- Visibility 73 Views
- Downloads 6 Downloads
- DOI 10.18231/j.ijced.2022.046
-
CrossMark
- Citation
Is the targeted approach for vitiligo satisfactory?
- Author Details:
-
G Manmohan
-
Swathi Bhanavath
-
Sunil Chaudhry *
Introduction
Vitiligo vulgaris is an acquired chronic pigmentation disorder characterized by white patches, often symmetrical, which usually increase in size with time, corresponding to a substantial loss of functioning epidermal and sometimes hair follicle melanocytes.
Types
Basically, there are two types of vitiligo Generalized or bilateral symmetrical form (80%) of vitiligo is a disease that destroys skin and mucosal membranes melanocytes progressively.

The localized form of vitiligo is divided into either segmental or focal forms. Segmental vitiligo, which is less common, affects only about 5% of adults and 20% of children affects only one area of the body on only one side, without crossing the midline of the body. It does not respond well to treatment.

Focal forms include spots on mucosal parts of the body (like the lips, inner nose, or genital areas), and so the pattern is called mucosal vitiligo.

If affects lips and fingertips, it’s called lip-tip vitiligo. Vitiligo involves the lips or other parts of the face plus the hands and/or feet, is termed acrofacial vitiligo.[1]
Vitiligo has a rarer inflammatory variant shows an inflammatory border (inflammatory vitiligo), a dermal lymphocytic infiltrate dermatitis, and mild spongiosis is observed.[2]
The prevalence of vitiligo is high in India, varying in the range of 0.46-8.8%, onset can be observed in 3rd decade of life. Familial occurrence has been reported to vary from 5 to 30% in different studies, they also report more female preponderance.[3]
There is a strong genetic predisposition for vitiligo. 20% of vitiligo patients have at least 1 first-degree relative with vitiligo, and the relative risk of vitiligo for first-degree relatives is increased by 7- to 10-fold. Linkage and association studies have provided strong support for vitiligo susceptibility genes on chromosomes 4q13-q21, 1p31, 7q22, 8p12, and 17p13. HLA-A∗02, A33, and Aw 31 are associated with an increased risk of vitiligo. [4], [5]
Pathogenesis
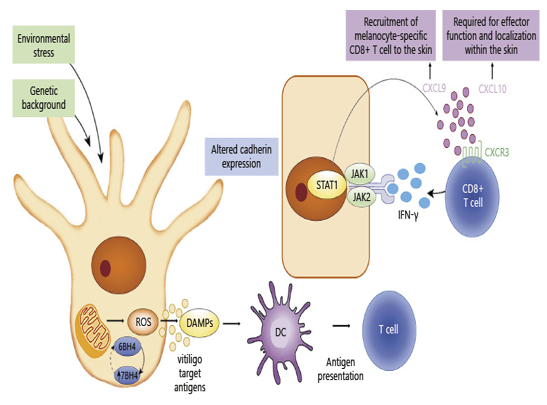
Autoimmune theory: Some of the mediators for vitiligo include T helper 1 cells, cytotoxic T cells, regulatory and resident memory T cells, as well as dendritic cells (DCs), natural killer (NK) and ILC-1 cells. Mediators such as interferon-γ (IFN-γ), C-X-C chemokine ligand 9 (CXCL9) and 10 (CXCL10), as well as interleukin-15 (IL-15) are also implicated in etiology of vitiligo.
IFN-γ is the key cytokine mediator that leads to the phosphorylation of the transcription factor STAT1 by Janus kinases (JAK) 1 and 2. IFN-γ, which activates JAK/STAT pathway and causes keratinocytes to produce the chemokines CXCL9 and CXCL10.[6]
Tumor necrosis factor-alpha (TNF-α) is one of the major cytokines implicated in the pathogenesis of vitiligo. TNF-α has been shown to inhibit melanocyte differentiation from stem cells, hamper melanocyte function and destroy melanocytes through induction of various apoptotic pathway.[7]
Oxidative stress theory: Reactive oxygen species generation causes an alteration in the expression of the antioxidant system affecting melanocyte function.
Neuropeptide theory: increased level of neuropeptides such as neuropeptide Y (NPY) has been observed in the marginal areas of vitiligo lesions triggered under the conditions of oxidative stress that is thought as a reason for the induction of vitiligo.
Viral association: strong association between vitiligo and hepatitis C virus (HCV) and hepatitis B virus (HBV) infections in vitiligo patients. [8]
Diagnosis
Autoimmune disorders include autoimmune thyroid disease, pernicious anemia, insulin-dependent diabetes, Systemic Lupus Erythematic (SLE), and Addison disease. These are associated with vitiligo. Hypothyroidism is commonly associated with vitiligo.
Clinical diagnosis
The changes are most striking in people with darker skin. Commonly affected areas are the face, fingers and toes, wrists, elbows, knees, hands, shins, ankles, armpits, anus and genital area, navel, and nipples.
Childhood vitiligo is often associated with a marked psychosocial element and the female preponderance is more.
Wood lamps can detect areas of skin that are pigmented or depigmented. It helps identify focal melanocyte loss and detect areas of depigmentation that may not be visible to the naked eye.
Microscopic diagnosis
Melanocytes are always reduced more in vitiligo; Degenerative changes have also been reported in nerves and sweat glands
Electron microscopy
No melanocytes, Keratinocyte apoptosis.
ANAs (antinuclear antibodies) can be positively found in the disease, where prevalence was found to be 35%.
Severity Scores
Vitiligo Extent Score (VES) is based on clinical pattern recognition of depigmentation of all areas of the body.
Vitiligo Area Scoring Index (VASI). Here, the extent of depigmentation is assessed based on six different areas of the body with specification of the percentage, which is multiplied by the degree of residual depigmentation[9] One hand unit (which encompasses the palm plus. The volar surface of all digits) is equivalent to 1% of the total body surface area.
The degree of depigmentation is estimated as follows:
100% -complete depigmentation-total absence of pigmentation.
90% -specks of pigment present.
75% -depigmented area exceeds the pigmented.
Area
50% -depigmented and pigmented areas are equal
25% -pigmented area exceeds depigmented area
10%-only specks of depigmentation are present [10]
VASI = ∑[Hand Units] x [Residual Depigmentation] all body sites
Stability of vitiligo
Stability refers to the arrest of the disease activity and is defined for vitiligo as the absence of new lesions, no extension of pre-existing lesions, and the absence of Koebner’s phenomenon (KP).
Active vitiligo
Characterized by inflammatory, trichrome and confetti like lesions, ill-defined hypopigmented borders and Koebner’s phenomenon.(KP). [11]
|
vitiligo activity |
Time period |
VIDA score |
|
Active condition |
45 days or less |
+4 |
|
Active condition |
45 days to 90 days |
+3 |
|
Active condition |
90-180 days |
+2 |
|
Active condition |
180-365 days |
+1 |
|
Stable condition |
365 days or more |
0 |
|
Stable plus spontaneous repigmentation |
365 days or more |
-1 |
Koebners phenomenon
Vitiligo has traditionally been a classical dermatosis to be aggravated by a variety of trauma. Three types have been subsequently defined. [12]
|
Type 1 (history) |
A history of depigmentation following various types of trauma (physical, chemical contact dermatitis, radiotherapy) |
|
Type 2 (clinical examination) |
2a) Sites involved in repeated friction like elbows, knees, drawstrings, clothes, and accessories |
|
|
2b) Morphology pointing towards the shape of an object or pattern of an obvious trauma (linear, crateriform, punctate) |
|
Type 3 (experimentally induced) |
Experimental induction of friction, epidermal trauma, or epidermal-dermal trauma |
Differential Diagnosis
This commonly includes Lichen planus, Pityriasis alba, Tinea Versicolor, Melanoma associated depigmentation, Mycosis Fungoides, Atopic eczema[13]
Therapy for vitiligo:[14]
|
First Line Therapy |
Second Line Therapy |
Third Line Therapy Surgical procedures |
||
|
Topical steroids alone orwith topical vitamin D3analogs |
Oral steroids mini-pulsetherapy for 3-4 months |
Punch grafts (small plugs of skin are transplanted to holes created in the white spots) |
Split thickness skin grafts (larger pieces of skin are transplanted to white spots where the skin has been removed) |
Cellular grafts (melanocytes and other skin cells from normal skin are transplanted to white spots where the top layer has been removed by dermabrasion or laser treatment) Monodispersed skin graft - suspension of dissociated keratinocytes and melanocytes, which are grafted |
|
Topical calcineurininhibitors (They dampen the cellular immune response) Combination with topical corticosteroids pimecrolimus 1 % or tacrolimus 0.1 % improves the responserate. |
308nm laser withcalcineurin inhibitors |
Monobenzone (monobenzyl ether of hydroquinone, MBEH) 20 to 40 percent is usually the treatment of choice of depigmentation therapy for severe cases of vitiligo. |
||
|
Associated Support- Camouflage- elf-tanning agents, stains, dyes,whitening lotions, tinted cover creams, compact,liquid and stick foundations |
PUVA therapy |
Cellular Therapies: New Cellular Transplantation Techniques Epidermal Cell Suspension Cultured melanocyte suspension Cultured Epidermis |
||
|
Psychotherapy helps the psychosocial effects ofvitiligo, but may also cause disease regression |
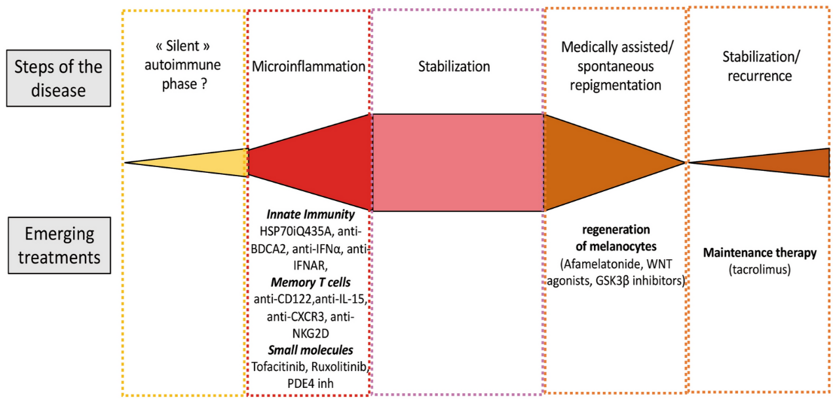
Biologics: Ruxolitinib cream, for topical use Ustekinumab Tofactinib |
|
Use of non-biologicals
Topical corticosteroids are the usual first-line treatment. Responses to corticosteroid therapy in vitiligo 20% and 90% improvement, which are usually achieved but not a total cure. Ease of application, high rate of compliance, and low cost are the advantages of topical corticosteroid therapy. Vitiligo is being treated either with 0.I% betamethasone valerate (BV) or with 0.05% clobetasol propionate (CP) creams. [15]
Oral Steroids
Low-dose oral dexamethasone mini pulse therapy of 2.5 mg per day on two consecutive days of the week stopped vitiligo in 91.8%.[16], [17]
After 4 months of treatment, 76% showed regimentation while the arrest of progression (both regimentation and stationary) was noted in 90% of patients. High numbers of cytotoxic CD8+ T cells are found in the blood of patients with vitiligo, their number significantly decreases after treatment corticosteroids are provided at the onset or early stages of the disease, they can reduce disease progression and promote regimentation.[18]
Calcineurin inhibitors: Tacrolimus, a macrolide immunosuppressant. Tacrolimus prevents signal transduction pathways from occurring, which ultimately halts the transcription of cytokines, including interleukin (IL) 2, IL-3, IL-4, IL-5, IL-8, tumor necrosis factor α, and interferon γ, which signal production of vitiligo. Tacrolimus inhibits calcineurin, which is involved in the production of interleukin-2, a molecule that promotes the development and proliferation of T cells,. Apart from inhibitory action on T-cells topical calcineurin inhibitors increase the activity of tyrosinase and promote melanogenesis. Tacrolimus stimulates the expression of MIFT (micro ophthalmic transcription factor) and melanocyte migration. In fact the induction of melanocyte migration by tacrolimus is much more significant than that induced by endothelin 1.[19]
These have special utility in the treatment of facial lesions, where corticosteroids can induce atrophy of thinner skin. Tacrolimus 0.1% ointment has been observed to have an efficacy equal to the 0.05% clobetasol propionate. A combination of tacrolimus with excimer has been shown to be effective in the treatment of acral vitiligo, which is typically UV-resistant. Its combination with NB-UVB enhances repigmentation rates compared with NB-UVB alone, but a meta-analysis did not support this observation and concluded that apart from face and neck, where calcineurin inhibitors can enhance the effect of NB-UVB phototherapy, adding topical calcineurin inhibitors or vitamin D analogs to NB-UVB has no effect on the degree of repigmentation achieved. 14% patients do not respond to these agents Moreover, continued application of tacrolimus 0.1% ointment twice a week has been shown to be an effective maintenance therapy.[20] The results with pimecrolimus are variable. Its effects are said to be more superior on face than on elsewhere. A recent meta-analysis supports the previous observation and recommends treatment with calcineurin inhibitors in vitiligo, both as monotherapy and in conjunction with phototherapy. Lotions and gel formulations are available to treat hair-bearing areas and mucosal sites.[21] As much as Topical tacrolimus At 0.03% concentration, it has been approved for use in children aged 2 to 15 years, while a 0.1% concentration has been approved for use in adults. The treatment should be prescribed initially for 6 months, which can be prolonged to 12 months safely.[22]
Pimecrolimus binds with high affinity to the protein receptor macrophilin-12(FKBP-12). The release of cytokines (which cause inflammation, redness and itching) from T-cells and mast cells is blocked. Pimecrolimus cream 1% results in regimentation in vitiligo to different extents according to the location of the lesion.

Minocycline
It has been shown to protect melanocytes against hydrogen peroxide-induced death in vitro. A preliminary study revealed its effectiveness in halting the slowly spreading vitiligo.[23] 100 mg of minocycline daily for 3 months, the arrest of activity was achieved in 90.6% of patients, and moderate to marked regimentation was observed in 21.8% of patients with vitiligo. Recently, it has been shown that minocycline can rescue melanocytes from oxidative stress in vitro. [24], [25]
Zinc: Serum zinc level is low in patients with generalized vitiligo. Zinc plays an essential role in the release and synthesis of the α-melanocyte-stimulating hormone in animals and works as an active agent in melanogenesis in humans. It can control vitiligo through inhibiting production of free radicals. Daily administration of 45mg of zinc seems to reduce IL-6 serum levels.[26], [27], [28]
Afamelanotide is an α-melanocyte stimulating hormone (α-MSH) analogue that stimulates melanogenesis and melanocyte proliferation by binding to the melanocortin-1 receptor (MC1R). causes the production of eumelanin and consequently increases melanin levels within epidermal melanocytes. Monthly subcutaneous implantation of 16 mg of afamelanotide resulted in a significantly superior and faster regimentation compared with narrowband ultraviolet B monotherapy. The onset of regimentation was observed the earliest for upper extremities.[29], [30]
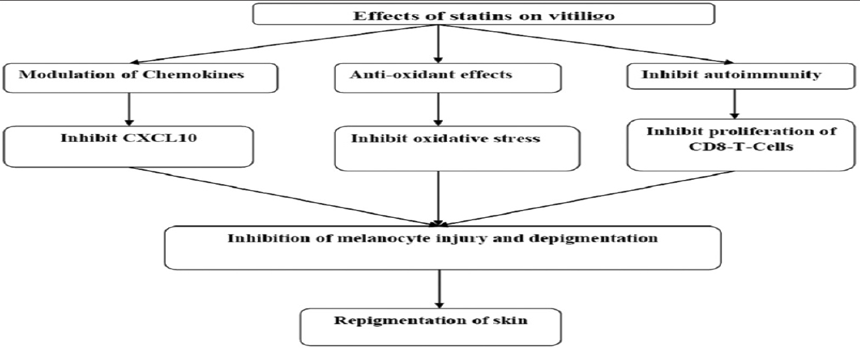
Statins: 17 serum level is increased in patients with vitiligo and statins have been found to be a potent inhibitor of IL‑17 through inhibition of T cells proliferation and induction of immunotolerance. The effective dose of simvastatin for regimentation of vitiligo is 80 mg/day in preliminary trials. Topical simvastatin may be used at a concentration of 1.0 mmol/L for vitiligo lesions, which is more effective with low adverse effects. Treatment with rosuvastatin increases serum levels of 25-hydroxyvitamin D, which can be beneficial in some patients of vitiligo.
Topical 5 Fluorouracil
5% fluorouracil cream was applied daily to vitiliginous lesions under occlusive dressings, following an epidermal abrasion or needling. Needling induces a strong trauma-induced inflammatory response inciting migration of keratinocyte along with melanocyte. Micro-needling with 5-FU, was associated with regimentation percentage of 67.24%.[31], [32], [33]
Vitamin D analogs
In many studies Vitamin D analogues as monotherapy were less effective than topical corticosteroids in vitiligo. There is some evidence of an additive effect with combining the two. Vitamin D ligands are designed to target the local immune response in vitiligo, acting on T cell activation. Vitamin D3 compounds (calcipotriol and tacalcitol) are known to influence melanocyte maturation and differentiation and also to up-regulate melanogenesis through the endothelin receptor.[34] The combination therapy of topical steroid and tacalcitol is effective and safety therapeutic candidate for vitiligo. There is evidence that topical therapy of vitamin D analog is effective for children between the ages of 5 to 17 years with vitiligo.[35]
Methotrexate treatment results in a decreased number of T cells capable of TNFa production, whereas the number of T cells producing IL-10 after polyclonal activation increased. MTX with 25mg dose/ week for 6 months reduced vitiligo patches.[36]
Others: Topical placental extract, and Basic fibroblast growth factor beta-fibroblast growth factor (b-FGF) decapeptide have been found to be effective in combination with phototherapy. b-FGF is released from the keratinocytes on exposure to NB-UVB, and it helps in melanocyte migration. [37] Another pathway that has been recently found is activation of wnt-beta catenin signaling. This signaling is vital for differentiation of melanoblasts into functioning melanocytes and was found to be impaired on exposure to oxidative stress. The wt agonists have been demonstrated to enhance melanocyte differentiation in ex-vivo studies. Also, dermal fibroblasts from hands and feet were found to secrete wt inhibitors and might be responsible for difficult repigmentation obtained at these sites. One of the plausible mechanisms of action of phototherapy is the induction of wnt signaling. These molecular targets should be utilized in the development of novel therapeutic targets for vitiligo.[11]
Unconventional Therapies
Alpha-lipoic acid has been proposed in the treatment of vitiligo, to prevent the destruction of melanocytes by free radicals. It is given orally at dosages, ranging from300 to 1,800 mg daily.
Levamisole
It has immunoregulatory properties, used alone or with steroids with has demonstrated some benefit. A dose of 150 mg of levamisole given for 2 days consecutively in a week. Initial study observed encouraging results. In above 90% patients, where aggressive arrest of activity is seen within 2 -4 months.[38], [39]
L-Phenylalanine (precursor of dopamine) may be administrated both orally (50 – 100 mg/kg of body weight) or topically, and provide better results if combined with UV exposure. Omega-3 fatty acids have been proposed for vitiligo treatment and to limit the side effects due to phototherapies. Topic gel composed by PGE2 has been introduced for the treatment of vitiliginous patients, as it stimulates melanocytes. Vitamin A, B12, C and E are used in vitiliginous patients, because of their antioxidant properties. Resveratrol and Soyabeans (rich in flavonoids) is useful in patients of Vitiligo. Melagenine is an alcohol extract of human placenta, which has been proposed for the topical treatment of vitiligo patients. Flavonoids due to their antioxidant action, have been proposed as supplements in the treatment of vitiligo patients. The unconventional therapies can be used only as adjuvants.
Homeopathic medicines for vitiligo which are evaluated to reduce white patches are Calcarea Carb, Arsenic Album, Ars Sulph Flavum, Hydrocotyle Asiatica and Kali Carb. [40]
Phototherapy of Vitiligo
This is the most successful treatment options for vitiligo, both monotherapy and combination therapy. [41], [42] phototheraphy includes sunlight, UVA(ultraviolet A), puva(PSORALEN PLUS UVA),BB-UVB(Broadband ultraviolet B), NB-UVB(Narrow Band UVB) and excimer. The damage caused by UV radiation activates p53 in keratinocytes, and mediates the transcription and release of various growth factors from keratinocytes in a paracrine fashion. These mediators can elicit some immediate and late changes in melanocytes.Immediate responses involve p53-mediated enhanced survival. The late response include NB-UVB-mediated transcription of MITF (Melanocyte inducing transcriotion factor), which mediates increase in melanogenesis and transfer of melanin to keratinocytes, resulting in photoprotection. UV radiation also causes mitosis of melanocytes and results in activation, migration, and proliferation of dormant melanocytes residing in the outer root sheath of hair follicles initiating repigmentation of vitiligous skin. NB-UVB (maximum emission between 311 and 312 nm) can induce apoptosis of T-cells in active disease. By inducing IL-10, it stimulates the differentiation of Tregs (regulatory T cells), which also inhibit the autoreactive cytotoxic T-cells. The biostimulation of functional melanocytes in the perilesional skin and immature melanocytes in hair follicles results in repigmentation after treatment with NB-UVB. NB-UVB causes activation, proliferation, and finally migration of melanocytes from hair follicles and also from perilesional skin. NB-UVB promotes melanocyte growth and proliferation by increasing the expression of endothelin-1 and b-FGF by keratinocytes. Migration of melanocytes toward depigmented skin is facilitated by enhancing the phosphorylated focal adhesion kinase and MMP-2 activity in melanocytes. 114 NB-UVB also reduces the oxidative stress in vitiligo. Higher doses of
NB-UVB may be required to achieve stabilization than in achieving repigmentation. It has been observed that the response to phototherapy is better in recent onset vitiligo than the long-standing one (>1-2 years of disease). The involvement of melanocytes in hair follicles (characterized by leukotrichia) is a limiting factor to phototherapy. Therefore, early treatment is recommended to avoid the development of leukotrichia. [43], [44], [45], [46]

Guidelines for Nb-Uvb Treatment
Guidelines for NB-UVB treatment have been recently published from Vitiligo Working Group.
These guidelines recommend to start NB-UVB treatment from 200 mJ/cm2 regardless of the (skin phototype and an increment of 10-20%per session till a desired erythema is achieved (pink, asymptomatic erythema lasting less than 24 hours).
Although optimal conditions imply a thrice-a-week exposure, twice-weekly treatments are also acceptable, as these are more patient-friendly and enhance long-term compliance.
Thrice-weekly exposures result in a faster and earlier-onset repigmentation; however, the final repigmentation outcomes are dependent on the total number of exposures rather than the frequency of exposures.
Maximum acceptable dosage on the face is 1500 mJ/cm?, and that on the trunk is 3000 mJ/cm?. Higher doses can be administered, especially in darker phototypes.
Carcinogenic potential of PUVA is already known, more so in Caucasians. Carcinogenic potential of NB-UVB has not yet been proved in larger studies and is considered safe in darker phototypes. Still, caution should be exercised beyond 3000 mJ/cm?. Moreover, an annual full-body screening is recommended for phototypes I-III after completion of NB-UVB treatment.
Carcinogenic potential of PUVA is already known, more so in Caucasians. Carcinogenic potential of NB-UVB has not yet been proved in larger studies and is considered safe in darker phototypes.Still, caution should be exercised beyond 3000 mJ/cm?. Moreover, an annual full-body screening is recommended for phototypes I-III after completion of NB-UVB treatment.
The aim of a phototherapy session is to induce a pink-colored asymptomatic erythema that lasts <24 hours. Till this aim is achieved, it is advisable to increment the dosing by 10-20% at each session.
Once the desired aim of pink asymptomatic erythema lasting <24 hours is achieved, the same dose is maintained till this erythema disappears, and increments of 10-20% are again administered till the desired erythema is achieved once more and so on.
If erythema is bright red and asymptomatic. Withhold phototherapy till it becomes light pink, and re-start at the previous dose.
If symptomatic erythema appears (like pain, edema, blistering), withhold phototherapy till healing and restart at the last tolerated dose.
Reduction of 25% and 50% is recommended with a gap of 8-14 and 15-21 days in treatment sessions, respectively. For a gap of 4-7 days, it is recommended to maintain at same dose, whereas for a gap of >21 days it is recom-mended to start again from 200 mJ/cm?.
After replacement of the bulbs or device calibration, a reduction in 10-20% of the dose is suggested.
Excess sun exposure beyond phototherapy sessions should be avoided, and 2 hourly sunscreen applications with a sun protection factor of 30 are recommended for all phototypes.
14. Apart from oil application, the rest of all topical medications (except psoralens) are not to be applied within 4 hours before the phototherapy session.
Face should be covered, if not involved by the disease. Areolae in women and genitals in men should be shielded. While receiving treatment for eyelid lesions, eyes should be firmly closed. Otherwise, a goggle is recommended.
Maintenance sessions after completion of NB-UVB treatment involve twice weekly for the first month, once weekly for the second month, and once every alternate week for the third month followed by discontinuation.
A topical treatment has been proposed for vitiligo, which consists of topical application of a cream consisting of diethylamino hydroxybenzoyl hexylbenzoate and alpha-glucosyl-hesperidin.
These ingredients actively filter all wavelengths except 311 nm that is selectively delivered to the vitiligo lesions after application of this cream. This formulation was found to be effective in treating vitiligo, and further trials are ongoing to assess the efficacy of this treatment option.
-With PUVA ( Combines 8-methoxypsoralen taken by mouth followed 45-60 minutes later by exposure of the skin to UVA phototherapy), it showed that the treatment response after 12 months of treatment was better than that after 6 months. Face and trunk lesions showed better regimentation than other areas, whereas hands, feet, perioral, and periorbital areas were generally refractory to treatment. [45] PUVA therapy seldom achieves extensive regimentation that is cosmetically acceptable, and treatment response is often followed by relapse. Retention of PUVA-induced repigmentation has been observed in more than 90% of patients, 14–15 years after discontinuation of treatment. [47], [48] Phototherapy is an excellent modality to induce stability in active vitiligo. It takes usually around 3.5 months to induce stability. NB-UVB is more effective than PUVA in inducing stability and producing repigmentation in active vitiligo. Moreover, recent meta-analyses have shown that long-term NB-UVB (12 months) can lead to maximum repigmentation rates. Face and neck were the sites that showed best repigmentation, followed by trunk and limbs. The long-term risk of skin cancer is well established for PUVA. NB-UVB, as well as targeted UVB phototherapies. [49], [50]
Excimer
Excimer laser (xenon chloride) has a monochromatic wavelength of 308nm.it is responsible for melanoblast differentiation.it is more effective than NB-UVB because it has been shown greater inhibitory effect on T-cells and causes maximum T-cell apoptosis and endothelin secretion of all UVB modalities. Repigmentation is faster with more frequent excimer treatments but the ultimate repigmentation depends upon total number of treatments than frequency. There is no difference with excimer lamps versus laser versus conventional NB-UVB phototheraphy treatment. [51]
Herbal drugs
Ammi visnaga, Angelica sinensis, Eclipta alba, Ginkgo biloba, Picrorhiza kurroa, and Psoralea corylifolia, have been evaluated in some studies. The postulated mode of action is Interleukin-17 inhibition.
|
Herbs |
Active ingredient |
|
Cucumis melo |
Cucumis melo superoxide dismutase |
|
Green Tea |
Epicatechin, epicatechin-3-gallate, epigallocatechin |
|
Picrorhiza kurroa |
Picroside I and picroside II |
|
Polypodium leucotomos |
p-coumaric, ferulic, caffeic, vanillic, 3,4 - dihydroxybenzoic, 4 - hydroxybenzoic, 4 - hydroxycinnamic, 4 -hydroxycinnamoyl - quinic, chlorogenic acids |
Biologicals
Ruxolitinib is a selective Jak1/2 inhibitor with little or no affinity toward Jak 3 receptor. Tofacitinib on the other hand is an inhibitor of Janus kinase Jak3 and Jak1 receptors and to a lesser extent Jak2 receptor, works to decrease the intracellular activity of immune cells by preventing cytokine or growth factor-mediated gene expression. [52]
Ruxolitinib cream 1.5% for the treatment of nonsegmental vitiligo in adult and pediatric patients 12 years of age and older. Phase 3 clinical trials that found 30% of patients using the cream regained 75% or more skin regimentation on the face and roughly 20% of patients regained at least 50% or more regimentation on their body after 24 weeks.
In the United States, the approved dosage forms of Tofacitinib are an oral tablet in either 5 or 10 mg and an extended-release tablet that is 11mg. Patients on Tofacitinib need to be monitored for bone marrow suppression and potential infections due to the suppression of immune cells in the body. Tofacitinib is currently being studied for use in Vitiligo. One of the central pathways of vitiligo that seems to be important to the disease progression is the interferon-gamma signaling pathway. Involved in this pathway are the JAK receptors. Because of this the use of a JAK receptor can be used to block the pathway and therefore block the progression of the disease and help induce regimentation.
Special scenarios
Pediatric vitiligo are almost same as adults Pimecrolimus can be used instead of Tacrolimus in very young children. During pregnancy and breast feeding NB-UVB can be given with replenishment of folate when expressed NB-UVB. Segmental vitiligo does not respond to medical treatments and generally responds to surgical treatments once disease has stabilized.
Effect of vitiligo on quality of life
Social concerns of a vitiligo patient is best assessed by using ‘vitiligo impact scale-22’ than Dermatology quality of life index (DLQI) which only correlated moderately with reduction in quality of life perceived by the patients. [53]
Surgical options
The aims of surgery are twofold:
To slow the progression of pigment loss.
Bring back the natural skin colour to abnormal white patches
Grafting of melanocyte-rich tissue grafting of melanocyte cell suspensions
Miniature punch grafting (MPG)-Autologous non cultured epidermal cell suspensions.
Suction blister grafting-Cultured melanocyte suspensions.
Split thickness skin grafting.
Complications of surgery include infections, alterations in texture of skin, hyperpigmentation. scarring and graft rejection.
Better results are reported in focal and segmental vitiligo (75%-95%), than in generalized vitiligo.[54]
Autologous Mesenchymal stem cell therapy has been shown to stimulate the mobilization of healthy melanocytes, leading to successful repigmentation of skin lesions in vitiligo patients.[55]
Conclusions
Vitiligo is a psychologically devastating skin condition, where patchy skin due to melanin dysfunction makes patients more aware of their physical appearance. Nearly 50 % of patients develop the disease before 20 years of age. Onset at an advanced age occurs but is unusual, and should raise concerns about associated diseases, such as thyroid dysfunction, rheumatoid arthritis, diabetes mellitus, and alopecia areata. The treatment modalities in vitiligo are mostly nonspecific. Complete regimentation of all the patches of vitiligo is never achieved, and nearly 15-30% of patients do not respond at all. In most of the trials, regimentation of more than 75% is considered a significant improvement. Problems with surgical therapy include the inability to treat large areas and the risk of the Koebner Phenomenon at the graft site. Cultured melanocytes at a density of 70 000 to 100 000 melanocytes/cm2 are transplanted to an area covering as much as 500 cm2, provide significant results in those where there is some inherent melanin production. Topical steroids are often used as a monotherapy or in combination with ultraviolet radiation. calcineurin inhibitors (tacrolimus and pimecrolimus) are not always well-tolerated. JAK inhibitors, such as ruxolitinib, baricitinib, and tofacitinib, are effective, elucidating the mode of action of the IFN-γ-chemokine signaling axis in the pathogenesis of vitiligo. There are no randomized controlled clinical trials for the same. Young individuals may regain the colour of skin when are treated much earlier after diagnosis and about 10 – 20 percent regain their skin colour. The clinical course of vitiligo remains unpredictable and the therapies used for long duration are not much satisfying.
Source of Funding
None.
Conflicts of Interest
There is no conflict of interest.
References
- MHA Jalali, B Jalali, M Jafari, MA Isfahani. Treatment of segmental vitiligo with normal-hair follicle autograft. Med J Islam Repub Iran 2013. [Google Scholar]
- LA Soro, AJ Gust, SM Purcell. Inflammatory vitiligo versus hypopigmented mycosis fungoides in a 58-year-old Indian female. Indian Dermatol Online J 2013. [Google Scholar]
- RV Vora, BB Patel, AH Chaudhary, MJ Mehta, AP Pilani. A Clinical Study of Vitiligo in a Rural Set up of Gujarat. Indian J Community Med 2014. [Google Scholar] [Crossref]
- Z Xue-Jun, C Jian-Jun, L Jiang-Bo. The genetic concept of vitiligo. J Dermatol Sci 2005. [Google Scholar]
- M Rashighi, JE Harris. Vitiligo Pathogenesis and Emerging Treatments. Dermatol Clin 2017. [Google Scholar] [Crossref]
- N Hlaˇca, T Žagar, M Kaštelan, I Brajac, L Prpić-Massari. Current Concepts of Vitiligo Immunopathogenesis. Biomedicines 2022. [Google Scholar] [Crossref]
- NC Laddha, M Dwivedi, R Begum. Increased Tumor Necrosis Factor (TNF)-α and its promoter polymorphisms correlate with disease progression and higher susceptibility towards vitiligo. PLoS One 2012. [Google Scholar] [Crossref]
- R Rahman, Y Hasija. Exploring vitiligo susceptibility and management: a brief review. Biomed Dermatol 2018. [Google Scholar] [Crossref]
- M Böhm, JA Schunter, K Fritz, C Salavastru, S Dargatz, M Augustin. S1 Guideline: Diagnosis and therapy of vitiligo. J Dtsch Dermatol Ges 2021. [Google Scholar] [Crossref]
- G Lannella, A Greco, D Didona, B Didona, G Granata, A Manno. Vitiligo: Pathogenesis, clinical variants and treatment approaches. Autoimmun Rev 2016. [Google Scholar] [Crossref]
- L Benzekri, Y Gauthier. Clinical markers of vitiligo activity. J Am Acad Dermatol 2017. [Google Scholar] [Crossref]
- N Van Geel, R Speeckaert, A Taieb, M Picardo, M Böhm, DJ Gawkrodger. Koebner's phenomenon in vitiligo:European position paper. Pigment Cell Melanoma Res 2011. [Google Scholar] [Crossref]
- V Eleftheriadou, R Atkar, J Batchelor, B McDonald, L Novakovic, J V Patel. British Association of Dermatologists guidelines for the management of people with vitiligo 2021. Br J Dermatol 2022. [Google Scholar] [Crossref]
- L Migayron, K Boniface, J Seneschal. Julien Seneschal, Vitiligo, From Physiopathology to Emerging Treatments: A Review. Dermatol Ther (Heidelb) 2020. [Google Scholar] [Crossref]
- SS Bleehen. The treatment of vitiligo with topical corticosteroids. Light and electronmicroscopic studies. Br J Dermatol 1976. [Google Scholar] [Crossref]
- P Manga, N Elbuluk, SJ Orlow. Recent advances in understanding vitiligo. F1000Res 2016. [Google Scholar] [Crossref]
- I Lee, H Chu, H Lee, M Kim, DS Kim. Oh retrospective Study of Methylprednisolone Mini-pulse Therapy Combined with Narrow-Band UVE Segmental Vitiligo. Dermatology 2016. [Google Scholar] [Crossref]
- K Banerjee, JN Barbhuiya, AP Ghosh, SK Dey, PR Karmakar. The efficacy of low-dose oral corticosteroids in the treatment of vitiligo patient. Indian J Dermatol Venereol Leprol 2003. [Google Scholar]
- KY Lee, SY Jeon, JW Hong, KW Choi, CY Lee, SJ Choi. Endothelin-1 enhances the proliferation of normal human melanocytes in a paradoxical manner from the TNF-a-inhibited condition, but tacrolimus promotes exclusively the cellular migration without proliferation: A proposed action mechanism for combination t. J Eur Acad Dermatol Venereol 2013. [Google Scholar] [Crossref]
- JH Lee, HS Kwon, HM Jung, H Lee, GM Kim, HW Yim. Treatment Outcomes of Topical Calcineurin Inhibitor Therapy for Patients with Vitiligo: A Systematic Review and Meta-analysis. JAMA Dermatol 2019. [Google Scholar] [Crossref]
- CCE Lan, CS Wu, GS Chen, HS Yu. FK506 (tacrolimus) and endothelin combined treatment induces mobility of melanoblasts: New insights into follicular vitiligo topical tacrolimus on sun repigmentation induced exposed skin. Br J Dermatol 2011. [Google Scholar] [Crossref]
- LB Travis, JM Weinberg, NB Silverberg. Successful Treatment of Vitiligo With 0.1% Tacrolimus Ointment. Arch Dermatol 2003. [Google Scholar] [Crossref]
- D Parsad, A Kanwar. Oral minocycline in the treatment of vitiligo - A preliminary study. Dermatol Ther 2010. [Google Scholar] [Crossref]
- H Seirafi, F Farnaghi, A Firooz, A Vasheghani-Farahani, NS Alirezaie, Y Dowlati. Pimecrolimus cream in repigmentation of vitiligo. Dermatology 2007. [Google Scholar]
- D Parsad, A Kanwar. Oral minocycline in the treatment of vitiligo--a preliminary study. Dermatol Ther 2010. [Google Scholar] [Crossref]
- R Yaghoobi, M Omidian, N Bagherani. Original article title: "Comparison of therapeutic efficacy of topical corticosteroid and oral zinc sulfate-topical corticosteroid combination in the treatment of vitiligo patients: a clinical trial". BMC Dermatol 2011. [Google Scholar] [Crossref]
- MR Mogaddam, NS Ardabili, N Maleki, MM Chinifroush, EM Fard. Evaluation of the serum zinc level in Dalents with vitiligo. Postepy Dermatol Alergol 2017. [Google Scholar] [Crossref]
- M Gupta, VK Mahajan, KS Mehta, PS Chauhan. ChauhanaPS Zinc therapy in dermalology: A review. Dermatol Res Pract 2014. [Google Scholar] [Crossref]
- HW Lim, PE Grimes, O Agbai, I Hamzavi, M Henderson, M Haddican. Afamelanotide and narrowband UV-B phototherapy for the treatment of vitiligo: a randomized multicenter trial. JAMA Dermatol 2015. [Google Scholar] [Crossref]
- K Li, M Ciao, X Wang, X Zhao, Q Sun. Effect of narrow band ultraviolet B phototherapy as monotherapy or combination therapy for vitiligo: a meta-analysis. Photodermatol Photoimmunol Photomed 2017. [Google Scholar] [Crossref]
- HM Al-Kuraishy, NR Hussian, MS Al-Naimi, AI Al-Gareeb. Statins Role in Vitiligo: A Mini‑Review. Turkish J Dermatol 2020. [Google Scholar] [Crossref]
- AK Singrodia, RD Mehta, D Sharma, P Choudhary, BC Ghiya, J Bai. Microneedling with topical 5-fluorouracil in the localized stable vitiligo – Is this the way out? – Our experience: A hospital-based study. J Dermatol Dermatol Surg 2021. [Google Scholar]
- T Lotti, K Agarwal, I Podder, F Satolli, M Kassir, RA Schwartz. Safety of the current drug treatments for vitiligo. Expert Opin Drug Saf 2020. [Google Scholar] [Crossref]
- G Khullar, A J Kanwar, S Singh, D Parsad. Comparison of efficacy and safety profile of topical calcipotriol ointment in combination with NB-UVB vs. NB-UVB alone in the treatment of vitiligo: a 24-week prospective right-left comparative clinical trial. J Eur Acad Dermatol Venereol 2015. [Google Scholar] [Crossref]
- Y Konishi, K Yamanaka, H Mizutani. Treatment of vitiligo vulgaris with the combination therapy of topical steroid and vitamin D3 compound. Dermatol Rep 2012. [Google Scholar] [Crossref]
- K Alghamdi, H Khurrum. Methotrexate for the treatment of generalized vitiligo. Saudi Pharm J 2013. [Google Scholar] [Crossref]
- CS Wu, Cce Lan, M H Chiou, HS Yu. Basic fibroblast growth factor promotes melanocyte migration via increased expression of p125FAK on melanocytes. Acta Derm Venereol 2006. [Google Scholar] [Crossref]
- JS Pasricha, V Khera. Effect of Prolonged Treatment With Levamisole on Vitiligo With Limited and Slow-Spreading Disease. Int J Dermatol 1994. [Google Scholar] [Crossref]
- S Agarwal, M Ramam, V K Sharma, S Khandpur, H Pal, R M Pandey. A randomized placebo-controlled double-blind study of levamisole in the treatment of limited and slowly spreading vitiligo. Br J Dermatol 2005. [Google Scholar] [Crossref]
- S Gianfaldoni, G Tchernev, J Lotti, U Wollina, F Satolli, M Rovesti. Unconventional Treatments for Vitiligo: Are They (Un) Satisfactory?, Open Access Maced. J Med Sci 2018. [Google Scholar]
- N Akdeniz, IH Yavuz, SG Bilgili, GO Yavuz, O Calka. Comparison of efficacy of narrow band UVB therapies with UVB alone, in combination with calcipotriol, and with betamethasone and calcipotriol in vitiligo. J Dermatolog Treat 2014. [Google Scholar] [Crossref]
- K Li, M Ciao, X Wang, X Zhao, Q Sun. Effect of narrow band ultraviolet B phototherapy as monotherapy or combination therapy for vitiligo: a meta-analysis. Photodermatol Photoimmunol Photomed 2017. [Google Scholar] [Crossref]
- TF Mohammad, M Al-Jamal, IH Hamzavi, JE Harris, G Leone, R Cabrera. The Vitiligo Working Group recommendations for narrowband ultraviolet B light phototherapy treatment of vitiligo. J Am Acad Dermatol 2017. [Google Scholar] [Crossref]
- U Khanna, S Khandpur. What Is New in Narrow-Band Ultraviolet-B Therapy for Vitiligo?. Indian Dermatol Online J 2019. [Google Scholar] [Crossref]
- X Wang, J Mccoy, T Lotti, A Goren. Topical cream delivers NB-UVB from sunlight for the treatment of vitiligo. Expert Opin Pharmacother 2014. [Google Scholar] [Crossref]
- S Esmat, RA Hegazy, S Shalaby, S Chu-Sung Hu, CC E Lan. Phototherapy and Combination Therapies for Vitiligo. Dermatol Clin 2017. [Google Scholar] [Crossref]
- A Bhatnagar, AJ Kanwar, D Parsad, D De. Comparison of systemic PUVA and NB-UVB in the treatment of vitiligo: An open prospective study. J Eur Acad Dermatol Venereol 2007. [Google Scholar] [Crossref]
- A Bhatnagar, Kanwar Aj, D Parsad, D De. Psoralen anc ultraviolet A and narrow-band ultraviolet B in inducing stability in vitiligo, assessed by vitiligo 1 disease activity score: An open prospective comparative study. Eur Acac Dermatoly Venereal 2007. [Google Scholar] [Crossref]
- JM Bae, HM Jung, BY Hong, JH Lee, WJ Choi, JH Lee. Phototherapy for Vitiligo: A Systematic Review and Meta-analysis. JAMA Dermatol 2017. [Google Scholar]
- S Kandaswamy, N Akhtar, S Ravindran, S Prabhu, SD Shenoi. Phototherapy in Vitiligo: Assessing the Compliance, Response and Patient's Perception about Disease and Treatment. Indian J Dermatol 2013. [Google Scholar] [Crossref]
- C Lopes, VFM Trevisani, T Melnik. Efficacy and Safety of 308-nm Monochromatic Excimer Lamp Versus Other Phototherapy Devices for Vitiligo: A Systematic Review with Meta-Analysis. Am J Clin Dermatol 2016. [Google Scholar] [Crossref]
- Rn Narayanaswamy, IS Ismail. Role of herbal medicines in Vitiligo treatment - Current status and future perspectives. Asian J Pharm Clin Res 2018. [Google Scholar] [Crossref]
- K Ezzedine, N Silverberg. A practical approach to the diagnosis and treatment of vitiligo in children. Pediatrics 2016. [Google Scholar] [Crossref]
- PK Ashwini, DJ Sushmita, S Veerana. Vitiligo with special emphasis on vitiligo surgery. Arch. Med Health Sci 2020. [Google Scholar] [Crossref]
- S Khandpur, S Gupta, D R Gunaabalaji. Stem cell therapy in dermatology. Indian J Dermatol Venereol Leprol 2021. [Google Scholar] [Crossref]
- Introduction
- Severity Scores
- Area
- Stability of vitiligo
- Active vitiligo
- Koebners phenomenon
- Differential Diagnosis
- Therapy for vitiligo:[14]
- Use of non-biologicals
- Oral Steroids
- Topical 5 Fluorouracil
- Unconventional Therapies
- Phototherapy of Vitiligo
- Guidelines for Nb-Uvb Treatment
- Excimer
- Herbal drugs
- Biologicals
- Special scenarios
- Effect of vitiligo on quality of life
- Surgical options
- Grafting of melanocyte-rich tissue grafting of melanocyte cell suspensions
- Conclusions
- Source of Funding
- Conflicts of Interest
