- Visibility 38 Views
- Downloads 8 Downloads
- DOI 10.18231/j.ijced.2020.039
-
CrossMark
- Citation
Ocular rosacea: The insight
- Author Details:
-
Tejinder Kaur *
-
Anisha Sethi
-
Niharika Mittal
-
Karamjit Singh
Introduction
The National Rosacea Society Committee identified four subtypes of rosacea: Erythemato-telangiectatic, papulopustular, phymatous and ocular.[1], [2] The diagnosis of ocular rosacea should be considered when the patient’s eyes have one or more of the following signs and symptoms: Watery or bloodshot appearance, foreign body sensation, dryness, itching, light sensitivity, blurred vision, telangiectasia of the conjunctiva and lid margin or lid and periocular erythema. Meibomian gland dysfunction presenting as chalazion or chronic staphylococcal infection are common signs of rosacea-related ocular disease. Some patients may have decreased visual acuity caused by corneal complications (punctate keratitis, corneal infiltrates/ulcer or marginal keratitis).[2] Although the frequency of ocular involvement in patients with rosacea is reported to be somewhere between 3 and 58%, its exact prevalence is not known.[3] In approximately 20% of the patients, eye findings may precede skin changes, making the diagnosis more challenging for both the ophthalmologist and the dermatologist.[1] This study was performed to evaluate the ocular signs and symptoms of rosacea in an Indian population presenting to a tertiary health care centre.
Aim
The study was designed to
Determine the incidence of ocular disease among the population of rosacea patients
To objectively determine the presence of eye dryness in both the patients and controls using Schirmer 1 test.
Correlate the severity of ocular disease with the severity of cutaneous rosacea
Materials and Methods
The study was conducted in Dermatology outdoor of a tertiary care hospital wherein 72 adult facial rosacea patients (32 men and 40 women) with a mean age of 35.8 years (range = 25 - 63) years were enrolled in this study using simple sequential sampling. All patients were questioned and thorough medical history and physical examination including skin manifestations was undertaken and recorded after taking written consent. Clearance from the Ethical Committee of the institute was taken. Each major sign and symptom of rosacea was classified into three groups as shown in [Table 1]. After skin examination, we referred all the 72 patients to an ophthalmology clinic of the same hospital. The ophthalmologist performed a thorough examination of the eyelids, conjunctiva and cornea via slit lamps. Ocular signs including lid, conjunctival, corneal, episcleral, and scleral manifestations as well as charted observations of the iris, lens, intraocular pressures (IOPs), best corrected visual acuity (VA), and funduscopic examination were recorded.
Schirmer 1 test was performed on all patients and controls. With the use of the Schirmer test without anesthesia, the amount of aqueous tear secretion of 30 ocular rosacea patients (18 women, 12 men) with rosacea was compared with that of 30 patients with melanocytic nevi (18 women, 12 men) without rosacea who served as age- and sex-matched controls. The criteria of minimum 4 mm of strip wetting, were used to indicate the lower limit of normal aqueous tear secretion. Results were interpreted as Normal ≥15 mm, Mild 14-9 mm and Moderate 8-4 mm wetting of the paper after 5 minutes.
Results
Out of total 72 patients diagnosed with facial rosacea, 30 (41.62%) were diagnosed with ocular rosacea. The Male: Female ratio was 1:1.5. Thirteen patients with ophthalmic manifestations had mild to moderate erythematotelangiectatic rosacea, 16 had moderate papulopustular rosacea while only 1 had phymatous rosacea. [Table 2] enlists the various symptoms complained by the patients. Of these 22 had symptoms pertaining to ocular manifestations. Dryness in 20 (56.67%) patients was the leading complaint followed by Stinginess and Burning sensation in 14 (46.67%) and 12(40%) patients respectively ([Table 2]). The ophthalmological examination led to the unmasking of various signs of which conjunctivitis was the commonest in 10 (33.33%) patients ([Table 3]).
Results of the Schirmer 1 test are given in [Table 4]. Ocular rosacea patients had a total mean value of 7.6mm which was considerably lower than that of control group 18.5 mm. This difference proved to be statistically significant (p < 0.05). There was also a statistically significant difference between mean Schirmer test values of male patients and controls and female patients and controls. Of the ocular rosacea patients, 56.67% had less than 8 mm of strip wetting compared with 23.3% of control patients (p < 0.05). The prevalence of documented meibomian gland dysfunction i.e dry eyes (p < 0.05), telangiectasia (p = 0.008), was significantly higher in patients when compared with controls. Of the conjunctival signs evaluated, only the presence of interpalpebral conjunctival hyperemia (p = 0.02) was found to be significantly higher in patients. Corneal changes were seen in 1 (3.33%) patients in the form of beginning of superficial punctate keratitis. The corneal, episcleral, scleral, and lens findings did not demonstrate a statistically significant difference between the two groups. Difference between IOP, fundoscopic findings and VA were not significantly different.

| Feature/ Grading | Mild | Moderate | Severe |
| Flushing | Instant flushing | Duration of less than 15 min | More than 15 min of flushing |
| Erythema | Light red erythema | Red erythema, | Purple red erythema, |
| Telangiectasia | Up to 10 lines | 10-20 lines | More than 20 |
| Papules or pustules | Less than 10 | 10-20 | More that 20 |
| Nodules and plaques | 1-3 | 4-10 | More than 10 |
| Ocular Symptoms | Number of patients (%) |
| 1. Dryness | 20 (66.67%) |
| 2. Stinginess | 14 (46.67%) |
| 3. Burning sensation | 12 (40%) |
| 4. foreign body sensation | 12 (40%) |
| 5. Photosensitivity | 8 (26.67%) |
| 6. Excessive watering | 2 (6.67%) |
| Total number of patients | 68 |
| Ocular Signs | Number of Patients (%) |
| 1. Conjunctivitis | 10 (33.33%) |
| 2. Telangiectasias | 9 (30%) |
| 3. Recurrent chalazion | 8 (26.67%) |
| 4. Eyelid swelling | 1 (3.33%) |
| 5. Blepharitis | 1 (3.33%) |
| 6. Superficial punctate keratitis | 1 (3.33%) |
| Total number of patients | 30 |
| Ocular Rosacea patients | Controls | |||||||
| Men | Women | Men | Women | |||||
| L.E | R.E | L.E | R.E | L.E | R.E | L.E | R.E | |
| 7.0mm | 7.5mm | 7.5.mm | 8.5mm | 17.5mm | 19.0mm | 18.0mm | 19.5mm | |
| Mean | 7.25mm | 8mm | 18.25mm | 18.75mm | ||||
| Cumulative Mean | 7.6mm | 18.5mm |
Discussion
Rosacea is a chronic cutaneous disorder that causes high psychological strain in those affected. The ocular manifestations of rosacea are commonly nonspecific and variable. The etiology of the inflammation is unknown and there is no diagnostic test for the disease. Ocular rosacea is often underdiagnosed, despite the potential for serious sight-threatening sequelae.
The Male: Female ratio in our study was found to be 1:1.5. Ocular rosacea affects both genders equally.[4] The incidence of ocular rosacea varies among ophthalmologic and dermatologic studies, ranging from 6-72%, being more prevalent in ophthalmology clinics.[5], [6], [7] Rosacea may be found in early childhood as well as in the elderly, but it most commonly affects middle-aged adults.[8] The mean age in our study was found to be 35.8 years.
Fair-skinned patients of European descent are more commonly affected by rosacea; however, any ethnicity can be afflicted with the disease. It has been suggested that skin pigmentation may obscure identification of the characteristic findings, contributing to underdiagnosis in dark skinned patients.[9] There have been no data so far in an Indian population showing the prevalence and clinical features of ocular rosacea.
Lack of diagnostic test
The diagnosis of rosacea is clinical and relies on observation of skin manifestations. In cases in which these are only very subtle, the diagnosis can become very challenging and the disease may remain undiagnosed. In addition, manifestations of ocular rosacea are by no means specific to the disorder alone and other ophthalmologic diseases may present with similar findings, making the diagnosis even more difficult and the search for a diagnostic test quite important. Unfortunately, there is not yet a diagnostic test available for either cutaneous or ocular rosacea. [10] No serologic or histologic markers have been described to date. A diagnostic marker may enable earlier diagnosis and treatment, as well as contribute with an etiologic explanation for this troublesome disorder. High abundance of O-linked oligosaccharides in the tears of patients has been found in patients with ocular rosacea.[11]
Clinical features
The incidence of ocular manifestations in our rosacea population was found to be 41.62% while other studies have shown to be in the range of 6-58%.[12] This variation probably reflects the difference between sociodemographic profile of population in study, the flare episodes and the means of diagnosis. [13] The real prevalence of ocular rosacea is highly underestimated because the ophthalmic disease usually remains underdiagnosed as patients focus their attention only to the aesthetic appearance their face.[13] The most frequent ocular symptom was dryness (66.67%) and stinginess of the eyes (46.67%) whereas the most common sign was conjunctivitis (33.33%) and telangiectasias (30%). These findings were consistent with other studies. [14], [15], [16], [17], [13], [18] Patients with ocular rosacea may complain of foreign body sensation, dryness, itching, photophobia and tearing.[19], [14] Decreased visual acuity may result when corneal involvement is present. Ocular manifestations are usually bilateral and, as previously mentioned, can be non-specific.[10] The severity of ocular rosacea symptoms is often not related to the severity of cutaneous manifestations.[10], [14] One study found a significant relationship between ocular involvement and the severity of telangiectasia.[15]
Eyelids and tear film
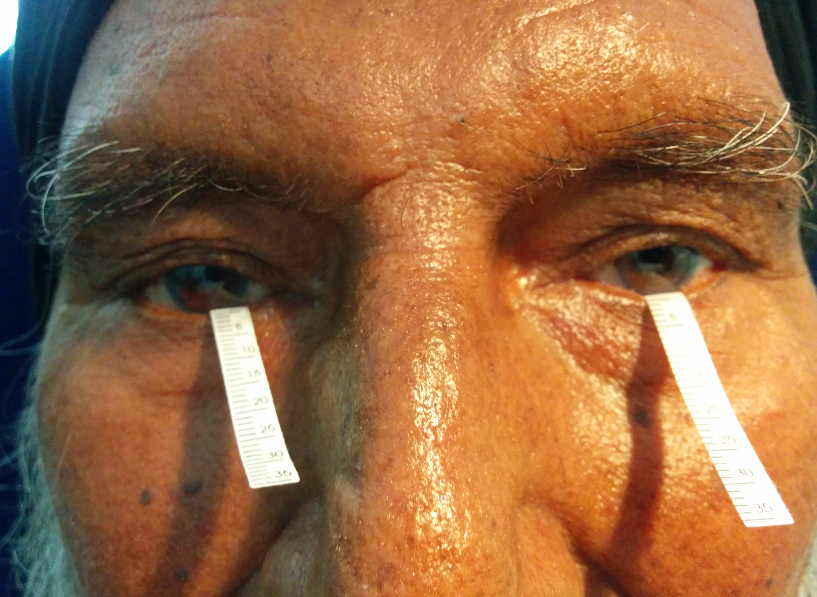
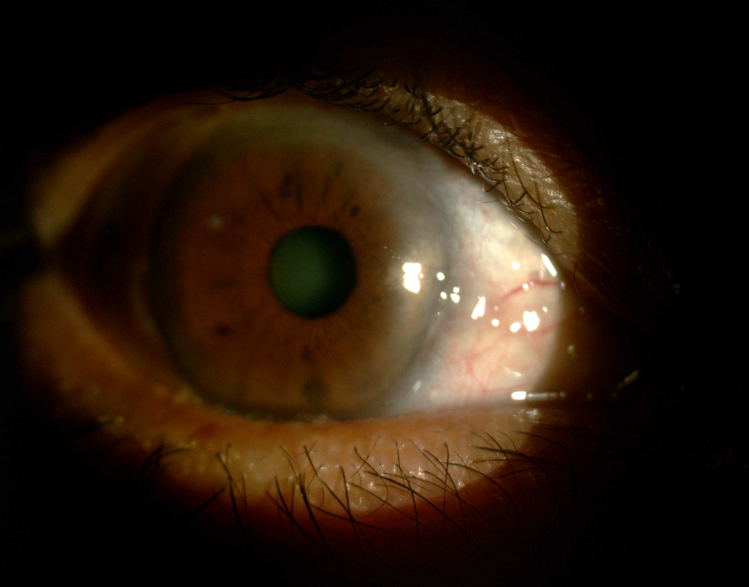
Tear function test i.e Schirmer 1 ([Figure 1]) was performed on 30 out of 72 patients in our study as well as 30 controls, to determine the presence and gravity of eye dryness. Although all eyes were above 5mm i.e pathological dry eyes, the total mean of Schirmer tests were 7.6mm in patients which was significantly lower compared with 18.5 mm score of the controls. Dry eyes, with abnormal Schirmer test, were reported in 56-62.5% of patients with ocular rosacea.[20], [21], [16] Furthermore male rosacea patients had lower value as compared to female patients which was similar to findings in a study by Lazaridou et al.[22] These findings further delineate the fact that rosacea is very often characterized by dry eye and at times is the only presenting symptom/sign. Diminished tear break-up time (TBUT) has also been reported in a large majority of patients with ocular rosacea.[14], [20], [21] In our study there was 1 case of lid edema and blepharitis each. Blepharitis and meibomian gland dysfunction are common findings in patients of ocular rosacea.[6], [10] These glands are considered as differentiated sebaceous glands which are target of inflammation in rosacea. Abnormal function leads to thickened secretions, lower tear break up time and consequently eye dryness.[22] This dysfunction could be secondary to increased glandular production of free fatty acids due to bacterial lipases or to hyperemia because of facial and angular venous dilatation.[23], [24], [25] Slit-lamp examination of the eyelid margins reveals telangiectases ([Figure 2]), dilated meibomian glands, excessive seborrheic secretion and collarettes around the eyelashes.[10] Recurrent hordeolum/chalazion and tear film insufficiency are commonly observed as a consequence of meibomian gland dysfunction.[4], [10] Though facial edema is an uncommon manifestation,[26] periorbital edema and eyelid edema has been reported in the literature.[26], [27]
Conjunctiva
In our study, conjunctivitis was seen in 10 (33.33%) patients. Starr and McDonald described a characteristic ‘arcade’ of dilated vessels in the superficial limbal plexus, usually present in the inferior quadrants and not extending into the cornea in ocular patients of rosacea.[28] Chronic conjunctivitis characterized by interpalpebral bulbar conjunctival hyperemia may be present,[7], [10] as well as a chronic papillary reaction.[6] Akpek et al described cicatricial conjunctivitis (lower lid) as one of the most common ocular surface findings in rosacea.[29] There have been reports of chronic cicatrizing conjunctivitis (upper lids), mimicking the classic findings in trachoma, pinguecula and conjunctival fibrosis have been reported in up to 20% of patients with ocular rosacea. [30], [31], [32]
Cornea
Corneal manifestations may occur in up to 33% of patients with rosacea [6], [28] with the inferior cornea being more commonly affected. [10] In our study one (3.33%) patient showed the features of superficial punctate keratitis ([Figure 3]). Corneal involvement typically starts with superficial punctate keratitis on the lower third of the cornea. [28] Peripheral neovascularization associated with subepithelial marginal triangular infiltrates along the advancing vascular border can also occur. [28] If left untreated, these infiltrates may progress centrally and lead to stromal ulceration and even perforation. [10], [33], [34] Recurrent corneal epithelial erosions have been reported in patients with ocular rosacea. [29], [17], [35] Other uncommon corneal findings include pseudodendritic ulcer and pseudokeratoconus, presenting with inferior corneal thinning and high astigmatism, secondary infectious keratitis. [36]
Other ocular findings
Other ocular findings include iritis, episcleritis and scleritis.[10], [37] In our study, one case of episcleritis was found who had moderate papulopustular rosacea. Decreased visual acuity can also be seen which may result from epithelial ulceration, surface irregularities and corneal scarring.[36] However, in contrast our study did show any severe complications like corneal neovascularization, thinning and perforation, scleral ulcers.
In our study, surprisingly, we found a significant relationship between the severity of telangiectasia and ocular involvement. Similar finding was reported in a study done in Tehran.[15] This finding is not in alignment with the previous studies that claim that the ophthalmologic complications of rosacea are completely independent of the severity of facial rosacea.[12] On the other hand, it seems that the significant relationship between the severity of telangiectasia and eye lesions in our study might be a coincidence. Larger studies with more number of patients need to be undertaken to further extrapolate this fact.
Differential Diagnosis
The differential diagnosis of ocular rosacea may include staphylococcal and seborrheic blepharokerato conjunctivitis, and sebaceous gland carcinoma.[36] Given that there is currently no diagnostic test for rosacea, distinguishing ocular rosacea from staphylococcal and seborrheic blepharo conjunctivitis in patients in which ocular signs precede skin findings may be difficult. Sebaceous gland carcinoma is often misdiagnosed as chalazion and early recognition is often challenging. For this reason, recurrent chalazia should be excised and sent for histopathology.[36] Thus it needs a good clinical suspicion by both a dermatologist and ophthalmologist to get to diagnosis in a setting of minimal but recurrent oculocutaneous symptoms.
Conclusion
Ocular rosacea in its most developed form still remains the domain of the ophthalmologist, still the role of a dermatologist in early diagnosis and management cannot be undermined. Looking and asking for ophthalmic symptoms in any suspected case of rosacea marks an astute clinician. Keeping in mind the clinical symptoms and signs can be a great help to the ailing patients. The findings in our study prove beyond doubt that ocular features of rosacea in patients presenting with mere cutaneous findings should not be overlooked. Furthermore Eye care professionals need to be aware of the presence of rosacea to appropriately treat ocular surface disease that is not responding as expected to standard topical therapy. Ocular rosacea, in particular, is often left undiagnosed as no specific test is available to confirm the diagnosis. Accurate diagnosis is further complicated because symptoms of ocular rosacea are not always specific to the disorder alone. Other ophthalmic disorders may present with similar findings. Further challenges exist because the severity of ocular symptoms is often not related to the severity of cutaneous findings in rosacea. Our study has found the correlation of telangiectasias with that of ocular rosacea.
Acknowledgement
We thank Dr. S.S. Shergill and Dr. K.J.S. Puri for their valuable support.
Source of Funding
None.
Conflict of Interest
None.
References
- E L Tanzi, J M Weinberg. The ocular manifestations of rosacea. Cutis 2001. [Google Scholar]
- Jonathan Wilkin, Mark Dahl, Michael Detmar, Lynn Drake, Matthew H Liang, Richard Odom. Standard grading system for rosacea: report of the National Rosacea Society Expert Committee on the classification and staging of rosacea. J Am Acad Dermatol 2004. [Google Scholar]
- Charles E. Gessert, Joel T. M. Bamford. Measuring the severity of rosacea: a review. Int J Dermatol 2003. [Google Scholar]
- J. Spoendlin, J.J. Voegel, S.S. Jick, C.R. Meier. A study on the epidemiology of rosacea in the U.K.. Br J Dermatol 2012. [Google Scholar]
- Bakar, Z Demircay, E Toker, S Çakır. Ocular signs, symptoms and tear function tests of papulopustular rosacea patients receiving azithromycin. J Eur Acad Dermatol Venereol 2009. [Google Scholar]
- V C Ghanem, N Mehra, S Wong, M J Mannis. The prevalence of ocular signs in acne rosacea: comparing patients from ophthalmology and dermatology clinics. Cornea 2003. [Google Scholar]
- George Wise. Ocular Rosacea* *From the Department of Ophthalmology, Columbia University, College of Physicians and Surgeons, and the Institute of Ophthalmology, Presbyterian Hospital, New York City.. Am J Ophthalmol 1943. [Google Scholar]
- Esther Hong, Gayle Fischer. Childhood ocular rosacea: Considerations for diagnosis and treatment. Australas J Dermatol 2009. [Google Scholar]
- David J. Browning, George Rosenwasser, Miguel Lugo. Ocular Rosacea in Blacks. Am J Ophthalmol 1986. [Google Scholar]
- Melissa Oltz, James Check. Rosacea and its ocular manifestations. Optom 2011. [Google Scholar]
- Hyun Joo An, Milady Ninonuevo, Jennifer Aguilan, Hao Liu, Carlito B. Lebrilla, Lenio S. Alvarenga. Glycomics Analyses of Tear Fluid for the Diagnostic Detection of Ocular Rosacea. J Proteome Res 2005. [Google Scholar]
- J L Michel, F Calibel. Frequency, severity and treatment of ocular rosacea during cutaneous disease. Ann Dermatol Venereol 2003. [Google Scholar]
- Glen H. Crawford, Michelle T. Pelle, William D. James. Rosacea etiology, pathogenesis and subtype classification. J Am Acad Dermatol 2004. [Google Scholar]
- MJ Quarterman, DW Johnson, DC Abele, JL Lesher, DS Hull, LS Davis. Ocular rosacea: signs, symptoms, and tear studies before and after treatment with doxycycline.. Arch Dermatol 1997. [Google Scholar]
- Maryam Akhyani, Alireza Keshtcar-Jafari, AmirH Ehsani, Maryam Ghiasi, Vahide Lajevardi, Oldoos Baradran, Siavash Toosi. Correlation of the severity of cutaneous rosacea with ocular rosacea. Indian J Dermatol Venereol Leprol 2009. [Google Scholar]
- Ken J. Gudmundsen, Brigid F. O’Donnell, Frank C. Powell. Schirmer testing for dry eyes in patients with rosacea. J Am Acad Dermatol 1992. [Google Scholar]
- Mark S. Jenkins, Stuart I. Brown, Steven L. Lempert, Richard J. Weinberg. Ocular Rosacea. Am J Ophthalmol 1979. [Google Scholar]
- V. Yaylali, C. Ozyurt. Comparison of Tear Function Tests and Impression Cytology with the Ocular Findings in Acne Rosacea . Eur J Opthalomol 2002. [Google Scholar]
- H E Baldwin. Diagnosis and treatment of rosacea: state of the art. J Drugs Dermatol 2012. [Google Scholar]
- Pierre-Jean Pisella, Françoise Brignole, Caroline Debbasch, Paul-Alexandre Lozato, Catherine Creuzot-Garcher, Jacques Bara. Flow cytometric analysis of conjunctival epithelium in ocular rosacea and keratoconjunctivitis sicca. Ophthalmol 2000. [Google Scholar]
- E. Lazaridou, C. Fotiadou, N.G. Ziakas, C. Giannopoulou, Z. Apalla, D. Ioannides. Clinical and laboratory study of ocular rosacea in northern Greece. J Eur Academy Dermatol Venereol 2011. [Google Scholar]
- E Lazaridou, Z Apalla, S Sotiraki, NG Ziakas, C Fotiadou, D Ioannides. Clinical and laboratory study of rosacea in northern Greece. J Eur Academy Dermatol Venereol 2010. [Google Scholar]
- Donald U Stone, James Chodosh. Ocular rosacea: an update on pathogenesis and therapy. Curr Opin Ophthalmol 2004. [Google Scholar]
- G Plewig, A M Kligman. Acne and Rosacea. 2000. [Google Scholar]
- Mélanie Chamaillard, Bruno Mortemousque, Franck Boralevi, Claudia Marques da Costa, Farida Aitali, Alain Taïeb. Cutaneous and Ocular Signs of Childhood Rosacea. Arch Dermatol 2008. [Google Scholar]
- B F O’donnell, I S Foulds. Visual impairment secondary to rosacea. Br J Dermatol 1992. [Google Scholar]
- A Morales-Burgos, G Alvarez Del Manzano, J L Sánchez, C L Cruz, . Persistent eyelid swelling in a patient with rosacea. P R Health Sci J 2009. [Google Scholar]
- P A J Starr, Angus MacDonald. Oculocutaneous Aspects of Rosacea. Proc R Soc Med 1969. [Google Scholar]
- E K Akpek, A Merchant, V Pinar, C S Foster. Ocular rosacea: patient characteristics and follow-up. Ophthalmol 1997. [Google Scholar]
- Z B Ravage, A P Beck, M S Macsai, S S Ching. Ocular rosacea can mimic trachoma: a case of cicatrizing conjunctivitis. Cornea 2004. [Google Scholar]
- K B Lima, L B Sousa, N C Santos, N Barros J De, D Antonio. Cost-benefit analysis of ocular examination of patients with rosacea. Arq Bras Oftalmol 2005. [Google Scholar]
- H G Faraj, Hoan. g-Xuan T Chronic cicatrizing conjunctivitis. Curr Opin Ophthalmol 2001. [Google Scholar]
- B Gracner, D Pahor, T Gracner. Repair of an extensive corneoscleral perforation in a case of ocular rosacea with a keratoplasty. Klin Monbl Augenheilkd 2006. [Google Scholar]
- WaseemAl Zamil, KhalidAl Arfaj. Spontaneous corneal perforation in ocular rosacea. Middle East Afr J Ophthalmol 2010. [Google Scholar]
- S Ramamurthi, M Q Rahman, G N Dutton, K Ramaesh. Pathogenesis, clinical features and management of recurrent corneal erosions. Eye 2006. [Google Scholar]
- Ana Carolina Cabreira Vieira, Ana Luisa Höfling-Lima, Mark J Mannis. Ocular rosacea: a review. Arquivos Brasileiros de Oftalmologia 2012. [Google Scholar]
- Lenio S. Alvarenga, Mark J. Mannis. Ocular Rosacea. Surf Ocul 2005. [Google Scholar]
