This involves the amplification or activation of the patient’s immune system with the help of immunomodulators. Intralesional immunotherapy uses purified protein derivative,[5][6]candida antigen,[7],[8] trychophytin skin test antigen.[9] MMR vaccine,[10] or Mw vaccine,[11] to treat warts.
In Intralesional immunotherapy, a delayed hypersensitivity response develops to the injected antigen and the wart tissue. It is usually seen that there is development of TH1 cytokines which activate cytotoxic and NK cells to eradicate the HPV infection.[2]
Intralesional immunotherapy carries an advantage of developing or augmenting the host immune response to the wart antigen. So, it is helpful for destroying the wart infection at the disease as well as at the remote site. It confers immunity to wart antigen for future also, so it is helpful in reducing the chance of recurrence also.[11]
It has been found that responders to intralesional immunotherapy have a significant positive peripheral mononuclear cell proliferation assay as compared to nonresponders (P=0.002).[12]
Current Indications of immunotherapy are– recalcitrant wart, difficult to treat area or extensive wart, but in our study, we took immunotherapy as primary treatment modality in all patients. Our study is different from the previous studies as we have not given any sensitization dose to the patients and the interval of PPD injections was kept as one week.
Materials and Methods
The study was conducted at LLRM medical college, Meerut. Total 51 patients with viral warts were included in the study. An informed consent was taken before including the patients in the study group.
Intralesional immunotherapy in form of tuberculin PPD was used to demonstrate the effectiveness and safety in patients of all age group.
Inclusion criteria included patients of any age from 1year to a maximum of 75yrs with single or multiple wart and not on any systemic or topical therapy or patients who have not responded to previous treatment.
Exclusion criteria included pregnant and lactating females, patient on immunosuppressive treatment, patients with keloids, fever or local infection or past history of allergy, asthma, skin allergy, meningitis, convulsions or patients with immunocompromised status.
All patients were clinically examined for age, sex, type of wart, number of warts, duration and site.
0.1ml of 5 TU tuberculin PPD (ARKRAY Healthcare Pvt Ltd MRP140/-) was injected intralesionally in largest wart with the help of insulin syringe in every patient at a regular interval of 1 week for a maximum of 6 injections. Patients were followed up every week for clinical improvement and after completion of treatment, further follow up was kept at an interval of 2 weeks for 3 months.
The changes or improvement was observed with the help of clinical photographs taken at baseline before treatment, at 3 weeks and 6 weeks of completion of treatment.
The response was concluded as complete clearance when the warts were totally resolved, partial clearance when the warts were decreased or minimized in size and no response when there was no change in number or size.
Patient were stopped giving PPD, once either the patient got clearance of the lesion or if the patient did not respond even after 6 visits, but all the patients were followed up for duration of 3 months and they were asked for any complaints or any side effects in form of pain, redness or swelling at each visit.
Results
In our study, maximum number of patients were between 11-40yrs (78.43%). Mean age of patients was 29 years. Out of 51 patients, 28 were males and 23 were females. The most common site of wart was forearm and hands (in 24 patients) followed by foot (in 11 patients). Fifteen patients were having single lesion, 16 patients with 2-5 lesions, 8 patients with 6-10 lesions and 2 patients were having lesions more than 10. Maximum number of patients were of multiple warts i.e. 36(70%). The most common type of wart was verruca vulgaris (17/51 i.e. 33.3%) followed by plantar wart (14/51 i.e. 27.5%). The most common symptom with which patients presented to us was asymptomatic in (26/51 i.e. 51%) followed by pain (23/51 i.e. 45%) and itching (2/51 i.e. 4%).
The mean duration of disease was 11 months.
Complete clearance (table 1) was seen in 35 patients, partial clearance in 6 patients and no response in 10 patients. In case of multiple warts, 23 out of 36 patients showed complete clearance, while in case of single wart 12 out of 15 patients showed complete clearance.
Table 1: Response to PPD treatment in patients
|
Type of clearance |
No. of Patients |
Percentage% |
|
Complete clearance |
35 |
68.6 |
|
Partial clearance |
6 |
11.7 |
|
No clearance |
10 |
19.6 |
Out of 35 patients showing complete clearance, 13 patients cleared of the disease in 2-3 visits and in 22 patients, clearance was observed in 5th visit or more.
In case of plantar wart or periungual volar wart, pain was the first symptom to respond. In 2nd to 3rd visit, patients got drastic relief in their pain.
Table 2: Complete clearance in various types of warts was as follows:
|
Type of wart |
Total number of wart |
Number cleared |
Percentage % |
|
Plantar wart |
14 |
11 |
78.5 |
|
Periungual wart |
7 |
7 |
100 |
|
Palmar wart |
2 |
2 |
100 |
|
Verruca plana |
10 |
6 |
60 |
|
Verruca vulgaris |
17 |
8 |
47 |
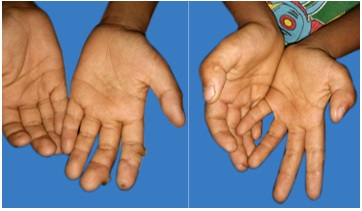
Number of patients showing complete clearance in plantar wart (Fig. 1) were 11 out of 14 patients (78.5%), in periungual wart (Fig. 2) 7 out of 7 patients (100%), palmar wart (Fig. 3) 2 out of 2 patients (100%), verruca plana (Fig. 4) 6 out of 10 patients (60%) and verruca vulgaris(Fig. 5) 8 out of 17 patients (47%). (Table 2)
Mean age of responders was 26 years while of non-responders was 36 years.
In the present work, response was seen in 2nd to 3rd visit at injection site and in 5th to 6th visit at remote site, so there was a gap of one month in response at the injection site and at the remote site
Few side effects of the PPD injection were also observed which include pain in 3 patients (5.8%) and swelling (Fig. 6) at site of injection in 10 patients (19.6%).
 |
Click here to view |
Fig. 1: 19 years female plantar wart (a) pretreatment and (b) complete clearance after 5 weeks.
 |
Click here to view |
Fig. 5: 50 years male with verruca vulgaris (a) pretreatment and (b) complete clearance after 6 weeks.
 |
Click here to view |
Fig. 2: 38 years female periungual wart (a) pretreatment and (b) complete clearance after 5 weeks.
 |
Click here to view |
Fig. 6: Erythema and swelling after PPD injection in a patient of verruca vulgaris.
 |
Click here to view |
Fig. 3: 6 years male palmar wart (a) pretreatment and (b) complete clearance after 5 weeks.
 |
Click here to view |
Fig. 4: 22 years male plane wart (a) pretreatment and (b) complete clearance after 4 weeks.
Discussion
In HPV infection, cell mediated immunity has important role for regression of the viral load. Spontaneously regressing wart shows significant number of CD4+ activated lymphocytes in epidermis as well as in dermis as compared to the non-regressing lesions.[13] Developing countries like India has high load of tuberculosis infection. That’s why, we used PPD to induce positive CMI against HPV.
How the PPD clears the wart, its mechanism is not very well established but various studies suggest that when PPD is injected into the wart tissue, it induces the release of various pro-inflammatory chemicals. These in turn, cause activation of APC (antigen presenting cell), which recognize and then process the HPV at the local site.[13]
This leads to the development of robust adaptive immune reaction against mycobacterium tuberculosis as well as against HPV infection.[14],[15],[16] It is mediated byTh1 cytokines such as interleukin-4, 5,8, IFN-ý and TNF-?. An increase in IL-12 as a process in boosting the cell mediated immunity also contributes to the mechanism of action.[17]
In our study, the mean age of responders was 26 years while in non-responders, it was 36 years (p=0.122); thus, there was no significant difference between the age of responders and non-responders.
In a study of Nimbalkar et al[11] no significant difference was found between the age of responders and non-responders. Abo Elela et al[13] in their study reported that the response to PPD was better with older age.
Patients who had responded to treatment, the mean duration of the lesions was 12 months while it was 8 months in non-responders (p=0.574) which was not statistically significant. Nimbalkar et al[11] in their study demonstrated that response to PPD was not affected by the duration of disease.
In the present study, out of 51patients, 35 patients (68.6%) showed complete clearance, 6 patients (11.7%) showed partial clearance and 10 patients (19.6%) showed no response. Nimbalkar et al[11] studied the effect of intralesional tuberculin PPD on 45 patients and observed that 28 patients (62.2%) showed complete clearance, 8 patients (17.8%) showed partial clearance and in 9 patients, there was no improvement. So, the results were similar to that of our study. In a study by Kus et al[18] on 18 patients using intralesional tuberculin injection, 5 patients (29%) showed complete clearance, 10 patients (59%) showed partial clearance and 2 patients (12%) showed no response. Reason for the variation in the result of this study might be due to the small number of patients or short duration of treatment. In a study done by Lahti and Hannuksela[19] who used tuberculin (PPD) jelly in treatment of warts, 8 out of 14 patients (57%) showed complete clearance which took 3-4 months.
In our study, the response to PPD at the site of injection was noticed in 2nd to 3nd visit while the response at remote site was seen in 5th to 6th visit.
The gap in response between the injection site and remote site was of 4 weeks i.e. at injection site and remote site, it may be due to time taken for induction of CMI. It suggests that immune response is not restricted only to the site of injection. In a study by Nimbalkar et al[11] the response at anatomically distant site was observed at the same time as at the site of injection. It may be due to the variation in injection content. In a study by Wananukul et al, complete clearance was seen in 93% patients with response rate at distant site of 87%.[20]
Present study showed that clearance of warts was seen in plantar wart (11/14 patients), palmar wart (2/2 patients), periungual wart (7/7 patients), verruca plana (6/10 patients) and verruca vulgaris (8/17 patients). There was one patient with genital wart who did not respond. Our observation of improvement in palmoplantar wart matched with the observation by Nimbalkar et al11 and Wannanakul et al[20] but improvement in periungual wart (100%) in our study did not match with Nimbalkar et al who found no improvement in periungual wart.
In our work, patients with complete clearance showed that in 22/35 patients, response came in 5 or more visits while in 13/35 patients, it came in less than 3 visits. In a study by Saoji et al[21] in 42 patients, complete clearance of warts was seen in only 4 sessions, which may be due to the high injection dose that was 25 TU, 5 times the dose given in our study.
In present study, side effects were minimum as pain was observed by only 3 patients (5.8%) and swelling or erythema in 10 patients (19.6%). Saoji et al[21] also showed that in their study, side effects were mild and included erythema, edema and pain.
Conclusion
We can conclude that PPD immunostimulation is worth in all types of warts. It can be used as a valuable first line of treatment in difficult to treat sites like palmoplantar warts and periungual warts. The patients can be benefitted with improvement in symptoms like pain in short period of time and there is high cure rate and the complications associated with other destructive methods can also be avoided. In addition, immunostimulation provides increased chances of attaining a retained immune response for whole life.
Conflicts of Interest: None
References
- a, b Sterling J C. virus infections. In: Burns T, Breathnach S, Cox N, Griffiths C. Rook’s Textbook of Dermatology 7th ed. Blackwell Science. 2004. P25.39-25.46.
- a, b Sterling JC, Handfield Jones S, Hardson PM, British association of dermatology: guideline for management of cutaneous warts. Br J Dermatol 2001;144:4-11.
- ^ Thomas D Horn, Sandid M Johnson. Intralesional immunotherapy of warts. Arch Dermatol 2005;141:589-594.
- ^ Reichman RC, Oakes D, Bonnez L, et al. Treatment of condylomaacuminatum with three different interferon-gamma preparations administered parenterally. A double blind placebo controlled trial. Inf Dis 1990;162:12070-12076.
- ^ Eassa BI, Abou-Bakr AA, El-Khalawany MA. Intradermal injection of PPD as a novel approach of immunotherapy in anogenital warts in pregnant women. Dermatol Ther 2011;24:137–143.
- ^ Kus S, Ergun T, Gun D, Akin O. Intralesional tuberculin for treatment of refractory warts. J Eur Acad Dermatol Venereol 2005;19:515–516.
- ^ Signore RJ. Candida albicansintralesional injection immunotherapy of warts. Cutis 2002;70:185–192.
- ^ Johnson SM, Roberson PK, Horn TD. Intralesional injection of mumps or Candida skin test antigens: A novel immunotherapy for warts. Arch Dermatol 2001;137:451–455.
- ^ Horn TD, Johnson SM, Helm RM, Roberson PK. Intralesional immunotherapy of warts with mumps, Candida, and Trichophyton skin test antigens: A single-blinded, randomized, and controlled trial. Arch Dermatol 2005;141:589–594.
- ^ Johnson SM, Horn TD. Intralesional immunotherapy for warts using a combination of skin test antigens: A safe and effective therapy. J Drugs Dermatol 2004;3:263–265
- a, b, c, d, e, f Nimbalkar Ajay, PardeSushil, Sharma Ramesh, BorkarMilind. Tuberculin purified protein derivative immunotherapy in the treatment of warts. Indian J drugs Dermatol 2016;2:19-23.
- ^ Thappa Devinder M, ChiramelMinu J. Evolving role of immunotherapy in the treatment of refractory warts. Indian Dermatol online J 2016;7:364-370.
- a, b, c Elela IM, Elshahid AR, Mosbeh AS. Intradermal vsintralesional purified protein derivatives in treatment of warts. Gulf J Deramatol Venereol 2011;18:21-26.
- ^ Froeschke JE, Ruben FL, Blot AM. Immediate hypersensitivity reactions after use of tuberculin skin testing. Clin Inf dis 2002; 34:12-13
- ^ Gupta S, Malhotra AK, Verma KK, Sharma VK. Intralesional immunotherapy with killed Mycobacterium w vaccine for the treatment of ano-genital warts: An open label pilot study. J Eur Acad Dermatol Venereol 2008;22:1089-1093.
- ^ Horn TD, Johnson SM, Helm RM, Roberson PK. Intralesional immunotherapy of warts with mumps, Candida, and Trichophyton skin test antigens: A single-blinded, randomized, and controlled trial. Arch Dermatol 2005;141:589-594.
- ^ Abd -Elazeim FMA, Mohammad GFA, Fathy A, Mohammad RW. Evaluation of IL-12 serum level in patients with recalcitrant multiple common warts treated by intralesional tuberculin antigen. J Dermatol Treat 2014;25:264-267.
- ^ Kus S, Ergun T, Gun D, Akin O. Intralesional tuberculin for treatment of refractory warts. J Eur Acad Dermatol Venereol 2005;19:515-516.
- ^ Lahti A, Hannuksela M. Topical immunotherapy with tuberculin jelly for common warts. Arch Dermatol Res 1982;273:153-154.
- a, b Wananukul S, Chatproedprai S, Kittiratsacha P. Intralesional immunotherapy using tuberculin PPD in the treatment of palmoplantar and periungual warts. Asian Biomed 2010;3:739-743.
- a, b Saoji Vikrant, Lade Nitin R, GadgezoneRutija, BhatArun. Immunotherapy using purified protein derivative in the treatment of warts:- An open uncontrolled trial IJDVL 2016; 82:42-46.
