- Visibility 31 Views
- Downloads 2 Downloads
- DOI 10.18231/j.ijced.2019.064
-
CrossMark
- Citation
A comparative study of Acne Vulgaris with special reference to Therapeutic options
- Author Details:
-
Sunil Kumar *
-
Basanti Devi
-
Veeraoubhadra Goud
Introduction
Acne vulgaris (AV) or simply acne is a human skin disease of the pilosebaceous unitthatcauses noninflammatory lesions (open and closed comedones), inflammatory lesions (papules, pustules, and nodules), and varyingdegrees of scarring.[1] Acne affects skin having dense sebaceous follicles in areas including face, chest and back.[2] Acne vulgaris may be of two forms- inflammatory and noninflammatory.[3] Acne vulgaris is commonly seen in during adolescence and affecting about 80–90% of teenagers in the Western population and lower rate are observed in rural societies.[4],[5] Increased levels of androgens causes Acne and seen mainly during puberty in both genders.[6] Acne vulgaris reduces over time and tends to disappear over the age.[7]
The primary pathogenic factors areincreased and altered sebum production by the sebaceousgland, alterations in the follicular keratinization process, which lead to comedones,follicular colonization by Propionibacteriumacnes, and activation of innate immunity followedby increased inflammation.[8],[9] Although acne is not life-threatening condition, many studies have reported the negative impact on quality of life of adults and adolescents.[10],[11]
Currently many treatments are available for acne; guidelines recommend a combinationof a topical retinoid and an antimicrobial agentfor majority of the patients in order to targetinflammatory and non-inflammatorylesions.[12] Acne typically requires prolonged treatment; poor adherence to acnetherapies has been documented. Dreno B et al., found poor adherence in 50% of participantsprescribed treatment for acne; adherencerates reported in Europe were lower than thosereported in the Americas or Asia.[13] Dissatisfactionwith treatment has been closely associatedwith poor adherence.[14] The present study aimed to compare the therapeutic efficacy of various drugs used in different grades of acne accordingly.
Materials and Methods
This study prospective comparative study was conducted in the Department of Skin and Venereal Diseases, SCB Medical College and Hospital, Cuttack, Odisha. Patients visiting the department of Skin & VD at SCBMedical College and Hospital were recruited as study subjects. Total number of patients were 80. The age of the study subjects was 15-25 years of both genders. Forty p atients with mild degree of acne consisting of mainly comedones were included as group I and forty patients with moderate degree of acne having mainly papules and pustules were considered as group II. Pregnant or lactating female, hypersensitive to drugs, children below 12 years of age and patients who have received either topical or oral treatment for acne in the past 4 weeks. Group I patients were divided into two groups – Tretinoin group (0.004% gel local application in the night) [Supratret] and Adapalene group (0.1% gel local application in the night) [Apgel]. All these patients were given the topical gel as per the dosage schedule over a period of 12 weeks. Group II patients were divided into two groups - Clindamycin (1% gel local application in the morning and evening) [Clear Gel] and Clindamycin 1% gel local application in the morning plus Benzoyl peroxide 5% cream local application in the night [Bengel]. All these patients were given topical gel as per the dosage schedule over a period of 12 weeks. The change occurred in acne lesions were recorded every 2 weekly follow-up using global assessment improvement scale. Response to therapy grading done as, if reduction of lesions >90% as excellent, 60-90% as good response, 30-60% as fair response and <30% as poor response.
Results
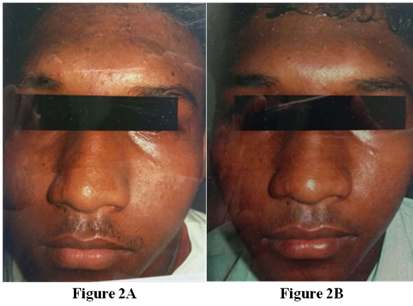
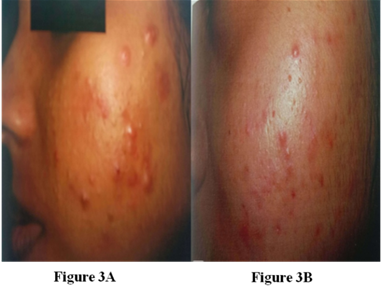
In the present study, 80 subjects were studied. Patients applied the test materials to the entire facial area in the night, for a period of 12 weeks. Efficacy and cutaneous tolerance were assessed at baseline and 2,4,6,8,10 and 12 weeks. Efficacy was determined counting the no. of inflammatory open and closed comedones as well as global improvement. Cutaneous tolerance was evaluated by erythema, scaling and dryness along with burning and pruritus. Table 1 shows the response of Tretinoin 0.04% Vs Adapalene 0.1% ([Table 1] [Figure 1] A,B, [Figure 2] A,B respectively) and table 2 shows the Clindamycin 1% gel Vs Clindamycin 1% gel and Clindamycin 1% gel and Benzoyl peroxide 5% cream ([Table 2] and [Figure 3] A,B, [Figure 4] A,B respectively).
| At the end of 2 weeks | ||||
| Drug | Poor response | Fair response | Good response | Excellent response |
| Tretinoin (0.04%) | 13 (65%) | 5 (25%) | 2 (10%) | 0 |
| Adapalene (0.1%) | 8 (40%) | 6 (30%) | 5 (25%) | 1 (5%) |
| At the end of 4 weeks | ||||
| Tretinoin (0.04%) | 7 (35%) | 10 (50%) | 3 (15%) | 0 |
| Adapalene (0.1%) | 3 (15%) | 4 (20%) | 10 (50%) | 3 (15%) |
| At the end of 6 weeks | ||||
| Tretinoin (0.04%) | 4 (20%) | 5 (25%) | 10 (50%) | 1 (5%) |
| Adapalene (0.1%) | 2 (10%) | 2 (10%) | 10 (50%) | 3 (15%) |
| At the end of 8 weeks | ||||
| Tretinoin (0.04%) | 3 (15%) | 5 (25%) | 11 (55%) | 1 (5%) |
| Adapalene (0.1%) | 2 (10%) | 3 (15%) | 8 (40%) | 4 (20%) |
| At the end of 10 weeks | ||||
| Tretinoin (0.04%) | 2 (10%) | 2 (20%) | 12 (60%) | 2 (10%) |
| Adapalene (0.1%) | 2 (10%) | 2 (10%) | 9 (45%) | 4 (20%) |
| At the end of 12 weeks | ||||
| Tretinoin (0.04%) | 2 (10%) | 3 (15%) | 12 (60%) | 3 (15%) |
| Adapalene (0.1%) | 2 (10%) | 2 (10%) | 12 (60%) | 4 (20%) |
At the end of 12 weeks treatment, 75 % of patients using Tretinoin showed good response to excellent response and 25% patients showed poor to fair response. At the end of 12 weeks treatment, 80% of patients using Adapalene showed good response to excellent response and 20% patients showed poor to fair response. There is no significant difference in the results between two groups (p=0.98). Topical Adapalene is eqally efficacious as Tretinoin. Adapalene 0.1% gel is equally efficacious as Tretinoin 0.04% in mild degree of acne. Cutaneous side effects were limited to a mild “ retinoid dermatitis” occurring in both treatment groups; however, patients treated with adapalene gel tolerated this therapy significantly better than those treated with tretinoin gel.

| At the end of 2 weeks | ||||
| Drug | Poor response | Fair response | Good response | Excellent response |
| Clindamycin (1%) | 11 (55%) | 5 (25%) | 4 (20%) | 0 |
| Clindamycin 1% gel + Benzoylperoxide 5% | 7 (35%) | 7 (35%) | 6 (30%) | 1 (5%) |
| At the end of 4 weeks | ||||
| Clindamycin (1%) | 9 (45%) | 6 (30%) | 5 (25%) | 0 |
| Clindamycin 1% gel + Benzoylperoxide 5% | 5 (25%) | 7 (35%) | 8 (40%) | 3 (15%) |
| At the end of 6 weeks | ||||
| Clindamycin (1%) | 7 (35%) | 7 (35%) | 6 (30%) | 0 |
| Clindamycin 1% gel + Benzoylperoxide 5% | 4 (20%) | 5 (25%) | 10 (50%) | 1 (5%) |
| At the end of 8 weeks | ||||
| Clindamycin 1% gel + Benzoylperoxide 5% | 5 (25%) | 6 (30%) | 9 (45%) | 0 |
| Clindamycin 1% gel + Benzoylperoxide 5% | 3 (15%) | 3 (15%) | 12 (15%) | 2 (10%) |
| At the end of 10 weeks | ||||
| Clindamycin 1% gel + Benzoylperoxide 5% | 4 (20%) | 5 (25%) | 10 (50%) | 1 (5%) |
| Clindamycin 1% gel + Benzoylperoxide 5% | 3 (15%) | 3 (15%) | 12 (60%) | 2 (10%) |
| At the end of 12 weeks | ||||
| Clindamycin 1% gel + Benzoylperoxide 5% | 5 (25%) | 6 (30%) | 8 (40%) | 1 (5%) |
| Clindamycin 1% gel + Benzoylperoxide 5% | 1 (5%) | 1 (5%) | 15 (75%) | 3 (15%) |
At the end of 12 weeks treatment, 45% of patients using only Clindamycin showed good to excellent response. While 90% of patients using both Clindamycin and Benzoyl peroxide showed good to excellent response. Treatment with Clindamycin/Benzoyl peroxide demonstrated a significant benefit over other treatments at week 2, highlighted its rapid onset of action. There is a significant difference between the two groups (p<0.05). Combination of Clindamycin 1% gel with Benzoyl peroxide cream more efficacious than Clindamycin 1% gel alone in reducing the number of lesions in grade 2 acne.

Discussion
Acne vulgaris is a chronic inflammatory disease, characterized by formation of comedones, erythematous papules, pustules, nodules, cysts, abscesses and sometimes widespread scarring developed. According to the severity of acne various topical, systemic and surgical therapies are being used.
In a study by Gollnick H et al., reported that reductions in lesion counts have been reported in the range of 33% to 81% for non-inflammatory lesions, 17% to 71% for inflammatory lesions and 22% to 83% for total lesions. In vehicle-controlled studies, once-daily tretinoin therapy (0.025% gel and 0.025% cream) reduced all types of acne lesions by 40% to50%. The original tretinoin formulations were associated with cutaneous irritation, including erythema, desquamation, burning and pruritus.[15] Grosshans E et al., reported that Adapalene offers comparable efficacy to tretinoin, but is less irritating. It represents a good alternative for the treatment of mild to moderate acne vulgaris.[16] Shalita AR and Weiss JS et al., observed that Adapalene gel 0.1% gel applied once daily was significantly more effective in reducing acne lesions and was better tolerated than tretinoin gel 0.025% in the treatment of acne vulgaris.[17],[18] Overall, there was a 49% to 63% mean reduction in lesions among patients receiving adapalene during 12 weeks of treatment, and the majority of patients (80-89%) were considered to have achieved a favorable clinical response. In addition,adapalene was better tolerated than tretinoin at all evaluation periods.
However, in a double-blind 12 week study, Nyirad et al., reported that tretinoin microsphere gel may have a faster onset of action than adapalene. These reported a greater reduction in comedone counts at 4 week with tretinoin verses adapalene ; reductions in acne lesions at 12 weeks were similar with the two drugs. In this, tretinoin microsphere gel was associated with an increased incidence of dryness and peeling when compared with adapalene gel.[19] In this study, initial response of tretinoin was seen around 2 weeks of therapy. At the end of 2 weeks 35% patients had fair to good response. While 55% of patients using adapalene had fair to good response in 2 weeks.
At the end of 12 weeks treatment, 75% patients using tretinoin showed good to excellent response and 25% patients showed fair to poor response. At the end of 12 weeks of treatment, 80% patients using adapalene showed good to excellent response and 20% patients showed fair to poor response. It suggests that adapalene has early onset of action when compared to tretinoin. Topical adapalene is equally efficacious as tretinoin. Cutaneous side effects were limited to a mild “ retinoid dermatitis ” occurring in both treatment groups; however, patients treated with adapalene gel tolerated this therapy significantly better than those treated with tretinoin gel.
Antimicrobials have been a mainstay of acne treatment for more than 30 years and an active area of research for much of this time. In the past two decades, a substantial armamentarium of topical and systemic agents has been developed and utilized in the treatment of acne. As with all topical medications, the medication should be applied to the entire affected area, usually in the morning and the evening and not only to the visible lesions. Topical antibiotics and benzoyl peroxide are indicated in patients with mild to moderate inflammatory acne.
Warner GT et al., reported that, Clindamycin/benzyl peroxide gel gas demonstrated efficacy and good overall tolerability in several well designed clinical studies in the topical treatment of patients with mild to moderate acne vulgaris. Clindamycin/benzoyl peroxide was more effective than benzoyl peroxide, clindamycin or vehicle and similar in efficacy to benzoyl peroxide/erythromycin in the reduction of inflammatory lesions and in raising physician- and patient- assessed mean global improvement scores. It may be useful in treating patients with acne caused by resistant strains of Propionibacterium acnes. Clindamycin/benzoyl peroxide gel is an effective topical agent in the treatment of patients with mild to moderately severe acne. It is a suitable alternative for patients who are currently using topical antibacterials either alone or in conjunction with other topical anti-acne agents or systemic anti- bacterials. [20] Leyden JJ et al., reported that improved efficacy obtained with the combination therapy was accompanied by a tolerability profile similar to that of benzoyl peroxide alone, making this new combination product an alternative antimicrobial therapy for acne vulgaris. [21]
In our study, 40% of patients using only Clindamycin had fair to good response in 2 weeks whereas 65% of patients using Clindamycin plus Benzoyl peroxide had fair to good response in 2 weeks. At the end of 12 weeks treatment, 45% patients using only Clindamycin showed good to excellent response. While 90% patients using both Clindamycin and Benzoyl peroxide showed good to excellent response. Combination of Clindamycin with Benzoyl peroxide creams are more efficacious than Clindamycin cream alone in reducing the number of lesions in grade 2 acne. Treatment with Clindamycin/Benzoyl peroxide demonstrated a significant benefit over other treatments at 2 week, highlighting its rapid onset of action. Out of 20 patients, 3 patients using Clindamycin and Benzoyl peroxide had side effects like dryness, scaling and irritation after 6 weeks.
Conclusion
The present study showed Adapalene gel produced numerically greater lesion reductions than Tretinoin gel at 2 to 4 weeks of treatment. No significant difference between the two treatments were observed after 12 weeks. Adapalene 0.1% gel was significantly better tolerated than Tretinoin 0.04% gel during the whole treatment period. Hence, Tretinoin 0.04% gel and Adapalene 0.1% gel are equally efficacious in grade 1 acne. Side effects like dryness, erythema, itching was more common with Tretinoin when compared to Adapalene. Significantly greater reductions in the number of inflammatory and total lesions were demonstrated in patients using combination therapy (Clindamycin plus benzoyl peroxide) compared with those using only Clindamycin gel in grade to acne patients. Both physicians and patients global evaluations showed significantly greater improvements with the combination therapy than with its individual components. The most frequent adverse effect, dry skin, occurred in the combination treatment groups. Combination of Clindamycin and Benzoyl peroxide works better than Clindamycin gel alone in grade 2 acne patients.
Conflict of Interest
None.
Source of Funding
None.
References
- A U Tan, B J Schlosser, A S Paller. A review of diagnosis and treatment of acne in adult female patients. Int J Women's Dermatol 2018. [Google Scholar]
- N Benner, D Sammons. Overview of the Treatment of Acne Vulgaris. Osteopath Family Physic 2013. [Google Scholar]
- A Manoj Suva, Ankita M Patel, Neeraj Sharma, Chandrayee Bhattacharya, Ravi K Mangi. A Brief Review on Acne Vulgaris: Pathogenesis, Diagnosis and Treatment. Research and Reviews. J Pharmacol 2014. [Google Scholar]
- M Taylor, M Gonzalez, R Porter. Pathways to Inflammation: Acne Pathophysiology. Eur J Dermatol 2011. [Google Scholar]
- E H Spencer, H R Ferdowsian, N D Barnard. Diet and Acne: A Review of the Evidence. Int J Dermatol 2009. [Google Scholar]
- W D James. Acne. New Engl J Med 2005. [Google Scholar]
- A Laurence. Looking Good, the Australian Guide to Skin Care, Cosmetic Medicine and Cosmetic Surgery. 2006. [Google Scholar]
- Gabriella Fabbrocini, Sara Cacciapuoti, Giuseppe Monfrecola. A Qualitative Investigation of the Impact of Acne on Health-Related Quality of Life (HRQL): Development of a Conceptual Model DermatolTher (Heidelb). 2018. [Google Scholar]
- H C Williams, R P Dellavalle, S Garner. Acne vulgaris. Lancet 2012. [Google Scholar]
- A F Klassen, J N Newton, E Mallon. Measuring quality of life in people referred for specialist care of acne: comparing generic and disease-specific measures. J Am Acad Dermatol 2000. [Google Scholar]
- E Tasoula, S Gregoriou, J Chalikias, D Lazarou, I Danopoulou, A Katsambasa. The impact of acne vulgaris on quality of life and psychic health in young adolescents in Greece. Results of a population survey. An Bras Dermatol 2012. [Google Scholar]
- D Thiboutot, H Gollnick, V Bettoli, B Drno, S Kang, J J Leyden. New insights into the management of acne: an update from the Global Alliance to Improve Outcomes in Acne group. J Am Acad Dermatol 2009. [Google Scholar]
- B Dreno, D Thiboutot, H Gollnick, A Y Finlay, A Layton, J J Leyden. Large-scale worldwide observational study of adherence with acne therapy. Int J Dermatol 2010. [Google Scholar]
- C Renzi, D Abeni, A Picardi, E Agostini, C F Melchi, P Pasquini. Factors associated with patient satisfaction with care among dermatological outpatients. Br J Dermatol 2001. [Google Scholar]
- H Gollnick, W Cunliffe, D Berson, B Dreno, A Finlay, J J Leyden. Global alliance to improve outcomes in acne, management of acne: A report from a global alliance to improve outcomes in acne. J Am Acad Dermatol 2003. [Google Scholar]
- E Grosshans, R Marks, J M Mascaro, H Torras, J Meynadier, M Alirezai. Evaluation of clinical efficacy and safety of adapalene 0.1% gel versus tretinoin 0.025% gel in the treatment of acne vulgaris, with particular reference to the onset of action and impact on quality of life. Br J Dermatol 1998. [Google Scholar]
- A R Shalita, D K Chalker, R F Grifuth, A A Herbert, J G Hickman, J M Maloney. Tazarotene gel is safe and effective in the treatment of acne vulgaris: a multicenter, double-blind, vehicle-controlled study. Cutis 1999. [Google Scholar]
- J S Weiss, J S Shavin. Adapalene for the treatment of acne vulgaris. J Am Acad Dermatol 1998. [Google Scholar]
- J Nyirady, R M Grossman, M Nighland, R S Berger, J L Jorizzo, Y H Kim. A comparative trial of two retinoids commonly used in the treatment of acne vulgaris. J Dermatol Treat 2001. [Google Scholar]
- G T Warner, G L Plosker. Clindamycin/benzoyl peroxide gel: a review of its use in the management of acne. Am J ClinDermatol 2002. [Google Scholar]
- J J Leyden, R S Berger, F E Dunlap, C N Ellis, M A Connolly, S F Levy. Comparison of the efficacy and safety of a combination topical gel formulation of benzoyl peroxide and clindamycin with benzoyl peroxide, clindamycin and vehicle gel in the treatments of acne vulgaris. Am J Clin Dermatol 2001. [Google Scholar]
