- Visibility 79 Views
- Downloads 14 Downloads
- DOI 10.18231/j.ijced.2022.024
-
CrossMark
- Citation
A study of Mucocutaneous Manifestations of HIV infections & its relation with CD4 Count
- Author Details:
-
Rajesh Velagam
-
Raghupati Reddy
-
G N R Netha
-
T Satyasri *
Introduction
HIV/AIDS occurrence is a major health problem facing all countries in the world. Dermatological involvement in AIDS has been appreciated since the disease was first recognized as a cryptic acquired immune deficiency illness in homosexual men and before the causative virus was identified. HIV has been demonstrated in the dermis of infected individuals and may be present in langerhans cells.[1] It is estimated that more than 90% of HIV- infected patients develop skin or mucous membrane disorders at some time during their infection.[2] The knowledge of skin manifestations such as bacillary angiomatosis, Kaposi‘s sarcoma, oral candidiasis and hairy leukoplakia, may provide a clue for diagnosing a previously undetected HIV positive status. In HIV- infected patients, some skin manifestations, including skin infections, are frequently used as indicators for patients immunological status, especially in the setting where testing for CD4+ cell count and HIV-1 RNA viral load cannot be performed regularly.
HIV1 infection now represents a global pandemic. If an average figure is taken, this comes to 2.5 million living with HIV and AIDS. More men are HIV positive than women. Nationally, the prevalence rate for adult females is 0.29 percent, while for males it is 0.43 percent. Prevalence is also high in the 15-49 age group (88.7 percent of all infections), indicating that AIDS still threatens the cream of society, those in the prime of their working life. [3]
Aim of the Study
To study mucocutaneous manifestations of HIV infection and its relation to CD4 count.
Materials and Methods
This is a prospective and observational study, carried out in the departments of Dermatology Venereology and Leprosy, at Gandhi medical college, secunderabad, Telangana.
Inclusion criteria
Patients whose HIV status has been proved by NACO guidelines.
HIV/AIDS patients with symptoms and signs suggested of dermatological diseases.
Exclusion criteria
Pregnant women & lactating mothers with HIV/AIDS.
Children below 18 years.
After getting ethical committee approval, one hundred (100) patients attending STI OPD at Gandhi medical college / Gandhi Hospital having mucocutaneous manifestations and who were tested HIV Antibodies positive at ICTC according to NACO guidelines were taken up for the study. A detailed history was taken in each case with special attention to sexually transmitted diseases (past or present), skin lesions, mucosal lesions were elicited in every case. Cases were thoroughly examined with regards to involvement of skin, scalp, hair, nail, oral and genital mucosa, lymph glands and other symptoms.
All routine investigations like hemoglobin, total count, differential count, erythrocyte sedimentation rate, urine albumin, sugar and micro, baseline weight, X-ray chest PA view, VDRL, HBsAg, Mantoux test, ultrasonography of abdomen were done in all cases. In cases with doubtful clinical diagnosis of skin disorder, skin biopsies were taken for histopathological examination and also relevant laboratory test like KOH, Tzanck test, ANA, Anti ds DNA, Anti histone antibodies were performed. The CD4 counts were estimated in all cases by flow cytometry (gold standard for CD4 T lymphocytes measurements). Patients were treated accordingly.
Results
Age distribution
In the present study, most common age group affected was 19-29 (36%), followed by 30-39 years (29%), followed by 40-49 years (26%), 50-59 years (7%), and 60-69 years (1%) with a mean age of 29.25 years.[Table 1]
|
Age |
Males |
Females |
Total |
|
19- 29yr |
22 |
14 |
36(36%) |
|
30-39yr |
18 |
11 |
29(29%) |
|
40-49yr |
16 |
10 |
26(26%) |
|
50-59yr |
05 |
02 |
07(07%) |
|
60-69yr |
01 |
00 |
01(01%) |
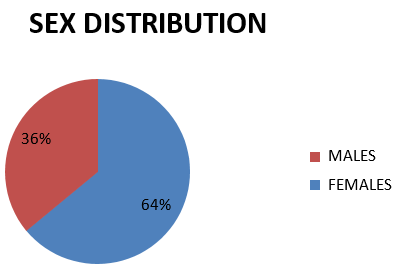
Sex distribution
In the present study, out of 100, 64% (64) were male and 36%(36) were female with a male to female ratio of 1.8:1.[Figure 1]
Infectious mucocutaneous manifestations and CD4 count
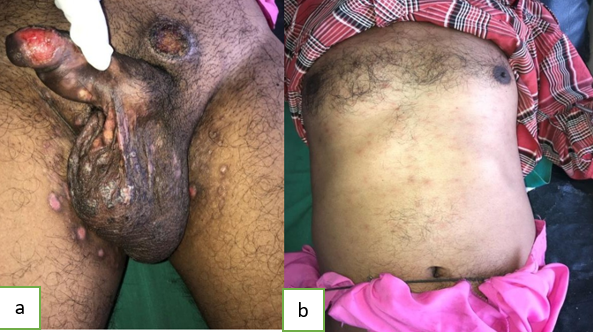
The dermatological diseases were classified according to causes, into infectious & noninfectious. In the infectious group, the most common cutaneous disease was viral including herpes zoster (11,11%), with mean CD4 count 196 cells/ul followed byherpes simplex molluscum contagiousm, warts. The second most common infection was fungal infection including oral candidiasis (12, 12%) with mean CD4 count 261cells /ul, followed by tineacorporis, tineacruris. Tineafaciei and tineaversicolor. Among bacterial infection, Furunculosis followed by folliculitis but other bacterial infection, impetigo were less common. 4 (4%) cases presented with scabies with mean CD4 count 316 cells/ul. [Table 2]
|
Diagnosis |
Total no. of patients (78) |
Percentage of patients |
Mean CD4 Counts (cells/ul) |
CD4 cells count range (cells/ul) |
|
Viral infections |
28 |
28 |
276.75 |
14-821 |
|
Herpes Zoster |
11 |
11 |
196.45 |
24-381 |
|
Herpes simplex |
8 |
8 |
284.37 |
14-650 |
|
Warts |
5 |
5 |
334.5 |
38-701 |
|
Molluscumcontagiousum |
4 |
4 |
493.75 |
177-821 |
|
Fungal & yeast |
26 |
26 |
268.11 |
05-992 |
|
Oral candidiasis |
12 |
12 |
261.58 |
05-488 |
|
T.Corporis |
8 |
8 |
263.87 |
52-721 |
|
T. Cruris |
4 |
4 |
292 |
52-392 |
|
T.Faciei |
1 |
1 |
254 |
254 |
|
T.Versicolor |
1 |
1 |
299 |
299 |
|
Bacterial infection |
17 |
|
|
19-843 |
|
Furunculosis |
7 |
7 |
222.7 |
40-843 |
|
Folliculitis |
5 |
5 |
255.57 |
19-702 |
|
Leprosy |
1 |
1 |
154 |
154 |
|
Impetigo |
1 |
1 |
164 |
164 |
|
Ecthyma |
1 |
1 |
287 |
287 |
|
Cellulitis |
1 |
1 |
179 |
179 |
|
Cutaneous Tuberculosis |
1 |
1 |
367 |
367 |
|
Other infections |
|
|
|
|
|
Scabies |
4 |
4 |
316 |
33-473 |
|
Syphilis |
2 |
2 |
385 |
176,600 |
|
Lymphogranulomavenereum |
1 |
1 |
278 |
278 |
Mucocutaneous manifestations and immune categories
Out of 28 patients with viral infections, 3%(3) of patients were under C1 category,12% (12) of patients were under C2 category, and 12% (12) of patients were under C3 category. Out of 26 patients with fungal and yeast infections 1%(1) patient under C1 category, 13%(13) patients under C2 category, and 12(12%) patients were under C3 category. Out of 17 patients with bacterial infections, 2% (2) patients were under C1 category, 4%(4) patients were under C2 category, 11%(11) patients were under C3 category. Out of 4 patients 3%(3) patients were under C3 category, 1% (1) patients were under C1 category.
Non- infectious mucocutaneous manifestations and CD4 cell count
In the non- infectious group, pruritic popular eruptions (PPE) (9%,9) with mean CD4 count of 232 cells/ul, was most common cutaneous findings among HIV positive patients followed by drug reactions (7%, 7) with mean CD4 count of 113 cells/ul. Other noninfectious dermatological diseases included Eczema (3%,3,232), psoriasis (2%,2,222), seborrheic dermatitis (2%,2,328), photosensitive dermatitis (1%,1,223), LPP, SLE, Acne were less common.[Table 3]
|
Diagnosis |
Total No. patients (28) |
% |
MeanCD4 Count(cells/ul) |
CD4 count rang (cells/ul) |
|
PPD |
09 |
9 |
234.33 |
31-571 |
|
Drug Reactions |
07 |
7 |
113 |
26-259 |
|
MPR |
02 |
2 |
74.5 |
35,114 |
|
SJS |
03 |
3 |
148 |
37,259 |
|
TEN |
01 |
1 |
98 |
98 |
|
EMF |
01 |
1 |
26 |
26 |
|
FDE |
01 |
1 |
222 |
222 |
|
Eczema |
03 |
3 |
232.33 |
114,310 |
|
psoriasis |
02 |
2 |
222.53 |
46,401 |
|
Seborrhoeic dermatitis |
02 |
2 |
328.5 |
284,373 |
|
Photosensitive dermatitis |
01 |
1 |
223 |
223 |
|
LSC |
01 |
1 |
160 |
160 |
|
SLE |
01 |
1 |
150 |
150 |
|
Acne |
01 |
1 |
268 |
268 |
|
LPP |
01 |
1 |
392 |
392 |
Non infectious mucocutaneous manifestations and immune categories
A total 9 patients developed PPD, of which 1%(1) of patients were under category 1, 2%(2) of patients were under category 2 and 6%(6) of patients were under immune category 3. Drug reactions were developed in 7 patients and of these, 2%(2) of patients were observed under immune category 2, 5%(5) of patients were observed immune category 3.
Immune categories
In the present study, out of 100, fifty (50,50%) patients had CD4 counts below 200 cells/ul and, of these 19 patients had CD4 counts below 50 cells/ul. Forty four (44,44%) patients had counts between 200-499 cells/ul and six (6,6%0 patients had above 500cells/ul.



Discussion
Skin disorders are frequent among persons infected with HIV. In many cases, skin disease is the first manifestation of HIV infection and serves as an early indicator of clinical T- cell deficiency. The frequent finding of cutaneous disorders in HIV infected individuals is due to the fact the skin itself is an immune system containing antigen presenting cells. There evidence that the number of Langerhan cells are decreased in AIDS because they are also targets of HIV infection.
Age group
The common age group affected in the present study was 19-29 years. Kviarasan etet [3] and Shobhana A et al [4] have also reported the same age group (21-30 years) involvement in their study. Mean age in the present 30.21 years which is comparable with studies by Kaviarasan et al and Shobhana A et al who have reported 30.7 years and 29 years as mean in their studies respectively.
Sex
In the present study 64% (64) males and 36% (36) females were affected with male to female ratio of 1.8:1. The male preponderance in the present study is comparable with studies of Kaviarasan et al (3:1), Shobhana et al (2.5:1) and Goh et al [5](8.5:1). Supanaranond W et al also reported males were affected more than female in their study years. Kviarasan et al and Shobhana A et al have also reported the same age group (21-30 years) involvement in their study. Mean age in the present 30.21 years which is comparable with studies by Kaviarasan et al and Shobhana A et al who have reported 30.7 years and 29 years as mean in their studies respectively. However Goh et al have reported higher mean age (40.2yrs) in their study. Singh H, et al have also reported higher mean age 30-39 years in their study.
Mucocutaneous Manifestations and CD4 Cell Count
Infectious mucocutaneous manifestations and CD4 count
The dermatological disease were classified into infectious & and non infectious. The infectious diseases were the largest category of cutaneous disorders associated with HIV infection.
In the present study, the most common infectious cutaneous disease was viral infection. Out of 100 patients, 28% (28) patients had viral infections. Among the viral infections herpes zoster was the commonest infection 11%. However Shobhana et al reported herpes zoster only in 6% HIV patients in their study. Where as Naburi AE, et al reported herpes zoster in as high as 25% HIV patients. [6]
In the present study, CD4 range among herpes zoster patients between 24-381 cells/ul which is comparable with the study by Shobhana et al who have reported CD4 range between 20- 659 cells/µl among herpes zoster patients. In the present study among herpes zoster patients, 6% had below 200 cells/µl while 5 % had CD4 counts above 200 cells/µl. This is comparable with study by Goh et al who have reported CD4 counts below 200 cells/µl in 9.6% of patients and above 200 cells/µl in 4.1% of patients. However zancanaro et al [7] reported 1.8% with CD4 counts below 200 cells/µl and 0.4% with CD4 counts above 200 cells/µl.
CD4 range among herpes simplex patients recorded on the present study range between 14-650 cells/ul which is comparable with the CD4 range reported by Shobhana et al ( 33- 672 cells/ul).
In the present study, 4% (4) patients had molluscum contagiosum, warts were noted in 5% (5) patients with CD4 range between 38-701 which is comparable which is consistent with the study by Shobhana et al.
Fungal infections are an early manifestation of immunosuppression and they are more frequent when the CD4 cell count approaches 450 cells/μL. [8]
The second commonest dermatological disease among infections in the present study was fungal infections (26%). Out of the 100 patients, 14% (14) patients had dermatophytosis. This finding is comparable with the studies of Shobhana et al and Kumaraswamy et al[9] who reported 13% and 8% patients with dermatophytosis respectively.
Other dermatophyte infections observed in this study were tineacruris 4%, and tineafaciei 1%, and tineafaciei in 14.6%. & dermatophytic infections like T.corporis (8,8%), T.Versicolor(1,1%) were less commonly noted in our present study.
Oral candidiasis have been reported as the most common dermatological disorders among HIV patients in various studies in the past decade.
In the present study oral candidiasis was observed in 12% (12) patients. This low proportion of oral candidiasis in the present study could be partially explained by the fact that HIV positive patients only with oral candidiasis were referred to gastroenterology OPD directly.
CD4 count among oral candidiasis patients range between 5-488 cells/ul which is comparable with CD4 range in study by Shobhana et al (17-551 cells/ul). In the present study 6 % HIV positive patients with oral candidiasis had CD4 count below 200 cells/µl and 6% had CD4 counts above 200 cells/ul.
In the present study bacterial infections accounted for 17% (17) of patients. Bacterial infections like Furunculosis (7, 7%), Folliculitis (5, 5%), leprosy (1, 1%), Impetigo (1,1%), Ecthyma (1, 1%), were less commonly noted.
Therapy with septran in all HIV positive patients to prevent opportunistic infections could be responsible for the less number of cases of bacterial infections in the present study.
In the present study, 4% (4) patients presented with scabies which is comparable with study by Shobhana et al who have reported scabies in 5% patients. In the present study 2% scabies patients had CD4 counts below 200 cells /ul and 2% patients had CD4 counts above 200 cells/ul. Farrokh et al reported 4.1% patients with CD4 counts below 200 cells/ul.
Non Infectious mucocutaneous manifestations and CD4 cell count
In the present study, the most common noninfectious mucocuatneous manifestation was pruritic popular eruption, observed in 9% (9) patients. This is similar to the studies by Kumaraswamy et al (7.7%) and Maniar et al (4.8%).
In the present study, CD4 range among pruritic popular eruption patients between 31-571 cells/ul.
In the present study, 6% (6) of pruritic popular eruption patients had CD4 counts below 200 CD4 cells/ul and 2% (2) of patients had cd4 counts above 200 cells/ul.
In the present study, drug reaction 7% (7), was the next common dermatological manifestation among noninfectious group
In the present study 5% (5) of patients with drug reaction had CD4 counts below 200cells/ul and 2% (2) of patients had CD4 counts above 200 cells/ul
In the present study out of 7% (7) of patients with drug reactions 2% (2) of patients had maculopapular drug rash followed by other drug reaction like SJS(3,3%), TEN(1,1%), EMF(1,1%), FDE(1,1%).
Other non-infectious disease included eczema (3%,3,232 ), psoriasis (2%,2,223),seborrheic dermatitis (2%,2,328), photosensitive dermatitis (1%,1,223), LSC (1%,1,160),LPP (1%,1,392), SLE (1%,1,150), and acne(1,1%) were less common.
MEAN CD4 COUNT In this study mean CD4 count was 280 cells/ul
Immune Categories
Various skin disorders in HIV patients were grouped into C1, C2 and C3 under the CDC Classification system based on the CD4 count. In the present study 50%(50) patients were in C4 category which is consistent with the study by Zancanarao et al who have reported 48.52% patients in C3 category. In the present study 44% (44) were in C2 category and 6% (6) were in C1 category.
Manifestations below 50 (cells/ul)
In the present study, out of 100 patients, 19% (19) had CD4 counts below 50 cells/ul. In the present study out of 19 patients having CD4 counts below 50cells/ul, 13% (13) patients had infectious mucocutaneous manifestations including oral candidiasis (3%), folliculitis (3%), herpes zoster (2%), herpes simplex (1%),
furunculosis (1%), scabies (1%), tineacorporis (1%).
Remaining 6% (6) of patients had non-infectious mucocutaneous manifestations. Among them 3% (3) patients had drug reactions, 2% (2) patients had PPE, and 15 (1) of patients had posriaisis. S.
Conclusion
The skin disorders are common and diverse in HIV positive patients and patients with advanced stages of skin problems have relatively low CD4 counts.
The results of this study indicated that all HIV positive patients should be examined for skin disorders because early diagnosis and management of such problems will improve the quality of life in these patients.
A low CD4 counts was associated with higher number of skin disorders and increased incidence of viral, fungal infections, PPE, adverse drug reactions.
Cutaneous manifestations can serve as dependable markers of HIV disease.
There was inverse relation relationship between the CD4 counts and the incidence and severity of skin disease in the HIV/AIDS patients.
Cutaneous manifestations of HIV can be considered as good clinical indicators to predict and assess the underlying immune status in resource-poor countries.
Conflict of Interest
None.
Source of Funding
None.
References
- CB Bunker, F Gotch, T Burns, S Breathmach, N Cox, C Griffiths. AIDS and Skin. Rooks Textbook of Dermatology, 7th Edn. 2004. [Google Scholar]
- AS Fauci, H Clifford Lane, E Braunwald, SL Hauser, AS Faui, L Long. Human Immunodeficiency Virus (HIV) disease: AIDS and reacted disorders. Harrison‘s Principles of Internal Medicine. 15th edn. 2001. [Google Scholar]
- PK Kaviarasan, TJ Jaishankar, DM Thappa, S Sujata. Clinical variations in dermatophytosis in HIV infected patients. Indian J Dermatol Venerol Leprol 2002. [Google Scholar]
- A Shobhana, SK Guha, DK Neogi. Mucocutaneous manifestations of HIV infection. Indian J Dermatol Venerol Leprol 2004. [Google Scholar]
- BK Goh, RKW Chan, P Sen, CTS Theng, HH Tan, YJ Wu. Chan et al, spectrum of skin disorders in human mmunodeficiency virus infected patients in Singapore and the relationship to CD4 lymphocyte counts. Int J Dermatol 2007. [Google Scholar] [Crossref]
- H Singh, P Singh, P Tiwari. Dermatological manifestations in HIV-infected patients at a tertiary care hospital in a tribal (Bastar) region of Chhattisgarh, India. Indian J Dermatol 2009. [Google Scholar] [Crossref]
- AE Naburi, B Leppard. Herpes zoster and HIV infection in Tanzania. Int J STD AIDS 2000. [Google Scholar] [Crossref]
- PCQ Zancanaro, LY McGirt,, AJ Mamelak, R H-N Nguyen, CR Martins. Cutaneous manifestations of HIV in the era of highly active antiretroviral therapy: an institutional urban clinic experience. J. Am Acad Dermatol 2006. [Google Scholar] [Crossref]
- Introduction
- Aim of the Study
- Materials and Methods
- Results
- Age distribution
- Sex distribution
- Infectious mucocutaneous manifestations and CD4 count
- Mucocutaneous manifestations and immune categories
- Non- infectious mucocutaneous manifestations and CD4 cell count
- Non infectious mucocutaneous manifestations and immune categories
- Immune categories
- Discussion
- Age group
- Sex
- Mucocutaneous Manifestations and CD4 Cell Count
- Infectious mucocutaneous manifestations and CD4 count
- Non Infectious mucocutaneous manifestations and CD4 cell count
- Immune Categories
- Manifestations below 50 (cells/ul)
- Conclusion
- Conflict of Interest
- Source of Funding
