- Visibility 1.5k Views
- Downloads 75 Downloads
- Permissions
- DOI 10.18231/j.ijced.2021.046
-
CrossMark
- Citation
Evaluation of facemask associated acne/ “Maskne” among health care workers and non-health care workers of India during COVID-19 pandemic-A cross-sectional study
- Author Details:
-
Savfeena M. Nagani
-
Aanal T. Patel
-
Nirav Bapat
-
Krina B Patel *
Abstract
Introduction: “MASK-NE”-Mask associated Acne, is a common form of acne during COVID-19 pandemic. It is type of acne mechanica seen when external factor occludes the skin, leads to irritation, inflammation and starts/aggravates all grades of acne.
Materials and Methods: We conducted a cross-sectional study among 773 participants, using a Self-administered, aim oriented, questionnaire which includes demographic data, acne related history, type and duration of wearing mask & other mask related skin problems in COVID-19 pandemic during 15th October to 15th December,2020.
Results: Among 773 participants, age ranged 18-45 years with mean 30.69 (SD: 61.30) and M:F was 1:1.78. After starting of Pandemic, occurrence of new development of mask associated Acne/ Maskne was higher among Health Care Workers (HCW) (34.98%) as compared to non- Health Care Workers (non-HCWs) (17.36%). Moreover, more number of HCWs had aggravation of their pre-existing acne and/or development of new of acne during pandemic (81.2%) than non-HCWs (61%). Wearing N95 type of mask showed the highest aggravation (82%) of Maskne as compare to wearing Surgical mask (75.5%) and wearing cloth (cotton) mask (65.6%).
Wearing a face mask for 4 to 8 hours/day and >8 hours/day showed increase in the aggravation of Maskne as compared to wearing a facemask <4 hrs/day.
Conclusion: Though wearing face masks can be the best strategy against COVID-19 infection, HAZARD OF THIS SAFETY is not negligible especially in front-line workers-doctors, nurses, pharmacist, policemen, hospital staff who are at higher risk due to several factors including type of mask use, duration of mask use etc.
Introduction
Corona virus (COVID‐19) pandemic is currently the most challenging threat to human health. Wearing a facemask is encouraged for preventing dispersal of droplets during talking, sneezing and coughing & therefore reduce the risk of environmental contamination by SARS‐CoV‐2 (COVID‐19). However, long‐time wearing of mask could lead to the flare of acne due to higher temperature and humidity on the surface of facial skin caused by expired air and the perspiration.[1], [2] Acne flare ups seen over the regions of the face covered with the masks are type of acne mechanica and is also called as “MASK-NE”.
Higher temperature has a close correlation with the flare of acne, which can be explained by the effect of temperature on the sebum excretion rate which is shown to increase by 10% for each 1°C rise and also there is higher quantity of sqaulene in surface lipid when temperature of skin increases underneath the mask.[3]
The ambient high humidity precipitates acne due to poral occlusive effect of skin hydration and irritation to the upper parts of pilosebaceous duct. In addition, sweat and increased humidity might cause swelling of epidermal keratinocytes, thus affecting the keratinocytes of pilosebaceous follicle and causing obstruction and aggravation.[4] The constant friction & continuous occlusion with mask can lead to comedones, papules, pustules & even cystic acne.
Moreover, changes in both surface sebum composition and skin hydration could contribute to disruption of skin barrier, leading to bacterial microflora imbalance and these all together will form a perfect Petridish for bacterial growth.
There were several reports of adverse skin reaction related to the personal protective equipment, for example mask, gloves, etc, during this pandemic.[5], [6], [7], [8], [9]
Summary of possible mechanisms for development of MASKNE has been sited in the[Figure 4]
The aim of the present study was to evaluate the occurrence of mask associated acne & aggravation of acne during this pandemic in HCWs and non-HCWs.
Materials and Methods
A cross sectional study was conducted by department of dermatology at tertiary care hospital of western India, between 15th October to 15th December 2020. The study was approved by Scientific & Ethics committee (Ref.: GMERSMCS/IEC/30/2020).
Participants above 18 years of age, both sexes and willing to participate and filled up questionnaire were enrolled in the study. Both HCWs as well as non-HCWs were included in the study.
A Self-administered, aim oriented, brief questionnaire which includes basic demographic data (age, sex,occupation), acne related history (aggravation, past history of acne), type of masks (N95, surgical, cloth mask), duration of wearing mask & other face mask related skin problems were used for the study. There were two different ways of filling the questionnaire as follows-
353 participants filled up the questionnaire in Out Patient Department (OPD) before consultation. All of them were evaluated for mask related side effects by consulting dermatologist. Out of which 113 Patients who had acne as per their responses and as observed by physician were included under OPD BASED study of acne and detailed history and examination regarding their grades of acne before and after pandemic were taken and photographs were taken.
Same questionnaire using live link Google form was sent via Whatsapp to HCWs and non-HCWs of Western India in equal proportion. Out of 420 responses received during stipulated time duration, 240 patients who had acne as per response received were included in the study.
New development of Mask associated acne, aggravation of pre-existing acne among HCWs and non-HCWs during pandemic was analyzed, variations in degree of aggravation of acne with different types of facemasks, variation in acne associated with duration of mask wearing and other skin problems because of regular wearing of facemasks were noted.
The collected data were analyzed using Microsoft excel;version 2010. Descriptive statistical methods, mean, standard deviations (SD), Confidence Interval(CI), Odds Ratio(OR), Chi square test, p value were used to analyze the demographic data.
Results
During the study period, 773 responses to self administered questionnaire were received. Age of the participants ranged from 18-45 years (Mean: 30.69; SD: 61.30) and M:F ratio 1:1.78.(M= 279, F=494) . 595(77%) responses were from HCWs and 178(23%) were from non-HCWs.
Among 595 HCWs, 132(22.18%) patient had already existing acne before pandemic, 162(27.22%) patients developed new onset of Acne and 301 responders (50.58%) had no Acne.
Among 178 non-HCWs, 34(19.10%) had preexisting acne, 25(14.04%) patients developed new onset of Acne, and 119 responders (66.85%) had no Acne.
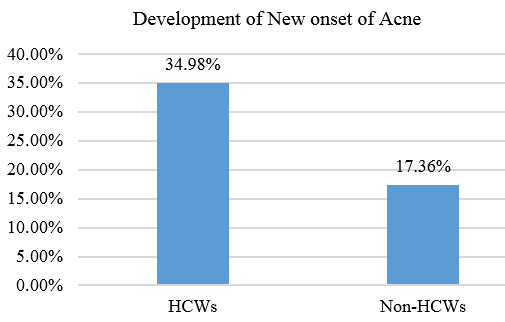
Analysis of participants showed that new onset of acne development was higher among HCW (34.98%) as compared to non-HCWs (17.36%). (OR 2.56; 95% CI -1.59 to 4.10; p value 0.0001)([Figure 1] )
Out of total 773 participants; 353 (45.66%) were found to have acne and they were further evaluated. Among 353 patients having acne, age of the patients ranged from 18-45 years (Mean: 31.58; SD: 73.32) and M:F ratio was 1:2.29.(M= 107, F=246). Out of 353 patients having acne, 113 (32%) were evaluated directly (OPD based survey) and 240(68%) were evaluated indirectly (via google form survey).
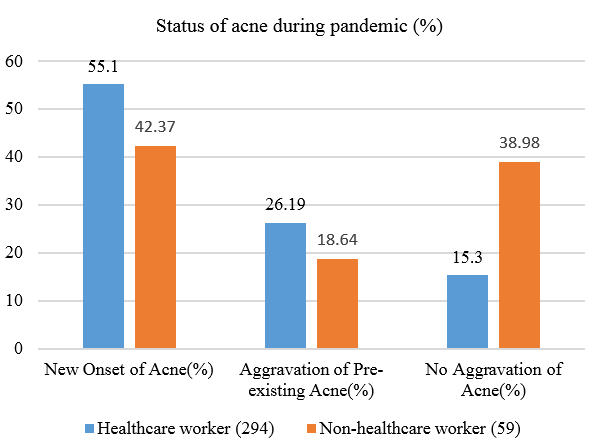
Among 353 patients of having acne; 294 (83.28%) were HCWs while 59 (16.72%) were non-HCWs. New onset of acne and/or aggravation of pre-existing acne was seen in 81.2% (N=239) of HCWs in comparison to 61%(N=36) of non-HCWs, which was statistically significant.(OR =2.77; 95% CI =1.52 to 5.07; p value 0.0008)
Among 294 HCWs, 162(55.1%) had new onset of acne, 77(26.19%) had aggravation of preexisting acne and 55(15.3%) had no change in their acne severity. While among 59 non- HCWs, 25(42.37%) had new onset of acne, 11(18.64%) had aggravation of preexisting acne and 23(38.98%) had no change in acne severity.([Figure 2])
Using different types of masks showed significant difference in regards to Maskne. Wearing N95 type of mask showed the highest aggravation of Acne (82%) as compare to wearing Surgical mask(75.5%) and wearing cloth/cotton mask(65.6%). (Chi-square=23.243, p value 0.0001)([Figure 3])
Increase in the duration of wearing mask also showed development of new onset of acne and/or aggravation of pre-existing acne. 65.5% of participants wearing mask for <4 hrs/day had acne aggravation, while 73.8% those who were wearing mask 4-8 hrs/day and 93.5% of those wearing mask for >8 hrs/day showed aggravation. ([Table 1])(Chi-square=24.78, p value 0.0001)
Among 113 patients of acne directly analyzed after filling up questionnaire, 71(62.8%) patients had showed new onset of acne only after starting of Pandemic([Table 2]). 28(24.8%) patients had preexisting acne which had worsened to higher grades due to wearing of facemask for prolonged period(Table 3). And rest of the 14(12.4%) participants did not change in their preexisting acne. Figure 2 shows images of patients with acne before and after staring of pandemic.
We also observed that development of maskne was only over particular areas of face like bilateral cheeks, chin, perioral, nose, mandibular margin, upper part of neck as compared to forehead, upper trunk and arms.([Figure 6]).
During the study, facemask associated other cutaneous problems observed were itching, darkening of the skin, redness, burning sensations over face, folliculitis, dermatophytic infection, warts etc.
Summary of all the statistical analysis have been given in the [Table 4]; which shows that all the data are statistically significant and there was definite association of maskne due to face mask.
|
Duration of wearing mask |
Total number of participants wearing mask |
Aggravation of acne on wearing mask (i.e. maskne) |
|
<4 hrs |
87 |
57(65.50%) |
|
4-8 hrs |
157 |
116(73.80%) |
|
>8 hrs |
109 |
102(93.50%) |
Increase in the duration of wearing mask also showed increased occurrence of MASKNE. Wearing mask for <4 hrs/day showed 65.50% (57/87) aggravation, those who were wearing mask 4-8 hrs/day showed 73.80%(116/157) and >8 hrs/day showed 93.50%(102/109) aggravation. Wearing a face mask for 4 to 8 hours/day and >8 hours/day showed increase in the aggravation of Maskne as compared to wearing a facemask <4 hrs/day. ([Table 1])
|
Types of acne (Grade) |
No. of patients |
|
Comedones (Grade-1) |
26(36.61%) |
|
Papules (Grade-2) |
18(25.35%) |
|
Pustules (Grade-3) |
13(18.31%) |
|
Nodulocystic (Grade-4) |
14(19.71%) |
|
|
Types of acne ( Grade) |
|
|
No. of patients (n) |
Before pandemic |
After pandemic |
|
15(53.57%) |
Comedones Grade-1 |
Papules,pustules Grade-2 |
|
7(25%) |
Papules Grade-2 |
Nodules GRADE-4 |
|
6(21.43%) |
Post acne scars |
Nodulo-cystic GRADE-4 |
As per OPD based study of 113 patients of acne, 71(62.8%) patients had new onset of acne only after starting of Pandemic. ([Table 2]). 28(24.8%) patients had preexisting acne which had worsened due to wearing of facemask for prolonged period. ([Table 3]) And rest of the 14(12.4%) participants did not feel aggravation of the acne.
71 patients did not have Acne before stating of the Pandemic. Out of them, 26(36.61%) patients developed Grade 1 Acne Vulgaris, 18(25.35%) patients developed Grade 2 Acne Vulgaris, 13(18.31%) Patients developed Grade 3 Acne Vulgaris and 14(19.71%) patients developed Grade 4 Acne Vulgaris after starting of the Pandemic.
Out of these 28 patients, 15(53.57%) patients were in Grade 1 Acne Vulgaris; and after starting of the Pandemic the Acne worsened and they developed Grade 2 Acne Vulgaris. Similarly 7(25%) patients were in Grade 2 Acne vulgaris, and 6(21.43%) patients had only Post Acne Scars, all these patients worsened and developed Grade 4 Acne vulgaris. ([Table 2])
|
|
n (%) of patients |
Statistical analysis |
|
New Onset of Acne |
|
OR 2.56; 95% CI -1.59 to 4.10; p value 0.0001 |
|
HCWs |
162(34.98.%) |
|
|
Non-HCWs |
25(17.36%) |
|
|
Aggravation of pre-existing Acne progressing to higher grades |
|
OR =2.77; 95% CI =1.52 to 5.07; p value 0.0008 |
|
HCW |
239(81.29%) |
|
|
Non-HCWs |
36(61.01%) |
|
|
Different types of Facemask and association of Aggravation of Acne |
|
Chi-square=23.243; p value 0.0001 |
|
N95 Mask |
196(82.00%) |
|
|
Surgical Mask |
37(75.51%) |
|
|
Cotton Mask |
42(65.62%) |
|
|
Duration of Wearing Mask |
|
Chi-square=24.78; p value=0.0001 |
|
<4 hrs |
57(65.50%) |
|
|
4-8 hrs |
116(73.80%) |
|
|
>8 hrs |
102(93.50%) |




Discussion
COVID-19 pandemic has affected human population through-out the world. The recommendation for wearing the hygienic mask in general use was announced in India as a manner to prevent spreading of the virus during the pandemic since the end of March 2020.
In dermatology practice, it was noticed that there were some episodic adverse skin reactions related to facemask wearing in the HCWs as well as non-HCWs. In particular worsening of acne was noticed during this period. This became an objective of our study. This study was aimed to focus in both HCWs and non-HCWs because its effects are not only on HCW, as reported in similar previous pandemic diseases[1] but also on the general population.
A recent publication about the effects of facemask on the skin underneath-surveyed during COVID-19 pandemic in Thailand by Techasatian et al reported an occurrence of acne as high as 39.9%, [10] in our study we found the same to be 34.98% in HCWs and 17.36% in non-HCWs. The study by Techasatian et al, focused on the effects of the mask related adverse reactions on face. Whereas, our study was aimed to explore face mask related acne in-depth including the grades of acne, aggravation of pre-existing acne and development of new onset of acne among HCWs and non-HCWs.
In our study, use of N95 mask showed the highest aggravation of Acne followed by use of Surgical mask and cloth mask. Whereas Techasatian et al study showed that Surgical masks had a higher risk of adverse skin reaction compared to cloth masks. There was a way of making a cloth cover on top of a surgical mask (surgical mask covered by a piece of cloth) in Thailand. This method showed a higher risk of adverse skin reaction compared to cloth masks, however, the risk was still less than the group with surgical masks.[10] It suggests that there were significant association between type of masks used and development of acne & other face mask related side effects.
Increase in the duration of wearing mask for >4 hrs/day has showed increased occurrence of MASKNE in our the study as well as Techasatian et al study.
A study of two women HCWs conducted in 2003 by Kian Teo Tan et al[11] in Singapore showed acne outbreaks associated with use of N95 masks continuously for about 3 months. Both patients had nodular acne in similar distribution over cheeks,chin , perioral area as seen in our study. [12] In our study development of new onset of acne and aggravation of preexisting acne were observed in both the groups; but it was higher among HCWs as compared to non-HCWs and was also confirmed by OPD based(direct) survey.
It was not possible to evaluate the grades of acne through google form survey but this limitation was partially compensated by our OPD based survey where patients were directly analyzed after filling up form.
Other aggravating/confounding factors like Stress/Anxiety among the Healthcare workers was not analyzed in the study.
Conclusion
Although Wearing face masks can be the best strategy against COVID-19 infection, HAZARD OF THIS SAFETY is not negligible especially in front-line workers who are at higher risk of maskne and other mask associated cutaneous disorders because of their tighter fitting masks & wearing it for longer duration. As lower risk of maskne was found to be associated with cloth mask as compared to N-95 mask, special fabric use for mask with better protection may be explored for future use.
Source of Funding
No external funding was received to carry out this work.
Conflict of Interest
None.
References
- Foo CC, Goon AT, Leow YH, Goh CL. Adverse skin reactions to personal protective equipment against severe acute respiratory syndrome--a descriptive study in Singapore. Contact Dermatitis. 2006;55(5):291-4. [Google Scholar]
- Gheisari M, Araghi F, Moravvej H, Tabary M, Dadkhahfar S. Skin reactions to non-glove personal protective equipment: an emerging issue in the COVID-19 pandemic. J Eur Acad Dermatol Venereol. 2020;34(7):297-8. [Google Scholar]
- Narang I, Sardana K, Bajpai R, Garg VK. Seasonal aggravation of acne in summers and the effect of temperature and humidity in a study in a tropical setting. J Cosmet Dermatol. 2019;18(4):1098-104. [Google Scholar]
- Sardana K, Sharma RC, Sarkar R. Seasonal variation in acne vulgaris--myth or reality. J Dermatol. 2002;29(8):484-8. [Google Scholar]
- Desai SR, Kovarik C, Brod B. COVID-19 and personal protective equipment: Treatment and prevention of skin conditions related to the occupational use of personal protective equipment. J Am Acad Dermatol. 2020;83(2):675-7. [Google Scholar]
- Payne A. Covid-19: skin damage with prolonged wear of FFP3 masks. BMJ. 2020;369. [Google Scholar] [Crossref]
- Chowdhury MM, Bevan N, Ryan K. Covid-19: virtual occupational skin health clinics for healthcare workers. BMJ. 2020;369. [Google Scholar] [Crossref]
- Hadjieconomou S, Hughes J, Kamath S. Occupational skin disease during the COVID-19 pandemic, as captured in a Dermatology staff clinic in the United Kingdom. J Eur Acad Dermatol Venereol. 2020;34(11):670-1. [Google Scholar]
- Lan J, Song Z, Miao X. Skin damage among health care workers managing coronavirus disease-2019. J Am Acad Dermatol. 2020;82:1215-6. [Google Scholar]
- Techasatian L, Lebsing S, Uppala R, Thaowandee W, Chaiyarit J, Supakunpinyo C. The Effects of the Face Mask on the Skin Underneath: A Prospective Survey During the COVID-19 Pandemic. J Prim Care Community Health. 2020;11. [Google Scholar] [Crossref]
- Tan KT, Greaves MW. N95 acne. Int J Dermatol. 2004;43(7):522-3. [Google Scholar]
- Tzeng HM. Fighting the SARS epidemic in Taiwan: a nursing perspective. J Nurs Adm. 2003;33(11):565-7. [Google Scholar]
How to Cite This Article
Vancouver
Nagani SM, Patel AT, Bapat N, Patel KB. Evaluation of facemask associated acne/ “Maskne” among health care workers and non-health care workers of India during COVID-19 pandemic-A cross-sectional study [Internet]. IP Indian J Clin Exp Dermatol. 2021 [cited 2025 Nov 04];7(3):243-248. Available from: https://doi.org/10.18231/j.ijced.2021.046
APA
Nagani, S. M., Patel, A. T., Bapat, N., Patel, K. B. (2021). Evaluation of facemask associated acne/ “Maskne” among health care workers and non-health care workers of India during COVID-19 pandemic-A cross-sectional study. IP Indian J Clin Exp Dermatol, 7(3), 243-248. https://doi.org/10.18231/j.ijced.2021.046
MLA
Nagani, Savfeena M., Patel, Aanal T., Bapat, Nirav, Patel, Krina B. "Evaluation of facemask associated acne/ “Maskne” among health care workers and non-health care workers of India during COVID-19 pandemic-A cross-sectional study." IP Indian J Clin Exp Dermatol, vol. 7, no. 3, 2021, pp. 243-248. https://doi.org/10.18231/j.ijced.2021.046
Chicago
Nagani, S. M., Patel, A. T., Bapat, N., Patel, K. B.. "Evaluation of facemask associated acne/ “Maskne” among health care workers and non-health care workers of India during COVID-19 pandemic-A cross-sectional study." IP Indian J Clin Exp Dermatol 7, no. 3 (2021): 243-248. https://doi.org/10.18231/j.ijced.2021.046
