- Visibility 67 Views
- Downloads 6 Downloads
- DOI 10.18231/j.ijced.2021.031
-
CrossMark
- Citation
Correlation of hypocalcaemia with severity and type of psoriasis: A cross-sectional study
- Author Details:
-
Anshu Maheswari *
-
Bornali Dutta
Introduction
Psoriasis is a chronic, recurrent, inflammatory and proliferative disease of skin caused by T-cell mediated inflammation. Various factors are known to initiate or aggravate psoriatic lesions including infections, stress, cold weather and drugs like lithium, beta blockers, antimalarials. Smoking, alcohol consumption and obesity can trigger it, and psoriasis has also been associated with metabolic syndrome. The severity of psoriasis can be categorized by a variety of scoring systems including Psoriasis Area and Severity Index (PASI) or the Physicians Global Assessment (PGA).
Metabolic disturbance in the form of hypocalcaemia can aggravate psoriasis. This occurs because calcium plays an important role in proliferation and differentiation of keratinocytes. Cell adhesion molecules like cadherins are damaged with a decrease in calcium level. This leads to hyperproliferation of keratinocytes, leading to development or aggravation of psoriasis. Alteration in serum calcium levels has been reported in many studies. Lee et al reported the association of Pustular psoriasis of von Zumbusch with hypocalcaemia.[1] Considering the role of calcium and Vitamin D3 in psoriasis, studies have been conducted to check the efficacy of topical Vitamin D3 preparations in improving psoriatic lesions.[2]
Hence this study was conducted to study the serum calcium levels in various types of psoriasis and to find a correlation, if any, between the severity of psoriasis vulgaris and serum calcium levels. Very few studies have been carried out to study an association of psoriasis and serum calcium level across the world, till date. Moreover, no studies have been carried out from this part of our country, to establish an association between hypocalcaemia and psoriasis severity, calculated by PASI scoring.
Materials and Methods
Selection and description of participants
A cross sectional observational study was conducted in the Department of Dermatology and Venereology of a tertiary care hospital for a period of one year (June 2017 to May 2018). Clinically diagnosed patients of psoriasis attending the OPD for the first time were included in the study, after obtaining written informed consent. Old treated cases, patients with calcium metabolism disorders, renal, hepatic or thyroid dysfunction, history of bone lesions or collagen vascular diseases, and patients on any medications capable of altering the serum calcium or albumin levels were excluded from the study. Psoriasis Area and Severity Index (PASI) score was used to assess the severity of patients with psoriasis vulgaris and categorized into mild (PASI <10) or moderate to severe (PASI >/= 10). Venous samples of patients were evaluated to determine serum calcium and albumin levels and corrected calcium was calculated using the following formula:
Corrected calcium = [0.8 x (4 – patient’s albumin)] + serum calcium (mg/dl)
Ethic
Institutional ethical committee clearance was taken. Informed written consent was obtained from the patients to participate in the study.
Statistics
Data were analysed using SPSS software, version 21.0. Chi-square test was used to find the significance of study parameters on categorical scale [significance was assessed at 5% level of significance] and Pearson test was used to find correlation. The coefficient of correlation r signifies the amount of co-variation between two variables which can range from +1 to – 1 [r = + 1 signifies perfect positive association, r = – 1 signifies perfect negative association, r = 0 signifies no association]. Similarly, r2 signifies the coefficient of determination which is always positive and measures the variance between the variables.
Results
During the study period, 74,970 patients attended the Dermatology outpatient department, of which 206 cases were diagnosed with psoriasis (Prevalence – 0.27%). Out of these, 105 were males and 101 were females with a male to female ratio of 1.04: 1. The mean age of patients was 34.5 + 17.88 years, with age ranging from 3 months to 94 years. The maximum number of patients [49 (23.79%)] belonged to age group of 41-50 years, followed by 43(20.87%) patients in the age group of 11-20 years.
Of the 206 patients, psoriasis vulgaris was the most common presentation [111 patients (53.88 %)], followed by palmoplantar psoriasis in 43 (20.87 %) patients and scalp psoriasis in 20 (9.71%) patients. Erythrodermic psoriasis was found in 11(5.34%) patients, while 10 had pustular psoriasis (4.85%), 6 had flexural psoriasis (2.91%), 4 had guttate type of psoriasis (1.94%) and 1 had genital psoriasis (0.48%).
Of the 111 patients of psoriasis vulgaris, 50 patients (45.04 %) had mild psoriasis with a PASI score of </= 10, while 61 (54.95%) constituted moderate to severe psoriasis (PASI>10). The mean PASI score was 12.67 + 7.84 with scores ranging from 3.2 to 38.5.
Out of 206 patients of psoriasis, 38 patients (18.45%) had reduced serum calcium levels. Twenty three patients were males while 15 patients were females. Nine patients (8.1 %) of psoriasis vulgaris had hypocalcaemia which was statistically significant [p value - 0.000035]. The mean PASI score of patients of psoriasis vulgaris having hypocalcemia was 29.0 + 7.42. None of the patients with mild disease (PASI <10) had hypocalcaemia. Eight (72.72%) patients of erythroderma and 9(90%) patients of pustular psoriasis showed hypocalcaemia, both having p values of <0.00001 which was also significant. Palmoplantar psoriasis and scalp psoriasis were associated with hypocalcaemia in 9(20.9%) and 3 patients (15%) respectively, but the p values were not significant. None of the patients of flexural, guttate and genital psoriasis showed reduced calcium levels. [[Table 1]]
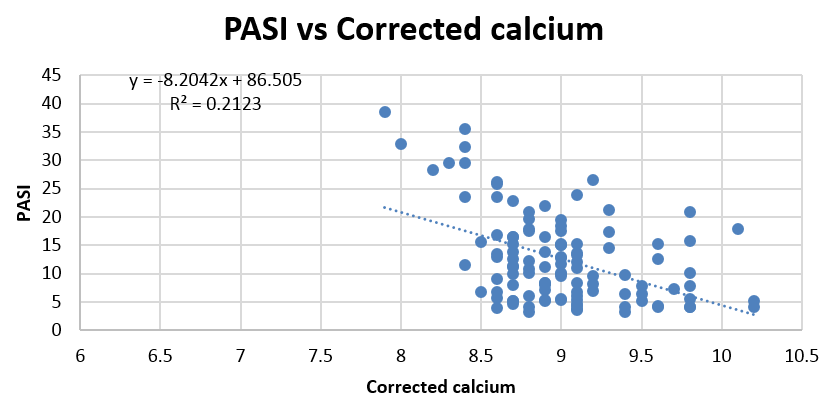
On comparing the correlation of the severity of psoriasis (PASI score) with corrected calcium levels on a scatter plot, the Correlation Coefficient was found to be -0.4607 which is significant at 0.01 level and the relationship is moderately strong. This indicates that as the PASI score increases, we expect a decrease in the corrected calcium level. The coefficient of determination (R2) was found to be 0.2122. [[Figure 1]]
|
Type of psoriasis |
Hypocalaemia |
Normocalcaemia |
p value |
||
|
No. |
Percentage |
No. |
Percentage |
||
|
Psoriasis vulgaris (n = 111) |
9 |
8.1 |
102 |
91.9 |
.000035 |
|
Palmoplantar psoriasis (n = 43) |
9 |
20.9 |
34 |
79.1 |
0.637 |
|
Scalp psoriasis (n = 20) |
3 |
15 |
17 |
85 |
0.676 |
|
Erythroderma (n = 11) |
8 |
72.72 |
3 |
37.5 |
<0.00001 |
|
Pustular psoriasis (n = 10) |
9 |
90 |
1 |
10 |
<0.00001 |
|
Flexural psoriasis (n =6) |
0 |
0 |
6 |
100 |
0.237 |
|
Guttate psoriasis (n = 4) |
0 |
0 |
4 |
100 |
0.337 |
|
Genital psoriasis (n= 1) |
0 |
0 |
1 |
100 |
0.634 |
|
Total |
38 |
18.45 |
168 |
81.55 |
|
Discussion
Psoriasis is an immune-mediated, chronic inflammatory disease affecting various aspects of patients’ lives far beyond the skin, challenging clinicians in its management. While psoriasis is prevailing worldwide, there are regional differences in its epidemiological characteristics.
The prevalence of psoriasis was 0.27% in our tertiary care hospital which was lower as compared to other studies. The National Psoriasis Foundation clinical consensus on disease severity[3] estimated the worldwide prevalence of psoriasis to be approximately 2–3%. However, the burden of psoriasis was found to be higher in areas with extremes of climate compared to areas with a milder climate. Also, dietary habits and genetic differences lead to a difference in the prevalence of psoriasis. Moreover, as psoriasis is becoming a relatively common disease, patients are being increasingly treated by the periphery health care providers and the doctors. This, along with a milder climate, has probably led to a reduced number of new, untreated cases in our tertiary care centre leading to a reduced prevalence rate. The higher prevalence rate in other studies can also be attributed to the inclusion of old, treated cases of psoriasis in their studies.
The mean age of patients in our study was found to be 34.5 + 17.88 years with age ranging from 3 months to 94 years. This was similar to studies by Nevitt et al [4] [mean - 33 years] and Kaur et al[5] [mean – 33.6 years]. However, Vijayan et al[6] [mean – 44.17 years] and Loo et al[7] [mean – 44.6 years] found the mean age to be higher. The difference in the mean age between the various studies could be because Nevitt et al [4] and Kauret al [5] had a similar age group compared to our study, including patients from infancy to the 8th decade, resulting in a similar mean age, while most of the other studies did not include the childhood age group.
A bimodal age distribution was observed in our study with maximum number of patients belonging to the age group of 41 – 50 years (23.79%) followed by 11 – 20 years (20.87 %). This pattern of distribution having two peaks, in adolescence and after 40 years, was also observed by Bell et al, [8] Huerta et al [9] and Icen et al. [10] However, the bimodal age distribution was not found by Vijayan et al, [6] Dogra et al[11] and Ramana et al, [12] which could be because they included only adults in their study population, leading to the absence of the first peak found during adolescence.
Our study population comprised of 206 patients, with 105 males and 101 females. Males and females were found to be equally affected by psoriasis in our study, with a male to female ratio of 1.04 : 1, which was similar to the ratio observed by other studies including Loo et al, [7] Lomholt [13] and Farber and Nall.[14] However, most of the studies in the developing countries have shown a male preponderance in psoriasis.[5], [11], [12], [15] This could be because, in most of the developing countries, females attend health care facilities less frequently as compared to males, more so when the lesions involve covered areas. Moreover, males are more predisposed to the precipitating factors like trauma, infection, alcohol and smoking.
Psoriasis vulgaris or plaque type psoriasis was the most common type of psoriasis encountered [111 (53.88%) patients], followed by palmoplantar psoriasis in 43(20.87%) patients and scalp psoriasis in 20(9.71%) patients. This was similar to all other studies reporting chronic plaque psoriasis to be the commonest type. [5], [6], [7], [12], [15]
Of the 206 patients of psoriasis in our study, hypocalcaemia was present in 38 (18.45%) patients. Twenty three patients were males while 15 patients were females. Hypocalcaemia was significantly associated with pustular psoriasis [9 (90%) patients], erythrodermic psoriasis [8 (72.72%) patients] and psoriasis vulgaris [9 (8.1 %) patients].
Rawat et al [16] found hypocalcaemia in 21% of their patients, which was similar to our study. All patients of erythroderma, psoriatic arthritis and pustular psoriasis had hypocalcaemia. However, 16.3% of patients of psoriasis vulgaris showed low calcium levels, which was higher than that found in our study. This difference in the occurrence of hypocalcaemia in plaque psoriasis is difficult to interpret as they did not comment on the severity of plaque psoriasis (PASI score) in their patients and did not compare the serum calcium levels with the severity of psoriasis.
Qadim et al [17] conducted a study on hospitalised patients of psoriasis and reported hypocalcaemia to be present in 37.5% of their patients. This was similar to the results in our study. Nineteen (50%) patients of pustular psoriasis, 4 (100%) patients of erythroderma and 14(24.5%) of patients of psoriasis vulgaris had hypocalcaemia in their study. We had a higher percentage of patients showing hypocalcaemia in pustular psoriasis possibly because of more extensive involvement by pustular lesions in our cases as all these patients had generalized pustular psoriasis. Their study reported hypocalcaemia in all the 4 patients of erythroderma, while we found hypocalcaemia in 8 of the 11 patients of erythrodermic psoriasis. The difference in the percentage of patients having hypocalcaemia in plaque psoriasis could be because they included hospitalized patients of psoriasis only, accounting for more severe disease in their patients, while our study included all patients of psoriasis including those with mild disease.
Puri et al [18] found hypocalcaemia in 10% of their patients, which was significant. Similarly, Goud et al,[19] Deepthi et al[20] (5%) and Solak et al [21] also reported significant association of psoriasis with hypocalcaemia, but they did not specify the association of hypocalcaemia to the type of psoriasis.
A moderately strong negative correlation was found between severity of psoriasis vulgaris and corrected calcium levels in our study, indicating a decrease in corrected calcium levels with an increase in PASI score. The Correlation Coefficient was -0.4607.
Morimoto et al[22] studied the association between serum calcium levels and severity of skin lesions in psoriasis vulgaris. They found significant hypocalcaemia in patients of psoriasis compared to control group. They also concluded that a decrease in serum calcium and vitamin D3 levels were associated with severe skin lesions.
Chaudhari et al[23] also found a significant reduction in serum calcium levels in patients of psoriasis vulgaris compared to control group, but they could not demonstrate a statistically significant association of hypocalcaemia with severity of psoriasis. Gisondi et al [24] and Nayak et al[25] also conducted studies on psoriasis vulgaris only, but they failed to demonstrate any association with hypocalcaemia.
Zhai et al[26] determined pre-treatment calcium levels before administration of methotrexate to patients with severe plaque type psoriasis. They found significantly better improvement in patients who were treated with calcium before methotrexate. A positive correlation was also found between pre-treatment calcium levels and degree of improvement.
Conclusion
Psoriasis is a common dermatological disorder with significant physical, mental and psychological impact on a person, thereby hampering his personal and social life. Despite being a common disease, there is a paucity of data regarding the various aggravating factors, including any association with reduced calcium or vitamin D3 levels, and also whether correction of these factors can prevent progression to severe disease.
We found a significant association of hypocalcaemia in psoriasis vulgaris, pustular psoriasis and erythrodermic psoriasis. Also a moderately strong association was found between the severity of psoriasis vulgaris, as evaluated from PASI scoring and serum calcium levels. Localized and relatively stable forms of the disease like mild form of plaque psoriasis, scalp palmoplantar and guttate psoriasis and did not show the association as seen with erythrodermic pustular and chronic plaque psoriasis (moderate to severe disease) Thus, correcting the calcium levels by dietary or oral supplements might prove to be beneficial in providing a better outcome and preventing progression of mild, stable disease to severe forms. Despite the small sample size and lack of randomization in our study, encouraging results were found which helped in determining hypocalcaemia as an aggravating factor. More research and detailed prospective studies with a larger sample size need to be done to determine the exact strength of association between calcium levels and disease severity.
Source of Funding
No financial support was received for the work within this manuscript.
Conflicts of Interest
There are no conflicts of interest.
References
- Y Lee, YH Nam, JH Lee, JK Park, YJ Seo. Hypocalcaemia-induced pustular psoriasis-like skin eruption. Br J Dermatol 2005. [Google Scholar] [Crossref]
- J Cook, B Thiers. Serum calcium and phosphorus measurements in patients with psoriasis: a retrospective review. J Eur Acad Dermatol Venereol 1993. [Google Scholar] [Crossref]
- DM Pariser, J Bagel, JM Gelfand, NJ Korman, CT Ritchlin, BE Strober. National Psoriasis Foundation Clinical Consensus on Disease Severity. Arch Dermatol 2007. [Google Scholar] [Crossref]
- G J Nevitt, P E Hutchinson. Psoriasis in the community: prevalence, severity and patients' beliefs and attitudes towards the disease. Br J Dermatol 1996. [Google Scholar]
- I Kaur, S Handa, B Kumar. Natural History of Psoriasis: A Study from the Indian Subcontinent. J Dermatol 1997. [Google Scholar] [Crossref]
- M Vijayan. Prevalence, clinical profile and prescribing pattern of psoriasis in a tertiary care referral hospital. Intl J Pharm Tech 2010. [Google Scholar]
- C H Loo, Y C Chan, K Q Lee, T Palanivelu, W C Tan. Clinical profile, morbidity and outcome of adult patients with psoriasis at a district hospital in Northern Malaysia. Med J Malaysia 2015. [Google Scholar]
- L M Bell, R Sedlack, C M Beard, H O Perry, C J Michet, L T Kurland. Incidence of psoriasis in Rochester, Minn, 1980-1983. Arch Dermatol 1980. [Google Scholar]
- C Huerta, E Rivero, LAG Rodríguez. Incidence and Risk Factors for Psoriasis in the General Population. Arch Dermatol 2007. [Google Scholar] [Crossref]
- M Icen, CS Crowson, MT McEvoy, FJ Dann, SE Gabriel, HM Kremers. Trends in incidence of adult-onset psoriasis over three decades: A population-based study. J Am Acad Dermatol 2009. [Google Scholar] [Crossref]
- S Dogra, R Mahajan. Psoriasis: Epidemiology, clinical features, co-morbidities, and clinical scoring. Indian Dermatol Online J 2016. [Google Scholar] [Crossref]
- GV Ramana, P Malini, N Arun. Patterns of psoriasis in patients attending DVL OPD at Osmania General Hospital-a prevalence study. Int J Contemp Med Res 2017. [Google Scholar]
- G Lomholt. Prevalence of skin diseases in a population; a census study from the Faroe Islands. Dan Med Bull 1964. [Google Scholar]
- E M Farber, M L Nall, HH Psoriasis Roenigk, HI Maibach. Epidemology: Natural history and genetics. 3rd Edn. 1998. [Google Scholar]
- C Raghuveer, D R Shivanand, N Rajashekar. A clinico-histopathological study of psoriasis. Int J Sci Stud 2015. [Google Scholar]
- L Rawat, R Kothiwala, A Mehra, A Meherda, D Bohara, RR Kumar. Serum calcium level in patients suffering from psoriasis and its correlation with severity of psoriasis: A case control study. Int J Multispeciality Health 2019. [Google Scholar]
- HH Qadim, F Goforousha, SB Nejad, M Goldust. Studying the Calcium Serum Level in Patients Suffering from Psoriasis. Pak J Biol Sci 2013. [Google Scholar] [Crossref]
- N Puri, B B Mahajan. A study of clinical and biochemical correlation in patients of psoriasis in acute exacerbation. J Pak Assoc Dermatol 2016. [Google Scholar]
- B M Goud, S S Avinash, M Amareshwara. Antioxidant vitamins, calcium and phosphorus levels in psoriasis. Int J Pharma Bio Sci 2010. [Google Scholar]
- E Deepthi, S Vijayakumar, D Ramchander. A Hospital Based Crosssectional Study on Early and Late onset Psoriatic Patients. Indian J Pharm Pract 2012. [Google Scholar]
- B Solak, BS Dikicier, HD Celik, T Erdem. Bone Mineral Density, 25-OH Vitamin D and Inflammation in Patients with Psoriasis. Photodermatol photoimmunol Photomed 2016. [Google Scholar] [Crossref]
- S Morimoto, K Yoshikawa, K Fukuo, T Shiraishi, E Koh, S Imanaka. Inverse relation between severity of psoriasis and serum 1,25-dihydroxyvitamin D level. J Dermatol Sci 1990. [Google Scholar] [Crossref]
- S Chaudhari, S Rathi. Correlation of serum calcium levels with severity of psoriasis. Int J Res Dermatol 2018. [Google Scholar] [Crossref]
- P. Gisondi, M. Rossini, A. Di Cesare, L. Idolazzi, S. Farina, G. Beltrami. Vitamin D status in patients with chronic plaque psoriasis. Br J Dermatol 2012. [Google Scholar] [Crossref]
- P B Nayak, B S Girisha, T M Noronha, H Sripathi. Low Vitamin D in psoriasis: Reality or myth?. Indian J Dermatol 2018. [Google Scholar]
- Z Zhai, L Chen, H Yang, J Yan, C Wang, J Yang. Can pretreatment serum calcium level predict the efficacy of methotrexate in the treatment of severe plaque psoriasis?. J Am Acad Dermatol 2015. [Google Scholar]
