- Visibility 127 Views
- Downloads 6 Downloads
- DOI 10.18231/j.ijced.2021.061
-
CrossMark
- Citation
Assessment of clinical and etiological factors in nail dyschromias
- Author Details:
-
Lalitha C
-
Shwetha S *
-
Asha G S
Introduction
Nail abnormalities can be a revealing sign of a systemic disease. Nail dyschromia or chromonychia is defined as an abnormality in the color of the substance or the surface of the nail plate or subungual tissue.[1] The discoloration specifically due to the deposition of melanin is labeled as nail pigmentation.[1] Melanonychia, as a variant, is defined as brown or black pigmentation of nails.[1], [2]
Nails of both limbs should be always examined in totality apart from the affected nail, preferably prior to the examination of the affected nail to avoid bias. However, prior to this, a detailed history is necessary, especially to rule out presence of any exogenously added pigmentation of the nail (e.g. Henna). When the discoloration is secondary to exogenous agents, the pattern lies along the curve of the proximal nail fold; if internal, follows the curve of the lunula.[2]
A working anatomical knowledge of the nail, its attachments and the underlying tissues is imperative to analyze the factors that cause discoloration of an otherwise transparent nail.[1] A systemic disease can affect one or all nails simultaneously, but a localized affect can alter the colour of the one or two nails maximally, limiting the involvement.[2] In addition, a quick but thorough cutaneous and mucosal examination is desired as these may many a times provide an important clue to an underlying disease. Few morphological changes might occur otherwise in an apparently normal healthy individual. An idea of this may help avert unnecessary work up in these individuals. [3]
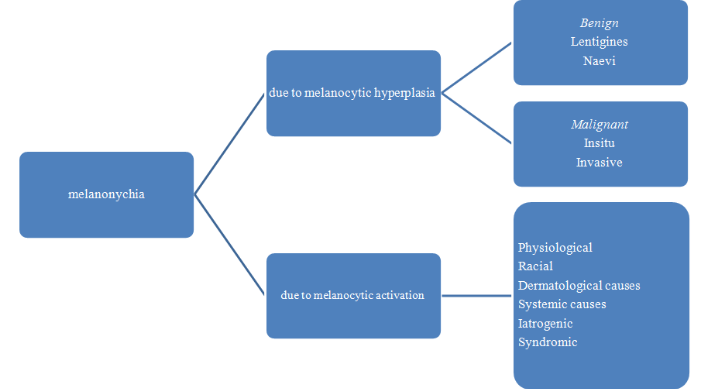
There can be several causes of Melanonychia, a brief description of which is mentioned in [Figure 1].
Materials and Methods
The aim of the study is to find out the different causes of nail dyschromias. It was a cross sectional study done from April 2015 to July 2015 at tertiary hospital in Bangalore. 200 patients above the age of 18 years, presenting with nail discoloration were included in the study. A detailed history including occupation, hobbies, and illnesses (systemic and dermatological), medications, past treatments, family history, trauma to the nail, type of footwear, manicure and pedicure treatment was noted in a semi structured pro forma.
Routine blood investigations like Complete hemogram with peripheral smear, Liver function test, renal function test, Random blood sugar, ELISA for HIV 1 & 2, Serum Vitamin B12 were done. Wherever deemed necessary, a nail biopsy and scrapings was performed.
The data was then entered in an MS excel spreadsheet. The statistical analysis was done using SPSS v21. The categorical data was represented as frequencies and proportions, while the quantitative data was represented as mean, median and IQR.
Results
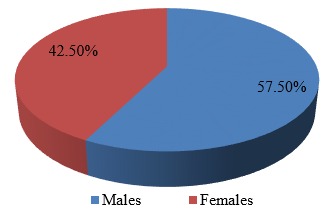
115 (57.5%) were males and 85 (42.05%) were females ([Figure 22]).
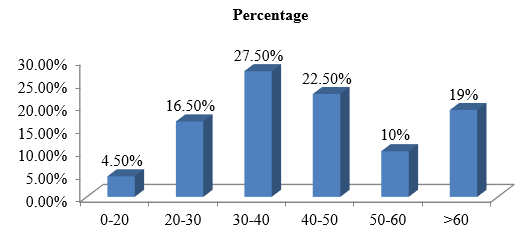
More than 50% patients were in the age group between 30 to 50 years ([Figure 23]).
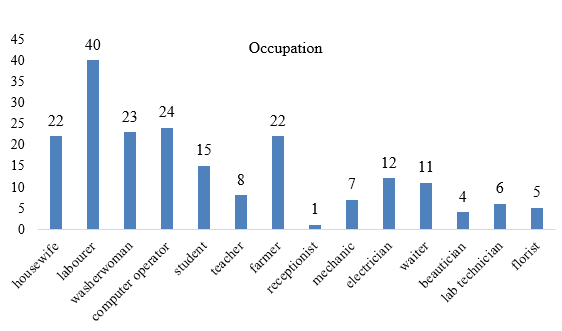
Laborers constituted the highest portion amongst the study participants, followed closely by computer operators.([Figure 24])
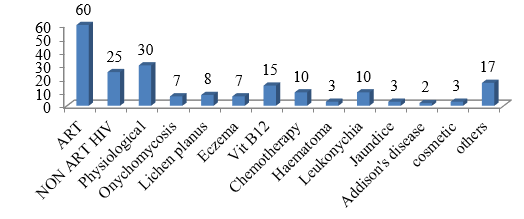
On analysis of the lab parameter, 22.5% participants had Hb less than 8 gm/dL. 12.3% of the study participants had serum creatinine more than 2.0 mg/L. Deranged liver function was observed in 12.45% participants. ELISA done for HIV I and II was reactive in 48.02% of the study participants with melanonychia. Vitamin B12 deficiency was observed in 14.12% of the study participants with melanonychia ([Figure 25]).
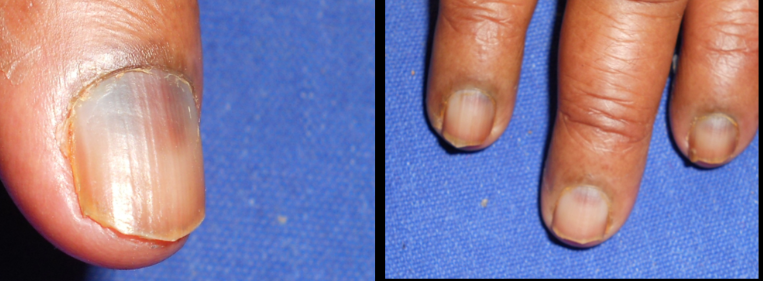
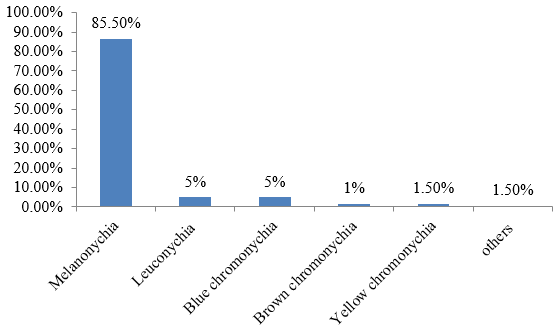
The most seen nail dyschromia in this study was melanonychia (86.5%) followed by leukonychia (5%), blue chromonychia (5%), yellow chromonychia (1.5%) and 0.5% of other color chromonychia (orange exogenous henna nail discoloration and one green nail associated with). Longitudinal Melanonychia, was the most seen, transverse, and subtotal melanonychia were seen in few cases ([Figure 26]). It involved both fingernails and toenails (fingernails> toenails). In fingernails, it was seen more in thumbnails and index and middle fingers and in toe nails, Great toe nail involvement was observed. The different types of nail dyschromias photographs are shown in figures ([Figure 2], [Figure 3], [Figure 4], [Figure 5], [Figure 6], [Figure 7], [Figure 8], [Figure 9], [Figure 10], [Figure 11], [Figure 12], [Figure 13], [Figure 14], [Figure 15], [Figure 16], [Figure 17], [Figure 18], [Figure 19], [Figure 20], [Figure 21]).



















Discussion
Nail dyschromias as a common disorder encountered by dermatologists, even general practitioners, on a day-to-day basis. This is secondary to pigmentation of the nail bed or plate and can be attributed to various endogenous (localized or systemic) or exogenous causes. The type of the nail dyschromia depends on the pigment deposited, the region and its duration.
In this study, majority of the patients belonged to the age brackets of 30-50 years. This was like the findings in a study done by Soo Hyeon Bae et al, the mean age was 43.6 ± 23.8 years. 57.5% of the patients were male, which was like the findings by Soo Hyeon Bae et al.[4]
Hobbies play an important role in the identification of the cause of nail dyschromia, as they contribute as an exogenous factor. In our study, we found that sports was the most common hobby amongst the study participants. This was like the findings in a study done by Yildirimer L et al,[5] where injuries due to sports related trauma (crush injuries) was a leading cause of nail dyschromia.
Anaemia is one of the causes of apparent leukonychia, a cause of nail dyschromia. In our study we found that 22.5% patients had anaemia. In a study by Braun et al, [6] anaemia was observed in those with leukonychia, due to blanching of the nail bed. In a study done by Soo Hyeon Bae et al, [4] incidence of anaemia was 38.5%. Half and half nails can be seen with those with deranged liver function, however in this study we didn’t report any such case in those patients with raised bilirubin. Chronic renal failure can also cause nail dyschromias, in this study 12.3% participants had raised serum creatinine. In a study done by Soo Hyeon Bae et al, [4] 15.4% patients had chronic renal failure.
Melanonychia was the most common dyschromia (85.5%) seen in this study. In the present study, drug induced and systemic infection like HIV contributed largely to melanonychia whereas local and dermatological conditions contributed to few. This is in accordance with other studies done on nail pigmentations.
Among the drug induced, 30% were due to antiretroviral drugs like zidovudine, lamivudine, others were due chemotherapatic agents and antimalarials. This can be attributed to the cause that our institute was referral centre for HIV and ART centre. In this study, we did not find any subungual melanoma or naevus or wart presenting with melanonychia. However, in a study done by Soo Hyeon Bae et al, 33.3% patients had naevus of the nail matrix.
In this, we observed 10 cases (5%) of blue nails, which was due to chemotherapeutic medication like doxorubicin, cyclophosphamide and antimalarials. In a study done by Soo Hyeon Bae et al, blue nails was seen only in a small percentage of the study population (1.3%). In a study done by P F Levey and team [7] in Africans, they found that HIV infection and the treatment is a cause for blue nails. Yellow discoloration of nails (5 in number) was seen in 2 cases of onychomycosis and in 3 cases of jaundice due to liver disorder. In a study by Brzeziński P et al,[8] the cause of the yellow nail discoloration was due to chronic pulmonary disease. Similar findings were recorded by Piraccini and team.[9] We found one case each on longitudinal erythronychia in Darier’s disease, green nails due to pseudomonas infection and orange discoloration of nails due to henna.
Conclusion
Nail being a small apparatus can reveal underlying systemic or local disorders. It’s important to examine nail routinely and worked up with detailed history and investigations
Conflicts of Interest
The authors declare that there are no conflicts of interest regarding the publication of this paper.
Source of Funding
None.
References
- M Jeanmougin, J Civatte. Nail Dyschromia. Int J Dermatol 1983. [Google Scholar]
- V Mendiratta, A Jain, Nail. Symposium-Nails Part I. Indian J Dermatol Venereol Leprol 2011. [Google Scholar] [Crossref]
- R Baran, R P Dawber, R Baran, RP Dawber, E Hanche. Physical science. Diseases of the nail and its management 2001. [Google Scholar]
- SH Bae, SH Jang, YH Won. Twenty-Nail Dystrophy Treated with Hydroxychloroquine in a Patient with Alopecia Areata. Ann Dermatol 2019. [Google Scholar] [Crossref]
- L Yildirimer. Experience of nail bed injuries at a tertiary hand trauma unit: A 12-month review and cost analysis. J Hand Surg 2019. [Google Scholar] [Crossref]
- R P Braun, R Baran, F A Le Gal, S Dalle, S Ronger, R Pandolfi. Diagnosis and management of nail pigmentation. J Am Acad Dermatol 2007. [Google Scholar] [Crossref]
- P F Levay, M E Botes, E Malela. Dyschromonychia: clinical significance in a South African population. SA Fam Pract 2005. [Google Scholar]
- P Brzeziński, M Bury, E Jagiełło-Wieczorek. Coexistence yellow nail syndrome with systemic symptoms. N Dermatol Online 2010. [Google Scholar]
- B M Piraccini, B Urciuoli, M Starace, A Tosti, R Balestri. Yellow nail syndrome: Clinical experience in a series of 21 patients. J Dtsch Dermatol Ges 2014. [Google Scholar]
