- Visibility 51 Views
- Downloads 4 Downloads
- DOI 10.18231/j.ijced.2024.078
-
CrossMark
- Citation
Comparative study of efficacy of intense pulsed light versus Intralesional triamcinolone in the treatment of hypertrophic scars and keloids
- Author Details:
-
Shilpa Haibatti Pathrikar
-
Bhargav Naik *
-
Anuj Bhatt
-
Trish Larissa Miranda
-
Hiteshi Kamboj
Introduction
The process of wound healing comprises of a series of modifications that ideally culminate into the development of a relatively flat and thin lined normotrophic scar.[1] In the event of excessive wound healing it may lead to scarring. Hypertrophic scars and keloids are the two common major types observed.[1], [2]
Few clinical researchers have reported that they could immensely affect the quality of life of patients.[3] Various mode of therapies have been proposed such as the silicone sheet and gel application, pressure garments, topical and intralesional injections of agents including corticosteroids, interferon, bleomycin, five-fluorouracil (5-FU), as well as cryotherapy, laser, radiotherapy and surgery.[4], [5], [6] Intense pulsed light (IPL) has been used more often with the similar efficacy of PDL.[7], [8] IPL rests on the principle of selective photothermolysis, in which thermally mediated radiation damage is confined to chosen epidermal and/or dermal pigmented targets at the cellular or tissue structural levels. [8]
Therapy affects melanin, destroy the blood vessels thereby reducing its size, induces tissue hypoxia leading to decreased cellular function. It also, induces disulphide bond disruption with subsequent remodelling of the fibres or collagenolysis following cytokine stimulation. Intense pulsed light [IPL] 400-1200 nm devices are non-laser high intensity light sources.
Intralesional steroids (Triamcinolone acetonide 10 mg/ml or 40 mg/ml with 1:1 dilution) has long been a mainstay and relatively effective [9] first-line therapy of treatment of keloids. Steroids are known to diminish collagen synthesis, reduce inflammation, decrease mucinous ground substance and inhibit collagenase inhibitors that prevent degradation of collagen, thus decreasing dermal thickening.[9] The present study was conducted to compare the efficacy of Intense pulsed light versus Intralesional Triamcinolone in the treatment of keloids and hypertrophic scar and to study adverse effects associated with them.
Materials and Methods
This single center, prospective and interventional study was conducted for duration of 2 years.
The inclusion criteria was individuals of both genders aged above 18 years age who presented to the OPD with keloids and hypertrophic scars. Pregnant, lactating females, those with active tuberculosis, psoriasis, other acute skin lesions, known case of photosensitivity, uncontrolled diabetes, cardiovascular and renal diseases were excluded from the study.
The detailed protocol was explained to the patients. Institutional ethics committee approval was acquired and written informed consent was obtained from all the patients in accordance with the principles of a Declaration of Helsinki as revisited in 2013.
Sample size-total of 60 patients were taken in the study and were divided into two groups of 30 patients each.For calculation of sample size, G*Power software was used. Alpha=α=0.05, Power = 0.80, large effect size was considered =0.8. Using G* Power software sample size of each group was found to be 30 patients.
In IPL group 590nm vascular filter was used and dose was started at 25 J/cm² and increased by 3 J/cm² in subsequent settings depending on patient’s tolerance. In second group, intralesional triamcinolone of 40 mg/ml mixed with lignocaine (1:1 dilution) was given with insulin syringe at 2 weeks interval for 5 visits. The patients were followed up at two weeks intervals until 5 visits were done and were assessed for the fate of pigmentation, pliability, height and vascularity of the lesions 15 days after each visit.
Results
Statistical analysis
Data was analysed using SPSS software version 21 and Excel sheets. Categorical variables were given in the form of frequency table. Continuous variables were given in Mean ± SD/ Median (Min, Max) form. Categorical variables were analysed by Chi square test. The obtained results are represented as the tables and graphs below.
|
Variables |
Sub Category |
ILS |
IPL |
|
Number of Subjects (%) |
|||
|
Age (years) |
<20 |
4 (13.3%) |
3 (10%) |
|
21 – 35 |
15 (50%) |
14 (46.7%) |
|
|
36 – 40 |
2 (6.7%) |
4(13.3%) |
|
|
41 – 55 |
8 (26.7%) |
6 (20%) |
|
|
56 – 70 |
0 |
3 (10%) |
|
|
>70 |
1 (3.3%) |
0 |
|
|
Mean ± SD |
32.97 ± 13.26 |
36.37 ± 13.15 |
|
|
|
Median (Min, Max) |
30 (16, 71) |
33 (14, 65) |
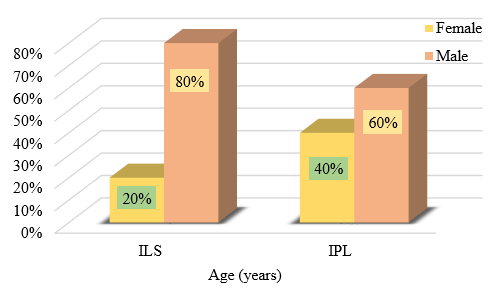
The mean of age of ILS patients was 32.97 ± 13.26 and the mean age of IPL patients was 36.37 ± 13.15. There was no significant association observed between the formation of scars and the age of the patients.([Table 1])
|
Variables |
|
ILS/IPL |
|
Number of lesions |
1 |
16 (53.3%) |
|
2 |
10 (33.3%) |
|
|
3 |
3 (10%) |
|
|
4 |
1 (3.3%) |
|
|
Site |
Patients receiving IPL |
Patients receiving ILS |
|
Chest |
5 (16.6%) |
4 (13.3%) |
|
Abdomen |
3 (10%) |
4 (13.3%) |
|
Pubic area |
4 (13.3%) |
4 (13.3%) |
|
Lower back |
2 (6.7%) |
2 (6.7%) |
|
Left forearm |
2 (6.7%) |
2 (6.7%) |
|
Left shoulder |
2 (6.7%) |
2 (6.7%) |
|
Left thigh |
2 (6.7%) |
2 (6.7%) |
|
Left arm |
1 ( 3.5 %) |
1 (3.5%) |
|
Right arm |
1 (3.5%) |
1 (3.5%) |
|
Right forearm |
2 (6.7%) |
2 (6.7%) |
|
Right shoulder |
4 (13.3%) |
4 (13.3%) |
|
Upper back |
2 (6.7%) |
2 (6.7%) |
Majority of the patients had presented with single lesions followed by two lesions. The most common sites of hypertrophic scar and keloids were chest, right shoulder and pubic area.Comparison of results between first and last visit for each parameter is as given below.
|
|
ILS-Height First Visit |
p-value |
|||
|
Flat |
<2 cm |
Total |
|||
|
Number of subjects (%) |
|||||
|
ILS-Height Fifth Visit |
<2 cm |
7 (23.33%) |
0 |
7 (23.33%) |
<0.001*C |
|
2-5 cm |
0 |
23 (76.66%) |
23 (76.66%) |
||
|
IPL-Height First Visit |
|||||
|
IPL-Height Fifth Visit |
Flat |
0 |
1 (3.33%) |
1 (3.33%) |
0.223 |
|
<2 cm |
5 (16.66%) |
15 (50%) |
20 (66.66%) |
||
|
2-5 cm |
0 |
9 (30%) |
9 (30%) |
There was a strongly significant reduction in the height of the lesions observed in ILS group between the 1st and 5th visit with the p value of <0.001 ,whereas the change in height with IPL group between the first and last sitting was not significant.
|
Vascularity |
ILS-Vascularity First Visit |
p-value |
||||
|
Normal |
Pink |
Red |
Total |
|||
|
Number of subjects (%) |
||||||
|
ILS-Vascularity Fifth Visit |
Normal |
3 (10%) |
11 (36.66%) |
0 |
14 (46.66%) |
0.072 |
|
Pink |
0 |
14 (46.66%) |
2 (6.66%) |
16 (53.33%) |
||
|
IPL-Vascularity First Visit |
||||||
|
IPL-Vascularity Fifth Visit |
Normal |
6 (20%) |
9 (30%) |
0 |
15 (50%) |
0.002 |
|
Pink |
0 |
9 (30%) |
6 (20%) |
15 (50%) |
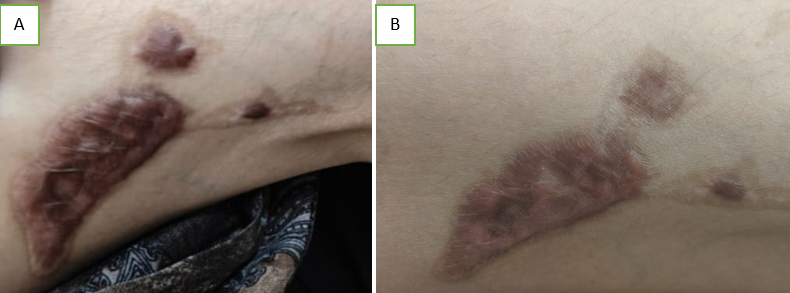
There was significant decrease in vascularity between 1st and last visit of IPL, (p Value= 0.002) but there was no significant decrease in vascularity between the first and final visit with ILS.
|
ILS-Pigmentation |
ILS-Pigmentation First Visit |
p-value |
|||
|
Normal |
Hypopigmentation |
Total |
|||
|
Number of subjects (%) |
|||||
|
ILS-Pigmentation Fifth Visit |
Normal |
8 (26.66%) |
0 |
8 (6.33%) |
0.704 |
|
Hypopigmentation |
2 (6.66%) |
20 (66.66%) |
22 (93.66) |
||
|
IPL-Pigmentation First Visit |
|||||
|
IPL-Pigmentation |
Normal |
28 (93.33%) |
0 |
28 (93.33) |
<0.001* |
|
Hypopigmentation |
0 |
2 (6.66%) |
2 (6.66%) |
28/30 (93.99%) of the study samples in IPL group had normal skin at the end of the study whereas only 8/30(26.6%) had found to be with normal skin in ILS at the last visit.66.66% of those treated with ILS developed hypopigmentation of the lesions at the end of study.
|
Pliability |
ILS-Pliability First Visit |
p-value |
|
|||
|
Supple |
Yielding |
Total |
||||
|
Number of subjects (%) |
||||||
|
ILS-Pliability Fifth Visit |
Normal |
2 (6.66%) |
0 |
2 (6.66%) |
0.015* |
|
|
Supple |
6 (20%) |
22 (73.33%) |
28 (93.33%) |
|||
|
IPL-Pliability: First visit |
||||||
|
IPL-Pliability: Fifth visit |
Normal |
5 (16.66%) |
1 (3.33%) |
0 |
6 (20%) |
p-value <0.001* |
|
Supple |
3 (10%) |
4 (13.33%) |
3 (10%) |
10 (33.33%) |
||
|
Yielding |
0 |
2 (6.66%) |
10 (33.33%) |
12 (40%) |
||
|
Firm |
0 |
0 |
2 (6.66%) |
2 (6.66%) |
Significant difference in pliability was observed between first and final visits on both IPL(p value <0.001) and ILS (p value -0.015),with IPL showing a much more significant reduction in pliability.
On analysing the degree of pliability, both ILS and IPL had significant improvement.


Discussion
On analysis, we did not find any association between the age, gender and other socio-epidemiological data with the incidence of the hypertrophic scar and keloids. Only 13.3% and 6.7% from ILS and IPL groups respectively had blunt trauma as the precipitating factor. Majority of them were symptom free and 33.3% each in both groups had presented with itching as the symptom. The clinical studies by Liu AH et al had reported that severe keloids and hypertrophic scars could be varied with sex, age, excessive scrubbing. [10] Other cross sectional and systematic analysis also have reported no sociodemographic association like the present study.[11]
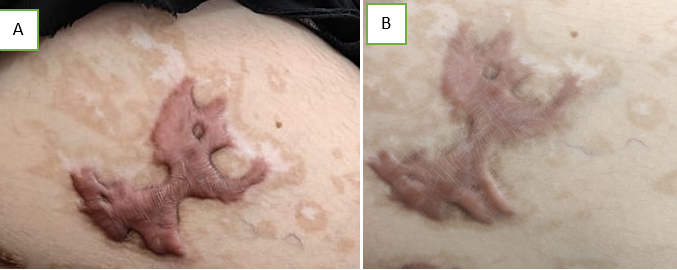
In the present study, majority of the cases presented with single lesion. Commonest sites were chest and shoulders which was consistent with the observations made by Hunasgi S et al[12] where they had discussed the same pattern of distribution.
On analysis we found that, there was no much difference in the height of the lesion between 1st visit and the 5th visit with IPL, but we observed that ILS group had significant reduction in height of the lesion between the first and fifth visit as compared to IPL. We could assess that the growth of the lesions were arrested and resolved faster with ILS than IPL. Contrary to our findings, scar thickness was significantly reduced among 10% after the first IPL session itself in the study conducted by Thanh LTV et al, 15% after the second session and>20% after the third session. Also, in contrast to our observations,[13] Li K et al found that IPL had significantly improved morphological changes in hypertrophic and keloid scars based on both subjective and objective analyses from first visit itself, but in contrast to our study where we used 590nm filter, they had used 1470 nm bare-fibre diode for the IPL.[14]
In the present study the vascularity of the lesions had significant reduction in the IPL group .Pigmentary changes were observed in both IPL and ILS group. 93.33% patients treated with IPL attained almost normal skin colour by the fifth sitting at the end of the study while 66.66%patients treated with ILS developed hypopigmentation at the end of study. Coppola MM et al [9] had discussed in their review that although ILS had shown a faster and more effective response and even though it is associated with a higher complication rate, the combination therapy of ILS with other modes of management is significantly higher than ILS alone.
Kim DY et al, a Korean study had reported that the combination therapy of IPL with corticosteroid injection not only improves the appearance of keloids and hypertrophic scars but also increases the recovery level of skin hydration status in terms of the skin barrier function than the monotherapy.[15] Similar to our outcome with ILS, Nishi N et al, who had compared ILS with cryotherapy also stated that ILS has high efficacy in management of keloids and it is aesthetically superior for exuberant scars. [16]
We can analyse that both IPL and ILS are efficacious in the management of hypertrophied scars and keloids but the duration and the improvement in the morphology are associated with the baseline morphological characteristics of the lesions which differ from individual to individual.
Conclusion
Both IPL and ILS are effective methods in the management of keloid and hypertrophic scars. ILS results in greater reduction in height of keloid and hypertrophic scars compared to IPL.IPL resulted in significant reduction of vascularity. Both IPL and ILS caused significant reduction in pliability, however the effect of IPL on improvement of pliability was superior compared to ILS. IPL also resulted in the transition of hyperpigmentation to normal skin colour, whereas with ILS the tendency to develop hypopigmentation was significantly high. We conclude that a single modality of treatment may not be as effective as a combination of both these modalities in the treatment of keloids and hypertrophic scars. Thus IPL and ILS can be combined to yield better results.
Conflicts of Interest
There are no conflicts of interest.
Source of Funding
None.
References
- GC Limandjaja, FB Niessen, RJ Scheper, S Gibbs. Hypertrophic scars and keloids: Overview of the evidence and practical guide for differentiating between these abnormal scars. Exp Dermatol 2021. [Google Scholar]
- GG Gauglitz, HC Korting, T Pavicic, T Ruzicka, MG Jeschke. Hypertrophic scarring and keloids: pathomechanisms and current and emerging treatment strategies. Mol Med 2011. [Google Scholar]
- W Lu, H Chu, X Zheng. Effects on quality of life and psychosocial wellbeing in Chinese patients with keloids. Am J Transl Res 2021. [Google Scholar]
- SW Kim. Management of keloid scars: noninvasive and invasive treatments. Arch Plast Surg 2021. [Google Scholar]
- SF Ekstein, SP Wyles, SL Moran, A Meves. Keloids: a review of therapeutic management. Int J Dermatol 2021. [Google Scholar]
- S Stephanides, S Rai, P August, J Ferguson, V Madan. Treatment of refractory keloids with pulsed dye laser alone and with rotational pulsed dye laser and intralesional corticosteroids: A retrospective case series. Laser Ther 2011. [Google Scholar]
- SP Nischwitz, DB Lumenta, S Spendel, LP Kamolz, S Shamsimeymandi, A Rezazadeh, L Téot, TA Mustoe, E Middelkoop. Minimally Invasive Technologies for Treatment of HTS and Keloids: Pulsed-Dye Laser. Textbook on Scar Management: State of the Art Management and Emerging Technologies [Internet] 2020. [Google Scholar]
- DJ Goldberg. Current trends in intense pulsed light. J Clin Aesthet Dermatol 2012. [Google Scholar]
- MM Coppola, R Salzillo, F Segreto, P Persichetti. Triamcinolone acetonide intralesional injection for the treatment of keloid scars: patient selection and perspectives. Clin Cosmet Investig Dermatol 2018. [Google Scholar] [Crossref]
- R Liu, H Xiao, R Wang, W Li, K Deng, Y Cen. Risk factors associated with the progression from keloids to severe keloids. Chinese Medical Journal 2022. [Google Scholar]
- Z Zhu, W Kong, H Wang, Y Xiao, Y Shi, L Gan. Clinical status of hospitalized keloid cases from 2013 to 2018. Burns 2018. [Google Scholar]
- S Hunasgi, A Koneru, M Vanishree, R Shamala. Keloid: A case report and review of pathophysiology and differences between keloid and hypertrophic scars. J Oral Maxillofac Pathol 2013. [Google Scholar]
- LTV Thanh, TS Quan, LV Anh, TQ Hung, NL Vuong. The Efficacy of Intense Pulsed Light in the Treatment of Keloids and Hypertrophic Scars. J Lasers Med Sci 2023. [Google Scholar] [Crossref]
- K Li, F Nicoli, C Cui, WJ Xi, A Al-Mousawi, Z Zhang. Treatment of hypertrophic scars and keloids using an intralesional 1470 nm bare-fibre diode laser: a novel efficient minimally-invasive technique. Sci Rep 2020. [Google Scholar] [Crossref]
- DY Kim, HS Park, HS Yoon, S Cho. Efficacy of IPL device combined with intralesional corticosteroid injection for the treatment of keloids and hypertrophic scars with regards to the recovery of skin barrier function: A pilot study. J Dermatolog Treat 2015. [Google Scholar]
- N Nishi, TS Rajashekar. A Comparative Study of Effectiveness of Cryotherapy with Intralesional Triamcinolone Vs Fractional CO2 Laser with Topical Betamethasone for the Treatment of Keloids. J Cutan Aesthet Surg 2022. [Google Scholar]
