- Visibility 45 Views
- Downloads 5 Downloads
- DOI 10.18231/j.ijced.2024.083
-
CrossMark
- Citation
Patchy acute effluvium in and around the donor area following FUE hair transplant and its predilection for two-day session and high graft extraction cases
- Author Details:
-
Mubashar Mashqoor Mir *
-
Sumit Sharma
-
Mona Sharma
Introduction
Follicular unit extraction (FUE) is the preferred technique of hair transplantation (HT) nowadays where follicular units (grafts) are harvested from the donor area using micro punches and implanted on to the recipient area thus exploiting the principle of donor dominance.[1] FUE technique has gained prominence in the recent years owing to its advantages including the decreased morbidity and patient care postoperatively and the absence of linear scaring seen with Follicular unit transplantation (FUT).[2] The follicular grafts are obtained in such a way so that the ratio of extracted hair with respect to the available donor hair should not exceed 1:3 in order to prevent the over extraction of hair which can give a bald look to the donor area.[3] In advanced grades of androgenetic alopecia (AGA), higher number of grafts are needed to adequately cover the recipient area often requiring the surgery to extend beyond single day. [4] The high demand of required grafts in advanced grades of AGA may lead to close extraction of grafts. Moreover, heavy extraction of donor area may lead to vascular compromise in the donor and peri-donor area follicles which is believed to contribute towards local post-procedure complication known as post transplant acute donor effluvium (ADE). [5] ADE has been described in the literature as sudden onset, patchy non-scarring alopecia of the scalp especially in and around the donor area of the scalp. [6] We propose it should be preferably called acute donor and peri-donor effluvium (ADPE) as the hair loss often extends on to the adjoining area of donor scalp including the occipito-parietal and occipito-temporal regions [[Figure 1]].
So far, very little data is available regarding ADE however with the expanding scope of FUE lesser seen complications of FUE HT including ADE are seen more nowadays. [7] The existing literature exploring the aetiology and clinical presentation of acute post transplant effluvium is inadequate. Hence this study was thus conducted to describe the clinical presentation of such cases and to study its association with clinic epidemiological factors like the age, co morbidities, personal habits, duration of surgery and number of grafts harvested. The correlation of ADE severity with the extent of graft extraction was also assessed.
Materials and Methods
It was a retrospective study undertaken at Dermawave Skin Laser and Hair Transplant Centre, Panipat (India). The study was completed within the period three months from October 2022 to December 2022. Clinical records and photographs of patients who had undergone hair transplant from the centre in last 3 years and experienced post transplant acute effluvium of the donor and peri-donor area were screened. A total of 30 such cases of androgenetic alopecia that underwent FUE hair transplant and experienced acute, non scarring and patchy hair loss of the donor and peri-donor scalp within 3 weeks of HT and diagnosed as acute donor effluvium by the dermatologist after fulfilling the selection criteria were selected for the study. Patients with non uniform extraction of the donor area of scalp, those having inadequate data available and those who did not consent for participation in the study were excluded. Relevant data was compiled in the form of a proforma filled by the researchers which included demographic data, history, clinical findings, procedure and follow up notes along with photographic record. History regarding age, co morbid conditions like diabetes and hypertension, personal habits like smoking and alcohol consumption were recorded. Clinical data regarding grade of androgenetic alopecia (AGA) severity.,[8] no of grafts extracted, duration of surgery in days was obtained and recorded. Follow up data from clinical notes and photographic findings were also recorded. Severity of the patchy hair loss was assesed using Severity of Alopecia Tool (SALT) score. [9]
Statistical analysis
Data was entered and analysed using Microsoft Excel and Statistical Product and Service Solutions (SPSS 24.0). Numerical data was calculated in the form of mean, standard deviation and categorical data as frequencies and proportions. Correlation analysis was done using spearman correlation coefficient. Findings with p value of <0.05 was taken as significant.
Results
The study included 30 subjects, age of patients ranged from 27 to 48 years with mean age of 33.9 years (standard deviation 5.4 years). All the patients were male. On studying the associated co morbidities, it was found that around 1 out of 30 cases had diabetes and 3 had hypertension; however both conditions were under permissible levels at the time of surgery. With regards to personal habits, 5(16.6%) were smokers and 7(23.3%) out of 30 were having history of alcohol consumption. Severity of hair loss occurring due to acute donor area effluvium was calculated using the SALT score. The maximum SALT score obtained was 19 in our study. An arbitrary categorisation was made among cases having SALT score less than 10 versus those having SALT score more than 10 for the sake of comparison and to understand the distribution of cases. It was seen that 18 (60.0%) of our cases when graded as per SALT scoring had a score of less than 10. On the other hand 12(40.0%) of cases had a SALT score of more than 10. Most of the cases presenting with ADE had higher grades of AGA. Around 26(86.7%) had AGA of grade 5 and above while only 4(13.3%) had lower than grade 5 AGA [Table 1].
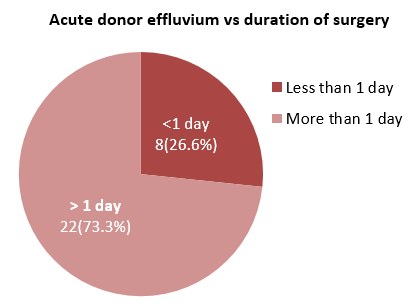
As far as the total duration in days of hair transplant surgery was concerned, it was seen that majority 22(73.3%) of the cases of acute donor effluvium comprised of those where the hair transplant surgery lasted for more than one day. Only 8(26.7%) cases of ADE had history cases of single day hair transplant. The maximum duration of surgery in all our cases did not exceed 2 days [[Figure 2]].
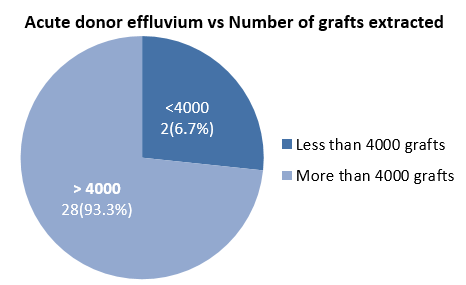
On assessing the occurrence of acute donor effluvium with regards to the number of grafts extracted from the donor area of scalp it was seen that 28(93.3%) cases of acute donor area effluvium had intra operative graft extraction of more than 4000, whereas only 2(6.7%) of the cases had scalp donor area extraction of less than 4000 grafts [[Figure 3]].
Correlation analysis was also conducted in our study to assess the relationship of severity of acute donor effluvium (SALT score) with number of total scalp hair extracted. It was found that there was a significant correlation between the severity of hair loss in ADE and the number of total scalp graft extracted. The correlation level was strong with ‘r’ value being 0.657 and ‘p’ value being 0.024.
|
Feature |
N (%) |
|
Co-morbidities |
|
|
Diabetes |
1 (3.3%) |
|
Hypertension |
3 (10.0%) |
|
Personal habits |
|
|
Smoking |
5(16.6%) |
|
Alcohol |
7(23.3%) |
|
Grade of AGA |
|
|
Grade V or more |
26(86.7%) |
|
Less than Grade V |
4(13.3%) |
|
Duration of surgery |
|
|
One day |
8(26.7%) |
|
Two day |
22(73.3%) |
|
SALT score |
|
|
<10 |
18 (60.0%) |
|
>10 |
12(40.0%) |
|
No of grafts extracted |
|
|
Less than 4000 |
2(6.7%) |
|
More than 4000 |
28(93.3%) |



Discussion
Hair transplant has witnessed a huge leap of advancement with the introduction of FUE technique as it offers better cosmetic appearance and less intra and post operative complications.10 However, FUE is not totally devoid of complications and has its own limitations which include local pinpoint scarring from the donor area, depletion of the donor site, epithelial cyst formation, and donor area acute effluvium. [7] Advancement in the skill and technique has pushed the boundaries of FUE HT and has lead to taking up higher grades of baldness for surgery. Increased demand of grafts for covering larger areas of baldness has led to longer sessions of hair transplant exceeding the conventional single day session. On the other hand there has also been an increase in the amount of graft harvesting in single day sessions giving rise to the phenomenon of mega and giga session hair transplantation.11 With the advancements and increased adoption of FUE hair transplant some lesser known complications have come into the fore light. One such phenomenon seen more often nowadays is the acute patchy and non scarring alopecia seen in and around the donor area of the scalp within the first 2 to 3 weeks of FUE HT known as acute donor effluvium. [7] Some studies having described a similar phenomenon post transplant as telogen effluvium. [10] However, in our experience, we have observed it to develop in most cases even before the patient comes back for the first scalp washing on the 7th to 10th day post transplant [[Figure 4]]. We believe that due to such short interval post transplant it can well be described as anagen effluvium caused due to sudden and transient ischemic insult to germinal cells of the hair. Since the hair fall occurs within few days or weeks post transplant, much before the time required for the hair to enter the telogen and exogen phase such phenomenon can only be described as anagen effluvium. Some studies have advocated the occurrence of same phenomenon in cases of post FUE HT and after therapeutic scalp surgeries. [6], [7], [8], [9], [11], [12], [10], [13] Fortunately, in most cases the hair loss is temporary and the recovery usually occurs within 3-4 months [[Figure 5]]. [14] In our study we found out that a large proportion of patients who suffered from acute donor effluvium were those having advanced grades of AGA (≥Grade 5 in 86.7%) or those in which the surgery was completed in two day session (73.3%). It was perhaps because of the increased requirement of grafts from the donor area needed to cover larger areas of baldness which resulted in a longer time of surgery. Most of the cases which required two day sessions were having advanced grades of androgenetic alopecia and thus had high graft requirement to cover larger recipient areas. More often than not, this leads to more aggressive graft extraction including the utilisation of the extended donor area. This was further validated from the fact that in our study majority of patients i.e. 28(93.3%) who had post transplant donor effluvium had scalp graft extraction of more than 4000 grafts. Since scoring of each follicular unit contributes to the trauma imparted to the donor scalp, in such advanced cases the cumulative trauma is more and widespread. We hypothesise that cumulative trauma to the donor scalp contributes in two different ways resulting in acute donor effluvium. On one hand it contributes by causing extensive vascular disruption leading to hypoxic tissue insult to the donor and peri-donor area. Similar phenomenon of donor effluvium was seen previously in Follicular Unit Transplantation (FUT) which was attributed to the vascular damage caused during strip excision from the donor area. [15] On the other hand, inflammation and oedema which follows as a response to the high cumulative trauma itself causes tissue ischemia by causing external vaso-compression and impairing the local vascular and lymphatic supply. Perhaps this explains the improvement seen with the use of intralesional triamcinolone by some authors in acute donor effluvium due to its anti-inflammatory effect. [6]
The higher incidence of acute donor hair loss in two day sessions can also be explained from the fact that two day surgery requires multiple injections of adrenaline containing tumescent anaesthesia which may have contributed towards prolonged vasoconstriction and resultant tissue hypoxia of the donor and peri-donor scalp. We also tried to corroborate if amount of extraction done from the donor area had an effect on the severity of hair loss seen in acute donor effluvium using SALT scoring. It was seen that donor graft extraction had a strong and direct correlation with the amount of hair loss in acute donor effluvium.
Limitation
Limitations of our study included the absence of a control group, smaller sample size and that no intervention was instituted to study the effect of drugs like minoxidil or triamcinolone on acute donor effluvium. Use of trichoscopic and histopathological studies can help us better understand this phenomenon in future studies.
Conclusion
We concluded that longer two day sessions of FUE hair transplant along with high graft extraction from the donor scalp often undertaken in advanced grade of AGA were two most common incriminating factors observed in our study which contributed to the causation of acute donor site effluvium. Hair transplant surgeons should be careful in observing such cases for possibility of acute donor effluvium and these patients need to be counselled in advance regarding the possibility of such phenomenon.
Source of Funding
None.
Conflict of Interest
None.
References
- N Karaçal, M Uraloğlu, T Dindar, M Livaoğlu. Necrosis of the donor site after hair restoration with follicular unit extraction (FUE): a case report. J Plast Reconstr Aesthet Surg 2011. [Google Scholar]
- A Dua, K Dua. Follicular unit extraction hair transplant. J Cutan Aesthet Surg 2010. [Google Scholar]
- MH Mohmand, M Ahmad. Effect of Follicular Unit Extraction on the Donor Area. World J Plast Surg 2018. [Google Scholar]
- K Chouhan, G Roga, A Kumar, J Gupta. Approach to Hair Transplantation in Advanced Grade Baldness by Follicular Unit Extraction: A Retrospective Analysis of 820 Cases. J Cutan Aesthet Surg 2019. [Google Scholar]
- AS Kerure, SM Agrawal, R Dhurat, A Ginzburg. Donor Area Acute Effluvium following Follicular Unit Extraction-Trichoscopic Simulator of Alopecia Areata: Series of Four Cases. J Cutan Aesthet Surg 2020. [Google Scholar]
- A Gómez-Zubiaur, P García-Morrás, Á Hermosa-Gelbard, S Vañó-Galván. Localized Telogen Effluvium of the Donor Area After Hair Transplant Surgery in 12 Patients. Dermatol Surg 2021. [Google Scholar]
- AS Kerure, N Patwardhan. Complications in Hair Transplantation. J Cutan Aesthet Surg 2018. [Google Scholar]
- NP Khumalo, F Gumedze. The adapted classification of male pattern hair loss improves reliability. Dermatology 2012. [Google Scholar] [Crossref]
- EA Olsen, MK Hordinsky, VH Price, JL Roberts, J Shapiro, D Canfield. Price VH et al Alopecia areata investigational assessment guidelines: part II. J Am Acad Dermatol 2004. [Google Scholar]
- SH Loh, BL Lew, WY Sim. Localized Telogen Effluvium Following Hair Transplantation. Ann Dermatol 2018. [Google Scholar]
- M Khanna. Hair transplantation surgery. Indian J Plast Surg 2008. [Google Scholar]
- R M Bernstein, W R Rassman, K W Anderson. Follicular unit extraction mega sessions: evolution of a technique. Hair Transplant Forum Int 2004. [Google Scholar]
- LA Contin, LDN Santos, IJN Pereira, VB Rocha. Anagen Effluvium after Therapeutic Scalp Surgery: Unreported Phenomenon. Skin Appendage Disord 2021. [Google Scholar]
- A Garg, S Garg, V Mysore. Hair Transplantation. Donor Area Complications of Strip Harvesting 2016. [Google Scholar]
- K Dua, S Uprety, A Dua. Donor Harvesting: Strip Dissection. J Cutan Aesthet Surg 2018. [Google Scholar]
