- Visibility 241 Views
- Downloads 20 Downloads
- DOI 10.18231/j.ijced.2025.008
-
CrossMark
- Citation
Rise in syphilis: Time to turn the tide
Introduction
Syphilis is a curable and preventable sexually transmitted infection (STI. In India, the prevalence of STIs such as syphilis, gonorrhea, and chlamydia has been reported to range from 0% to 3.9%.[1] Syphilis is a sexually and vertically transmitted infection caused by the spirochete Treponema pallidum subspecies pallidum. It remains one of the "great imitators" due to its diverse clinical manifestations. The epidemiological profile of syphilis varies by region, influenced by ethnographic, demographic, socio-economic, and health-related factors.[2] The clinical presentation of syphilis reflects the interaction between the pathogen, transmission behaviors, and the effectiveness of preventive and control measures. [2]
The incidence and prevalence of syphilis significantly declined following the introduction of HIV prevention programs, the advent of penicillin, and improvements in diagnostic and therapeutic facilities. In 2000 and 2001, the national rate of reported primary and secondary syphilis cases in India was 2.1 per 100,000 population. [2] Although syphilis was once thought to be on the verge of elimination in India, recent clinical data suggest its re-emergence as a public health concern.
In recent decades, syphilis cases have surged due to multiple factors, including the HIV epidemic, global travel, an increase in men having sex with men (MSM), and high-risk groups such as unmarried youth. The interplay with HIV co-infection, changes in sexual behavior due to the availability of effective antiretroviral therapy, and the ease of finding sexual partners through internet and mobile dating applications have added complexity to the epidemiology of syphilis and its control. [3]
Syphilis is often misdiagnosed and mistreated, partly because many physicians are unfamiliar with its varied clinical presentations, a consequence of the decline in cases in previous years. Additionally, the infection’s ability to mimic other conditions can lead to diagnostic challenges, potentially contributing to its further spread. This study reports confirmed syphilis cases diagnosed over a one-year period in a tertiary care hospital in western Maharashtra, India.
Materials and Methods
A prospective observational study was conducted from December 2022 to November 2023 at the STI Clinic of the tertiary care teaching hospital in Pune, Maharashtra, after obtaining approval from the Institute’s Ethics Committee. Written informed consent was obtained from all enrolled patients, and clinical photographs were taken for documentation and further analysis. All procedures were conducted in accordance with the Declaration of Helsinki guidelines for medical research involving human subjects.
All patients diagnosed with syphilis during the study period at the STI clinic were enrolled. Inclusion criteria included patients of both sexes, aged 18 years or older, who provided written informed consent and had a confirmed syphilis diagnosis. Exclusion criteria included patients unwilling to provide consent or those with incomplete medical records.
Demographic details such as age, gender, occupation, and sexual behavior were collected along with detailed clinical histories. Syphilis diagnosis was based on a combination of clinical history, physical examination, and laboratory confirmation. Clinical findings, including the stage of syphilis (primary, secondary, latent, or tertiary), were documented. Clinical photographs were obtained with patient consent to record cutaneous and mucosal manifestations. The diagnosis was confirmed if the patient presented with a Venereal Disease Research Laboratory (VDRL) titre of 1:8 or greater. In addition, Treponema pallidum hemagglutination assay (TPHA) was performed to corroborate the diagnosis. Other relevant serological tests included screening for hepatitis B surface antigen (HBsAg), anti-hepatitis C virus (HCV) antibodies, and HIV using ELISA. Appropriate treatment with Injection Benzathine Penicillin 2.4M IU was administered according to the stage of syphilis.
The collected data were entered into Microsoft Excel 2010 for analysis. Descriptive statistics, such as mean, median, and frequency, were used to describe the demographic and clinical characteristics of the patients. Categorical data were presented as frequencies and percentages. Continuous data were presented as means and SD or medians with interquartile ranges, depending on the data distribution. The association between co-infections and syphilis stages was assessed using appropriate statistical tests (Chi-square test for categorical variables). A p-value of less than 0.05 was considered statistically significant.
Confidentiality was maintained throughout the study by anonymizing patient data during data entry and analysis. The study posed minimal risk to participants, and ethical principles were adhered to at all stages of research conduct.
Results
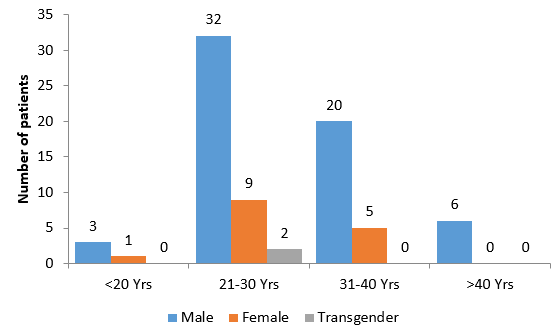
A total of 78 confirmed cases of syphilis, accounting for 4.7% of the 1660 STI cases reported during the study period, were enrolled in the study. All patients were referred to our center for treatment from various clinics and hospitals. None of the patients had received prior treatment elsewhere. The demographic distribution of these cases indicates that 61 (78.2%) were male, 15 (19.2%) were female, and 2 (2.6%) were transgender. The majority of cases were young adults between the ages of 21-30 years (43; 55.1%), with the youngest patient being 16 days infant and the oldest 55 years old ([Figure 1]). Regarding marital status, 51 (65.4%) of the patients were married, and 27 (34.6%) were unmarried. In terms of educational background, 33 (42.3%) were graduates, 39 (50%) had completed higher secondary or less, and 6 (7.7%) had only primary education ([Table 1]).
|
Demographic Parameter |
Category |
Number of Cases (n=78) |
Percentage (%) |
|
Sex |
Male |
61 |
78.2% |
|
Female |
15 |
19.2% |
|
|
Transgender |
2 |
2.6% |
|
|
Age Group |
<=20 years |
4 |
5.1% |
|
21-30 years |
43 |
55.1% |
|
|
31-40 years |
25 |
32.1% |
|
|
>40 years |
6 |
7.7% |
|
|
Marital Status |
Married |
51 |
65.4% |
|
Unmarried |
27 |
34.6% |
|
|
Educational Background |
Graduate |
33 |
42.3% |
|
Higher Secondary or Less |
39 |
50.0% |
|
|
Primary Education |
6 |
7.7% |
In terms of sexual behavior, 52 (67.5%) patients reported being in polygamous relationships, and the vast majority of the cases (67; 87.0%) did not use condoms regularly. The sexual orientation of the patients was primarily heterosexual in 51 (66.2%) cases, while 6 (7.8%) identified as homosexual and 20 (26.0%) as bisexual. Different modes of sexual intercourse were practiced, with peno-vaginal intercourse being the most common (69; 89.6%, followed by peno-oral (34; 44.2%) and peno-anal (29; 37.7%) intercourse, all without condom usage ([Table 2]). The details of clinical settings in which latent syphilis was diagnosed are presented in [Table 3].
|
Sexual Behavior Parameter |
Category |
Number of Cases (n=77) |
Percentage (%) |
|
Relationship Type |
Polygamous |
52 |
67.5% |
|
Monogamous |
25 |
32.5% |
|
|
Condom Usage |
No Regular Condom Use |
67 |
87.0% |
|
Regular Condom Use |
10 |
13.0% |
|
|
Sexual Orientation |
Heterosexual |
51 |
66.2% |
|
Homosexual |
6 |
7.8% |
|
|
Bisexual |
20 |
26.0% |
|
|
Mode of Sexual Intercourse |
Peno-Vaginal |
69 |
89.6% |
|
Peno-Oral |
34 |
44.2% |
|
|
Peno-Anal |
29 |
37.7% |
The [Table 3] outlines various clinical settings where syphilis was diagnosed. A total of 78 cases were reported, including 61 in males, 16 in females, and 2 in transgender individuals. The largest number of cases were found in 31 symptomatic males out of which 7 had genital chancre, 17 presented with asymptomatic rash of secondary syphilis whereas remaining 6 had both. One symptomatic female presented with genital chancre. During pre-operative routine tests or voluntary health check-ups 15 males, 1 female, and 2 transgender were detected. During antenatal checkups, 10 out of 11 cases were in females, as syphilis screening is a routine part of prenatal care. The one male listed in this category was the husband of a female diagnosed during her antenatal visit. Additionally, 7 cases were found when a spouse tested positive, with 6 of these in males. Following HIV detection, 6 syphilis cases were identified, primarily among males (5 cases). One case of congenital syphilis with four time lower VDRL titre than mother without any stigmata of congenital syphilis was detected. Other settings included (1 each) genital warts, herpes genitalis, and a male diagnosed during an overseas pre-employment medical investigation. Overall, syphilis diagnoses were predominantly in males, particularly in symptomatic and routine testing contexts.
|
Clinical Setting at Diagnosis |
|
Sex |
Total |
|||
|
|
Male |
Female |
Transgender |
|||
|
Symptomatic |
Genital chancre |
7 |
1 |
0 |
8 |
31 |
|
Asymptomatic rash of secondary syphilis |
17 |
0 |
0 |
17 |
||
|
Both |
6 |
0 |
0 |
6 |
||
|
Routine test |
15 |
1 |
2 |
18 |
||
|
Antenatal checkup |
1 |
10 |
0 |
11 |
||
|
Spouse Positive |
6 |
1 |
0 |
7 |
||
|
After HIV detection |
5 |
1 |
0 |
6 |
||
|
Genital Warts |
1 |
0 |
0 |
1 |
||
|
Herpes genitals |
0 |
1 |
0 |
1 |
||
|
Baby born to syphilitic mother |
0 |
1 |
0 |
1 |
||
|
Investigation for VISA |
1 |
0 |
0 |
1 |
Co-infection with HIV was identified in 26 (33.3%) patients, of which 6 were newly diagnosed during the course of the study, while the remaining 20 were already on treatment for HIV. The VDRL titres of the patients varied, with most cases having titres ranging between 1:16 and 1:64 ([Table 2]). Symptomatic patients had titres ranging from 1:16 to 1:128. 11 (14.1%) pregnant women tested positive for VDRL during routine antenatal check-ups, and their diagnoses were confirmed by TPHA. All of them were in the late latent stage of syphilis ([Table 4]).
|
VDRL titre |
n |
% |
|
1:08 |
5 |
6.41% |
|
1:16 |
23 |
29.49% |
|
1:32 |
20 |
25.64% |
|
1:64 |
18 |
23.08% |
|
1:128 |
3 |
3.85% |
|
1:320 |
3 |
3.85% |
|
1:640 |
6 |
7.69% |
The clinical staging of the patients revealed that 1 (1.28%) patients had both primary and secondary syphilis, 9 (11.54%) had primary syphilis, 14 (17.95%) had secondary syphilis, 3 (3.85%) were in the early latent stage, and 51 (65.38%) were in the late latent stage of syphilis ([Table 5]).
|
Clinical Stage |
n |
% |
|
Both Primary and Secondary Syphilis |
1 |
1.28% |
|
Primary Syphilis |
9 |
11.54% |
|
Secondary Syphilis |
14 |
17.95% |
|
Early Latent Syphilis |
3 |
3.85% |
|
Late Latent Syphilis |
51 |
65.38% |
Discussion
The Indian national program data has indicated a steady decline in the prevalence of syphilis among patients with STIs, pregnant women, and high-risk groups.[4] According to national HIV program data, syphilis prevalence among patients attending STI clinics decreased from 0.5% in 2014-2015 to 0.4% in 2016-2017.[4] Similarly, syphilis prevalence among pregnant women decreased from 0.23% in 2014-2015 to 0.15% in 2015-2016, before rising slightly to 0.16% in 2016-2017.[5], [6] Data from the Maharashtra State AIDS Control Society (MSACS) showed syphilis seropositivity rates of 0.49% among STI attendees, 0.02% among pregnant women, and 5.28% among transgender individuals in 2022-2023.[7]
Globally, syphilis remains a significant public health issue. In 2020, WHO estimated that 7.1 million adults aged 15-49 acquired syphilis.[8] Alarming rises in STI prevalence, particularly in men who have sex with men (MSM) in the U.S. and other developed countries, indicate the need for constant vigilance.[9] At our designated STI clinic, syphilis cases showed an increasing trend, with 7 cases in 2021-2022, 13 in 2022-2023, and 37 in 2023-2024. The lack of robust surveillance systems in India makes it difficult to have an accurate understanding of the syphilis epidemic. The stigma attached to STDs, poor attendance at STD clinics, and lack of reporting are major barriers to assessing the actual prevalence. This underscores the need for syphilis to be a notifiable disease to strengthen the surveillance and control efforts. [10]
In the current study, 78 cases of syphilis were diagnosed within 22 months, similar to findings by Kulkarni et al. and Gosavi et al., raising concern about the re-emergence of syphilis. [11], [12] Male preponderance (73.33%) observed in the study aligns with findings by Jain et al. and Gupta et al., likely reflecting higher-risk behaviors among men and their tendency to seek medical advice earlier. Cultural restrictions and the often asymptomatic nature of syphilis in women may contribute to underrepresentation among females. [13], [14]
Most patients in our study were young adults aged 21-30, which highlights the early onset of sexual activity and high-risk sexual behavior among the youth. This finding suggests the need to target both married and unmarried individuals in STI prevention efforts, as cases were not confined to traditional high-risk groups (e.g., MSM, sex workers). Changing social norms around premarital sex and same-sex behavior further complicate efforts to reduce syphilis transmission. [15]
Contrary to the traditional belief that lower education is associated with higher STI prevalence, most patients in our study were literate, with the majority having higher education. This suggests that increased awareness and treatment-seeking behavior may be contributing factors to the higher detection of syphilis among educated individuals, as seen in studies by Gosavi et al., Jain et al. and Shah et al. [12], [13], [16]
HIV co-infection was observed in 26 patients, which exacerbates the public health implications. Studies indicate that syphilis prevalence is significantly higher in HIV-positive individuals than in HIV-negative ones. While biomedical interventions like antiretroviral therapy help control the HIV epidemic, they do not provide protection against other STIs. This emphasizes the importance of continued behavioral interventions and robust Information, Education, and Communication (IEC) activities to curb the spread of syphilis. [9], [10]
Eleven women in the study were diagnosed with syphilis during routine antenatal checkups, underscoring the importance of strengthening antenatal syphilis screening and ensuring appropriate treatment and follow-up for positive cases. Additionally, our findings show a rise in syphilis cases, echoing trends seen by Thokchom et al. and Kamat et al. Routine serological screenings, such as VDRL, have helped identify these latent cases, highlighting the need for early diagnosis and treatment in asymptomatic patients. [17], [18]
Syphilis control requires a multifaceted approach that includes expanding awareness, testing, and treatment interventions. Existing prevention strategies should be enhanced, including efforts to increase testing and provide early treatment. Community-based initiatives and the use of rapid point-of-care testing, such as combined HIV and syphilis testing, could also play a significant role in syphilis control. [19]
In conclusion, controlling the current syphilis resurgence requires a comprehensive strategy that includes consistent and correct condom use, regular testing, behavioral interventions, and effective treatment. A tailored approach using evidence-based prevention methods and emerging biomedical tools, adapted to current social and epidemiological contexts, offers the best opportunity to curtail the spread of syphilis.
Conclusion
This study highlights the critical need for improved surveillance among both the general population and high-risk groups to effectively diagnose latent syphilis and reduce transmission rates. Strengthening sex education, promoting safe sex practices, and implementing cost-effective rapid point-of-care tests are essential strategies. Furthermore, ensuring appropriate and adequate management of syphilis cases, along with targeted campaigns aimed at high-risk groups such as men who have sex with men (MSM), female sex workers (FSW), and people living with HIV (PLHIV), could play a pivotal role in curbing the resurgence of syphilis.
Study Limitations
The study was limited to a single center, and the relatively small sample size may affect the generalizability of the findings. Further multicenter studies with larger populations are required to validate the results.
Conflict of Interest
The authors declare no conflict of interest.
Source of Funding
No external funding was received for this study.
References
- P Haldar, G Morineau, A Das, S Mehendale. A surveillance model for sexually transmitted infections in India. Indian J Public Health 2015. [Google Scholar]
- DM Thappa, S Kaimal. Sexually transmitted infections in India: current status (Except human immunodeficiency virus/acquired immunodeficiency syndromE). Indian J Dermatol 2007. [Google Scholar]
- G Spiteri, M Unemo, O Mårdh, AJ Amato-Gauci. The resurgence of syphilis in high-income countries in the 2000s: a focus on Europe. Epidemiol Infect 2019. [Google Scholar] [Crossref]
- . National AIDS Control Organization. Ministry of Health and Family Welfare, Government of India; 2016. (Annual report 2016-17). 2016. [Google Scholar]
- . National AIDS Control Organization. Ministry of Health and Family Welfare, Government of India; 2014. (Annual report 2014-15). . [Google Scholar]
- . National AIDS Control Organization. Ministry of Health and Family Welfare, Government of India; 2014. (Annual report 2014-15). . [Google Scholar]
- . Sankalak: Status of National AIDS and STD Response (Fifth edition, 2023). New Delhi, NACO, Ministry of Health and Family Welfare, Government of India. National AIDS Control Organization. . [Google Scholar]
- . Centers for Disease Control and Prevention. Reported STDs in the United States 2015 National Data for Chlamydia, Gonorrhea, and Syphilis. Centers for Disease Control and Prevention; October, 2016. Centers for Disease Control and Prevention. . [Google Scholar]
- M Unemo, CS Bradshaw, JS Hocking, HJC De Vries, SC Francis, D Mabey. Sexually transmitted infections: challenges ahead. Lancet Infect Dis 2017. [Google Scholar]
- VK Desai, JK Kosambiya, HG Thakor, DD Umrigar, BR Khandwala, KK Bhuyan. Prevalence of sexually transmitted infections and performance of STI syndromes against aetiological diagnosis, in female sex workers of red light area in. Sex Transm Infect 2003. [Google Scholar]
- V Kulkarni, R Parchure, S Darak. Let’s not let the guard down! - Early indications of syphilis resurgence?. Indian J Dermatol Venereol Leprol 2019. [Google Scholar]
- AP Gosavi, RB Chavan, A Bandhade, DR Kundale. Clinicodemographic profile of syphilis with rising trends at a tertiary care hospital: The tip of the iceberg. Indian J Sex Transm Dis AIDS 2021. [Google Scholar]
- A Jain, V Mendiratta, R Chander. Current status of acquired syphilis: A hospital-based 5-year study. Indian J Sex Transm Dis AIDS 2012. [Google Scholar]
- M Gupta, GK Verma, R Sharma, M Sankhyan, R Rattan, AK Negi. The Changing Trend of Syphilis: Is It a Sign of Impending Epidemic?. Indian J Dermatol 2023. [Google Scholar]
- S Jejeebhoy, R Acharya. Adolescents in Rajasthan 2012: Changing situation and needs." New Delhi: Population Council.. . [Google Scholar] [Crossref]
- BJ Shah, DR Karia, CL Pawara. Syphilis: Is it making resurgence?. Indian J Sex Transm Dis AIDS 2015. [Google Scholar]
- N Thokchom, B Meka, L Kongbam, S Mrudula, E Salam, T Ananto. Syphilis on the rise-a retrospective study at a tertiary care hospital in Northeast India. Int J Res Dermatol 2021. [Google Scholar]
- S Kamat, A Vaghasia, J Dharmender, KG Kansara, BJ Shah. Syphilis: Is it Back with a Bang?. Indian Dermatol Online J 2024. [Google Scholar]
- TA Peterman, BW Furness. Public Health Interventions to Control Syphilis. Sex Health 2015. [Google Scholar]
